Mon, Nov 24, 2025
[Archive]
Volume 2, Issue 4 (Summer 2024)
CPR 2024, 2(4): 241-250 |
Back to browse issues page
Ethics code: IR.MUBABOL.HRI.REC.1402.019
Clinical trials code: IR.MUBABOL.HRI.REC.1402.019
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadi Daniali S, Tirgar A, Pourhadi S, Greaili Z. Association of Sleep Quality and Sleepiness With Cognitive Failures among Iranian Medical Students. CPR 2024; 2 (4) :241-250
URL: http://cpr.mazums.ac.ir/article-1-138-en.html
URL: http://cpr.mazums.ac.ir/article-1-138-en.html
Mobility Impairment Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran.
Full-Text [PDF 694 kb]
(144 Downloads)
| Abstract (HTML) (103 Views)
Full-Text: (27 Views)
Introduction
Sleep is an essential component of physical and mental health, and is crucial for learning, strengthening memory, efficient consolidation of knowledge, and acquiring desired skills [1]. There is a growing body of evidence that good sleep is important for optimal neurocognitive and psychomotor function in humans [1, 2]. Sleep has a profound impact on mental integration and, consequently, on cognitive functions. Insufficient sleep, on the other hand, causes the dissociation of consciousness, impaired attention, and delayed cognitive functions [3].
According to past studies, one of the major causes of accidents in work environments is cognitive error. Many people have had the experience that their behavior and thoughts change from time to time, or are involuntary and unwanted. These behaviors range from simple forgetfulness to functional impairments such as dropping tools or equipment during work. Donald Broadbent in 1982 called such errors “cognitive failures,” which is similar to the term “slips” used by Reason. According to him, slips can be classified into three general forms: slips in attention (failures in understanding), slips in memory (failures related to information retrieval), and slips in motor actions (unintentional actions or slips of action) [4]. Attention to these cognitive failures through a scientific study can make them less likely to occur in work environments [5]. Given the relative and inconclusive scientific evidence regarding the relationship between sleep quality and cognitive performance, the role of sleep in cognitive function has garnered increasing attention in neuroscience and sleep-related research over the past few decades [6-8].
Poor sleep quality and sleep deprivation are very common among medical students due to constant stress and anxiety caused by heavy curriculum and course content, frequent exams, fear of not achieving desired results [9], hospital work shifts, and long hours of study late at night [10]. Although the most important consequences are increased risk of burnout, psychoactive substance use, anxiety, and depression [10] in medical students, the impact on cognitive functions and academic performance, and ultimately the quality of care, is also conceivable [8]. The results of a study on medical and non-medical students in 2024 showed that most of them had a sleep duration of less than 7 hours, and students who had high sleep quality had good academic performance [11]. Another study on clinical-year medical students reported that poor sleep quality had a negative impact on grade point average and academic performance, creating a vicious cycle [9]. Although no definitive results were found regarding the association of poor sleep quality with the incidence of medical errors among medical students, studies in other occupational groups have shown that poor sleep quality can have a detrimental effect on a broad range of cognitive functions, including decision-making, problem-solving, creative thinking, memory, learning, attention, and reasoning in employees. For example, a study has shown that poor sleep quality can lead to reduced safety behaviors and an increased risk of road traffic accidents [12]. Therefore, given the importance and sensitivity of the subject and the lack of related studies among medical students in Iran, we aimed to investigate the relationship of sleep quality and sleepiness with the occurrence of cognitive failures in Iranian medical students.
Materials and Methods
This is a cross-sectional study that was conducted on medical students in internship and externship courses at Babol University of Medical Sciences (BUMS) in 2023. The required sample size was estimated to be 187, based on previous research [13] and using the formula, by considering the correlation coefficient between sleep quality and cognitive performance (r=0.26), a test power of 95% and a significance level of 0.05. However, considering a 15% possibility of sample dropout, the sample size increased to 214. Participants were selected using a convenience sampling method. The criteria for entering the study included at least 1 month of study in the internship and apprenticeship courses, willingness to participate in the study, and fully answering the questions. The exclusion criteria were the uptake of sleeping pills prescribed for insomnia and sleep disorders (e.g. diazepam, oxazepam, clonazepam, lorazepam, flurazepam, chlordiazepoxide, zolpidem, and melatonin), a history of sleep disorders before entering the educational courses, and not responding completely or incorrectly to questions.
The Pittsburgh sleep quality index (PSQI), Karolinska sleepiness scale (KSS), and cognitive failure questionnaire (CFQ) were administered to participants and were collected after two days. The PSQI has 19 items and 7 subscales. The total score ranges from 0 to 21; a global scale score of ≥5 indicates poor sleep quality, while a score of <5 shows adequate sleep quality. Buysse et al. [14] reported a Cronbach’s α value of 0.83 for the internal consistency of PSQI [14]. In Iran, Sheikhinasb et al. [15] reported a Cronbach’s α and split-half reliability of 0.81 and 0.78, respectively [15]. In our study, Cronbach’s α was calculated to be 0.84. The KSS is a 9-level scale, with values 1-5 indicating a desirable level of alertness and values 6-9 indicating an undesirable level of alertness. The score of this scale is correlated with electroencephalographic results and behavioral and executive test variables, indicating its high validity in measuring sleepiness [16-18]. The content validity ratio and content validity index for the Persian version of this questionnaire were reported to be 0.86 and 0.81, respectively [18]. In our study, Cronbach’s α was calculated to be 0.87. The CFQ has 25 questions to measure everyday failures in the areas of perception, memory, and motor function. The total score ranges from 0 to 100, with lower scores indicating no failure and the highest score indicating the highest frequency of cognitive failure. According to this scale, a cut-off score of ≥43 indicates cognitive impairment [19]. Wallace et al. reported CFQ’s Cronbach’s α coefficient as 0.91 and its reliability coefficient as 0.59 [20]. In Iran, Cronbach’s α coefficient for the entire scale was reported to be 0.84, indicating the high reliability and validity of the Persian version [21]. In our study, Cronbach’s α was calculated to be 0.94.
Independent variables in this study included educational level, gender, marital status, consumption of tea and coffee one hour before bedtime, use of specific medications, housing status, buying/selling shifts, daily commute status, average use of mobile applications and the internet, satisfaction with living conditions, level of fatigue, sleep duration, sleep quality, and sleepiness. The collected data were analyzed in SPSS software, version 23. In the descriptive analysis section, mean and standard deviation values were calculated for quantitative variables. To perform statistical analysis, the normality of the data was first examined using the Kolmogorov-Smirnov Test. Based on its results, the nonparametric Mann-Whitney U and Kruskal-Wallis tests were used to compare the cognitive failure score based on demographic variables due to the lack of abnormality of the CFT data distribution. Spearman’s rank correlation test was also used to examine the relationship of sleep quality and sleepiness with cognitive failures. The generalized linear models (GLM) testing was used to adjust for confounding variables. The significance level was set at 0.05.
Results
After removing seven questionnaires due to incomplete responses, the data of 207 medical students were examined, among whom 50.7% were interns and 49.3% were externs. The majority of them were female (55.1%) and single (88.9%). Table 1 provides more information about the participants.

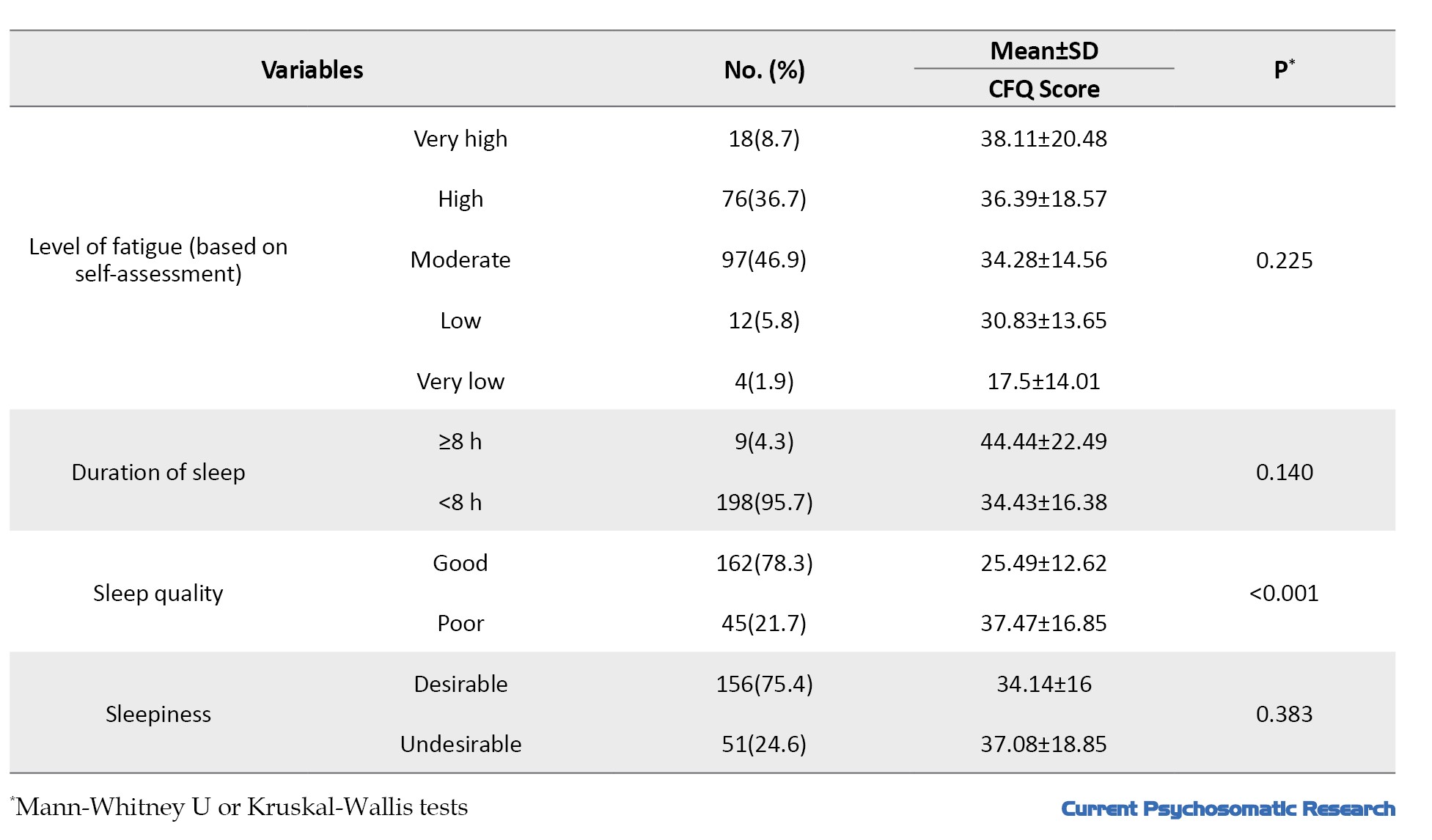
More than 95% reported less than 8 hours of sleep per night. The mean PSQI score was 6.76±2.88. Based on the PSQI score, 45 students (21.7%) had good sleep quality and 162(78.3%) had poor sleep quality. The prevalence of sleepiness based on the KSS score was 24.6%. Also, 30.9% of students had high cognitive failures. The prevalence of cognitive failures was higher in interns than in externs, but this difference was not statistically significant based on the chi-square test results (P=0.096) (Figure 1). Also, as seen in Table 1, the CFQ score was significantly different based on academic satisfaction (P=0.039), use of specific medication (P=0.005), average time spent using mobile applications and the internet (P=0.018), buying shifts (P=0.038), satisfaction with living conditions (P=0.003), study level (P=0.009), and sleep quality (P<0.001).
Spearman’s correlation test results revealed a positive relationship between poor sleep quality and cognitive failure (r=0.398, P<0.001), but not between sleepiness and cognitive failure (P>0.05). By eliminating the effect of confounding factors using the GLM multiple test, a positive and significant association was observed between cognitive failure and the factors of sleep quality (P<0.001, β=1.67), use of specific medications (P=0.009, β=6.65), and average use of mobile applications and the internet (P=0.004, β=-6.67) with in medical students (Table 2).
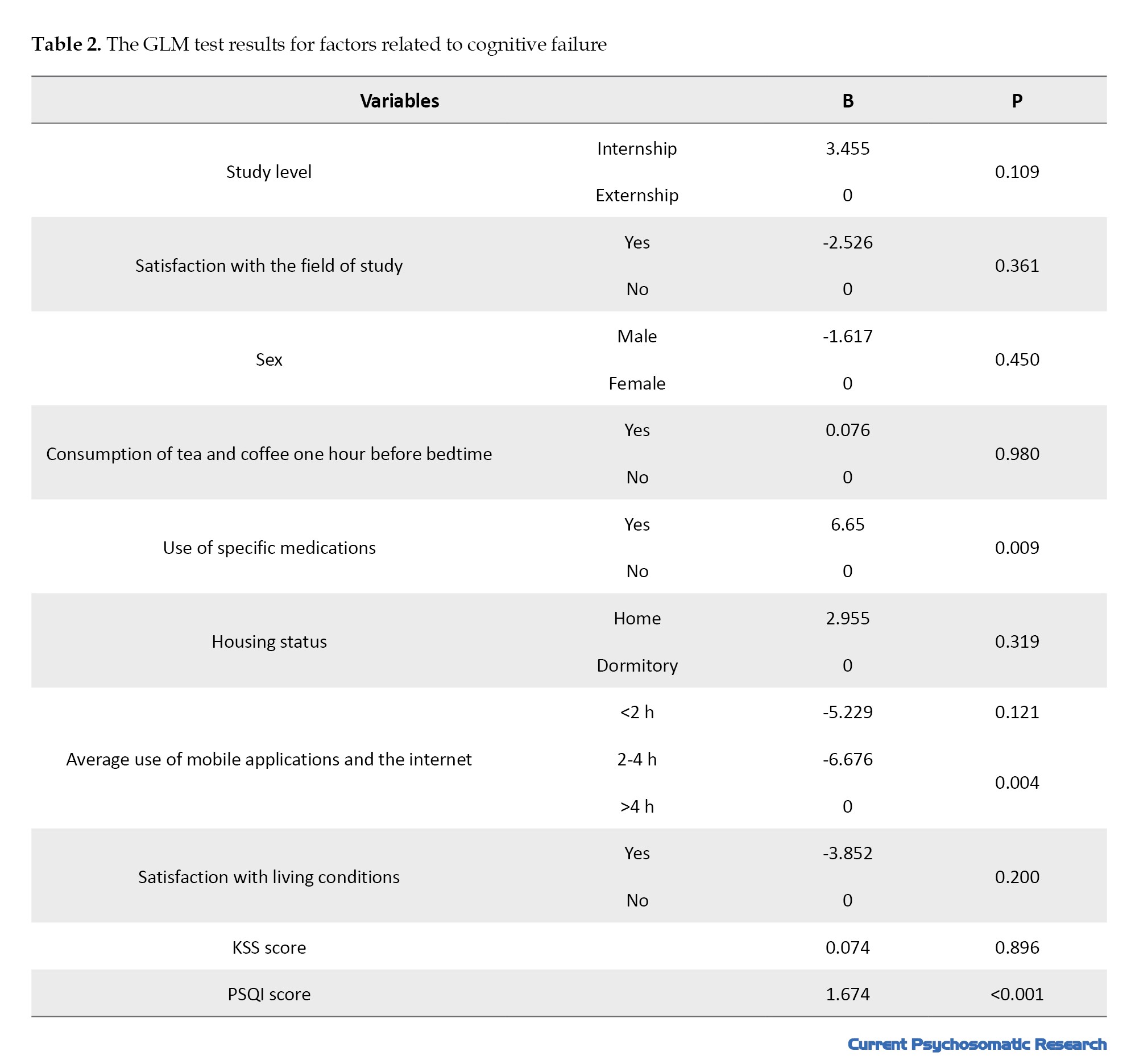
For every one-unit increase in PSQI score, the average CFQ score increased by 1.674 units. With the use of specific medications, the CFQ score increased by 6.65 units. Also, the use of mobile applications and the internet for only 2-4 hours a day can reduce the CFQ score by 6.67 units.
Discussion
According to the findings, more than three-quarters of BUMS medical students did not have adequate sleep quality, and about one-quarter of them suffered from sleepiness during work. Also, the prevalence of high/severe cognitive failures among them was 30.9%. In univariate analyses, a significantly positive association was observed between poor sleep quality and the occurrence of cognitive failure. In multivariate analyses, this association remained significant after controlling for the effects of confounding variables. In the present study, 24.6% of medical students had high daytime sleepiness. This is significantly lower than the rates reported in other studies for medical students in Morocco (36.3%) [10], Brazil (46.5%) [22], Malaysia (35.5%) [23], India (30.6%) [2], Pakistan (39.5%) [24], and Saudi Arabia (37.8%) [25], as well as the rate (35.9%) reported in a systematic review and meta-analysis by Seoane et al. [26]. The reasons for this discrepancy can be due to differences in demographic characteristics, sample size, educational levels, educational centers, work shift allocation, rest facilities, and nutrition of students and the type of measurement tools. In the mentioned studies, the Epworth sleepiness scale (ESS) was used to assess sleepiness, while we used the KSS.
There are several reasons why BUMS medical students had a high daytime sleepiness. One possible reason for this situation could be the students’ short nighttime sleep duration. Studies have found that students who get less sleep at night or whose sleep does not follow a regular schedule are more likely to experience daytime sleepiness [27-29]. According to the National Sleep Foundation, people aged 18-25 need 7-9 hours of sleep per night [30]. Therefore, it is expected that medical students sleep at least 7 hours per day, but in the present study, the majority of medical students (95.7%) had less than 7 hours of sleep at night. In the study by Seoane et al. only 29.1% of students had insufficient sleep duration [26].
In the present study, 83.3% of medical students had poor sleep quality. This rate is much higher than the rates reported in studies conducted on Moroccan (58.2%) [10], Brazilian (62.2%) [22], Indian (32.53%) [31], and Saudi Arabian (74.2%) [32] medical students. This discrepancy can be due to the fact that these studies were conducted on medical students of different ages, in different years of study, and in different countries. In a study by Hangouche et al., 3rd- to 5th-year medical students had lower sleep quality than 1st- to 2nd-year students [10]. Nojomi et al. showed a positive and significant relationship between the age of students and poor sleep quality [33].
In the present study, 30.9% of medical students had high cognitive failures. Those with higher study levels (interns compared to externs), medication use, higher hours of mobile application/internet use, higher frequency of buying shifts per month, and lower sleep quality had higher cognitive failure. Additionally, a positive relationship was found between poor sleep quality and cognitive failure. In a study among medical students, Varalakshmi et al. reported a 51.7% incidence of cognitive failures. Poor diet, poor interpersonal relationships, degree of adaptation to university life and relationships with new friends, living conditions in dormitories, and parents’ financial status were identified as risk factors [34]. In other studies, other factors such as age [35], gender [4, 36-38], marital status [35], and shift work [35, 36] were also associated with the incidence of cognitive failures. The findings of our study are consistent with those of Singla et al. Their findings also showed that inappropriate use of the Internet, low physical activity, and poor sleep quality were associated with cognitive decline [39]. Higher frequency of buying shifts and long work shifts can increase the incidence of cognitive failure in interns compared to externs, by increasing fatigue and applying more work pressure. The results of a relatively similar study in South Korea [40] showed that shift workers made more mistakes at work than non-shift workers, possibly due to their depressed mood, poor sleep quality, and cognitive impairment. In the study by Hong et al., lower sleep quality was also associated with more cognitive failures in daily life [41]. The relationship between sleep quality and cognitive failure is complex and bidirectional. Sleep disturbance, in various ways such as increased wakefulness or sleep fragmentation, can cause excessive neural activity without sufficient time for homeostasis, and subsequently lead to dysfunction of the nervous system [7].
One of the limitations of this study was the lack of in-depth analysis of the role of potential confounding factors (such as stress or academic burden), which is recommended to be investigated in future studies. Other limitations of this study included the use of self-report tools, a cross-sectional design (which precludes inferring causality), and the potential for response bias.
Conclusion
Given the prevalence of poor sleep quality in more than three-quarters of interns and externs at BUMS, and the direct relationship between this factor and a high level of cognitive failure in them, the authorities are recommended to implement measures to improve sleep quality and reduce the problem of sleepiness among medical students, such as more careful management of shifts, improving sleeping and resting conditions, making dietary changes, and educating on sleep hygiene, with the aim of preventing cognitive failures, reduced teaching quality, and the occurrence of medical errors.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Babol University of Medical Sciences, Babol, Iran (Code: IR.MUBABOL.HRI.REC.1402.019).
Funding
This study was financially supported by Babol University of Medical Sciences, Babol, Iran.
Authors' contributions
Study design and conceptualization: Aram Tirgar; Data collection, initial draft preparation: Sara Mohammadi Daniali; Data analysis: Zahra Garaeili; Investigation, review and editing: Aram Tirgar and Samaneh Pourhadi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all students who participated in this study for their cooperation, as well as the Deputy for Research and Technology of Babol University of Medical Sciences for financial support.
References
Sleep is an essential component of physical and mental health, and is crucial for learning, strengthening memory, efficient consolidation of knowledge, and acquiring desired skills [1]. There is a growing body of evidence that good sleep is important for optimal neurocognitive and psychomotor function in humans [1, 2]. Sleep has a profound impact on mental integration and, consequently, on cognitive functions. Insufficient sleep, on the other hand, causes the dissociation of consciousness, impaired attention, and delayed cognitive functions [3].
According to past studies, one of the major causes of accidents in work environments is cognitive error. Many people have had the experience that their behavior and thoughts change from time to time, or are involuntary and unwanted. These behaviors range from simple forgetfulness to functional impairments such as dropping tools or equipment during work. Donald Broadbent in 1982 called such errors “cognitive failures,” which is similar to the term “slips” used by Reason. According to him, slips can be classified into three general forms: slips in attention (failures in understanding), slips in memory (failures related to information retrieval), and slips in motor actions (unintentional actions or slips of action) [4]. Attention to these cognitive failures through a scientific study can make them less likely to occur in work environments [5]. Given the relative and inconclusive scientific evidence regarding the relationship between sleep quality and cognitive performance, the role of sleep in cognitive function has garnered increasing attention in neuroscience and sleep-related research over the past few decades [6-8].
Poor sleep quality and sleep deprivation are very common among medical students due to constant stress and anxiety caused by heavy curriculum and course content, frequent exams, fear of not achieving desired results [9], hospital work shifts, and long hours of study late at night [10]. Although the most important consequences are increased risk of burnout, psychoactive substance use, anxiety, and depression [10] in medical students, the impact on cognitive functions and academic performance, and ultimately the quality of care, is also conceivable [8]. The results of a study on medical and non-medical students in 2024 showed that most of them had a sleep duration of less than 7 hours, and students who had high sleep quality had good academic performance [11]. Another study on clinical-year medical students reported that poor sleep quality had a negative impact on grade point average and academic performance, creating a vicious cycle [9]. Although no definitive results were found regarding the association of poor sleep quality with the incidence of medical errors among medical students, studies in other occupational groups have shown that poor sleep quality can have a detrimental effect on a broad range of cognitive functions, including decision-making, problem-solving, creative thinking, memory, learning, attention, and reasoning in employees. For example, a study has shown that poor sleep quality can lead to reduced safety behaviors and an increased risk of road traffic accidents [12]. Therefore, given the importance and sensitivity of the subject and the lack of related studies among medical students in Iran, we aimed to investigate the relationship of sleep quality and sleepiness with the occurrence of cognitive failures in Iranian medical students.
Materials and Methods
This is a cross-sectional study that was conducted on medical students in internship and externship courses at Babol University of Medical Sciences (BUMS) in 2023. The required sample size was estimated to be 187, based on previous research [13] and using the formula, by considering the correlation coefficient between sleep quality and cognitive performance (r=0.26), a test power of 95% and a significance level of 0.05. However, considering a 15% possibility of sample dropout, the sample size increased to 214. Participants were selected using a convenience sampling method. The criteria for entering the study included at least 1 month of study in the internship and apprenticeship courses, willingness to participate in the study, and fully answering the questions. The exclusion criteria were the uptake of sleeping pills prescribed for insomnia and sleep disorders (e.g. diazepam, oxazepam, clonazepam, lorazepam, flurazepam, chlordiazepoxide, zolpidem, and melatonin), a history of sleep disorders before entering the educational courses, and not responding completely or incorrectly to questions.
The Pittsburgh sleep quality index (PSQI), Karolinska sleepiness scale (KSS), and cognitive failure questionnaire (CFQ) were administered to participants and were collected after two days. The PSQI has 19 items and 7 subscales. The total score ranges from 0 to 21; a global scale score of ≥5 indicates poor sleep quality, while a score of <5 shows adequate sleep quality. Buysse et al. [14] reported a Cronbach’s α value of 0.83 for the internal consistency of PSQI [14]. In Iran, Sheikhinasb et al. [15] reported a Cronbach’s α and split-half reliability of 0.81 and 0.78, respectively [15]. In our study, Cronbach’s α was calculated to be 0.84. The KSS is a 9-level scale, with values 1-5 indicating a desirable level of alertness and values 6-9 indicating an undesirable level of alertness. The score of this scale is correlated with electroencephalographic results and behavioral and executive test variables, indicating its high validity in measuring sleepiness [16-18]. The content validity ratio and content validity index for the Persian version of this questionnaire were reported to be 0.86 and 0.81, respectively [18]. In our study, Cronbach’s α was calculated to be 0.87. The CFQ has 25 questions to measure everyday failures in the areas of perception, memory, and motor function. The total score ranges from 0 to 100, with lower scores indicating no failure and the highest score indicating the highest frequency of cognitive failure. According to this scale, a cut-off score of ≥43 indicates cognitive impairment [19]. Wallace et al. reported CFQ’s Cronbach’s α coefficient as 0.91 and its reliability coefficient as 0.59 [20]. In Iran, Cronbach’s α coefficient for the entire scale was reported to be 0.84, indicating the high reliability and validity of the Persian version [21]. In our study, Cronbach’s α was calculated to be 0.94.
Independent variables in this study included educational level, gender, marital status, consumption of tea and coffee one hour before bedtime, use of specific medications, housing status, buying/selling shifts, daily commute status, average use of mobile applications and the internet, satisfaction with living conditions, level of fatigue, sleep duration, sleep quality, and sleepiness. The collected data were analyzed in SPSS software, version 23. In the descriptive analysis section, mean and standard deviation values were calculated for quantitative variables. To perform statistical analysis, the normality of the data was first examined using the Kolmogorov-Smirnov Test. Based on its results, the nonparametric Mann-Whitney U and Kruskal-Wallis tests were used to compare the cognitive failure score based on demographic variables due to the lack of abnormality of the CFT data distribution. Spearman’s rank correlation test was also used to examine the relationship of sleep quality and sleepiness with cognitive failures. The generalized linear models (GLM) testing was used to adjust for confounding variables. The significance level was set at 0.05.
Results
After removing seven questionnaires due to incomplete responses, the data of 207 medical students were examined, among whom 50.7% were interns and 49.3% were externs. The majority of them were female (55.1%) and single (88.9%). Table 1 provides more information about the participants.

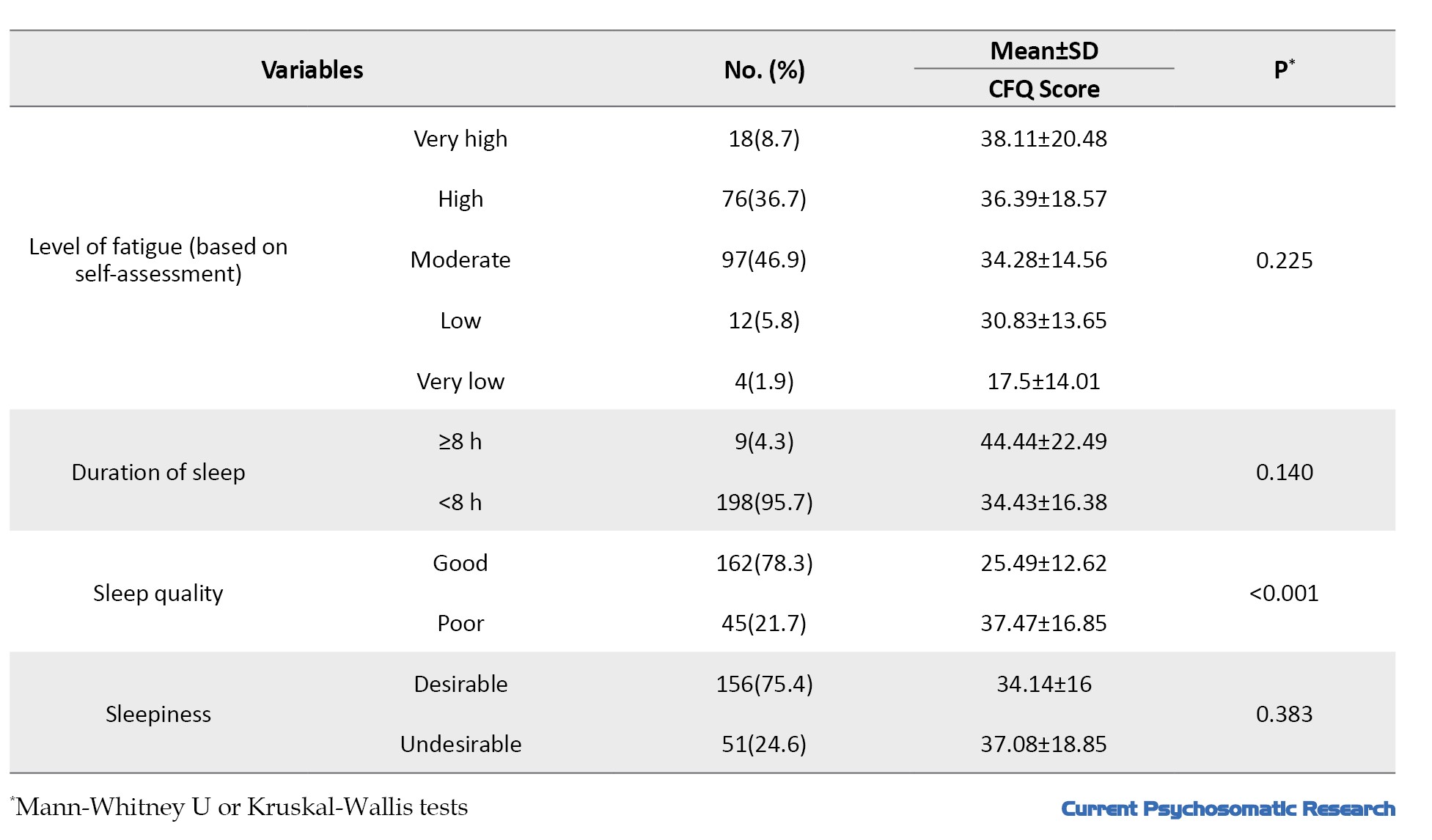
More than 95% reported less than 8 hours of sleep per night. The mean PSQI score was 6.76±2.88. Based on the PSQI score, 45 students (21.7%) had good sleep quality and 162(78.3%) had poor sleep quality. The prevalence of sleepiness based on the KSS score was 24.6%. Also, 30.9% of students had high cognitive failures. The prevalence of cognitive failures was higher in interns than in externs, but this difference was not statistically significant based on the chi-square test results (P=0.096) (Figure 1). Also, as seen in Table 1, the CFQ score was significantly different based on academic satisfaction (P=0.039), use of specific medication (P=0.005), average time spent using mobile applications and the internet (P=0.018), buying shifts (P=0.038), satisfaction with living conditions (P=0.003), study level (P=0.009), and sleep quality (P<0.001).
Spearman’s correlation test results revealed a positive relationship between poor sleep quality and cognitive failure (r=0.398, P<0.001), but not between sleepiness and cognitive failure (P>0.05). By eliminating the effect of confounding factors using the GLM multiple test, a positive and significant association was observed between cognitive failure and the factors of sleep quality (P<0.001, β=1.67), use of specific medications (P=0.009, β=6.65), and average use of mobile applications and the internet (P=0.004, β=-6.67) with in medical students (Table 2).
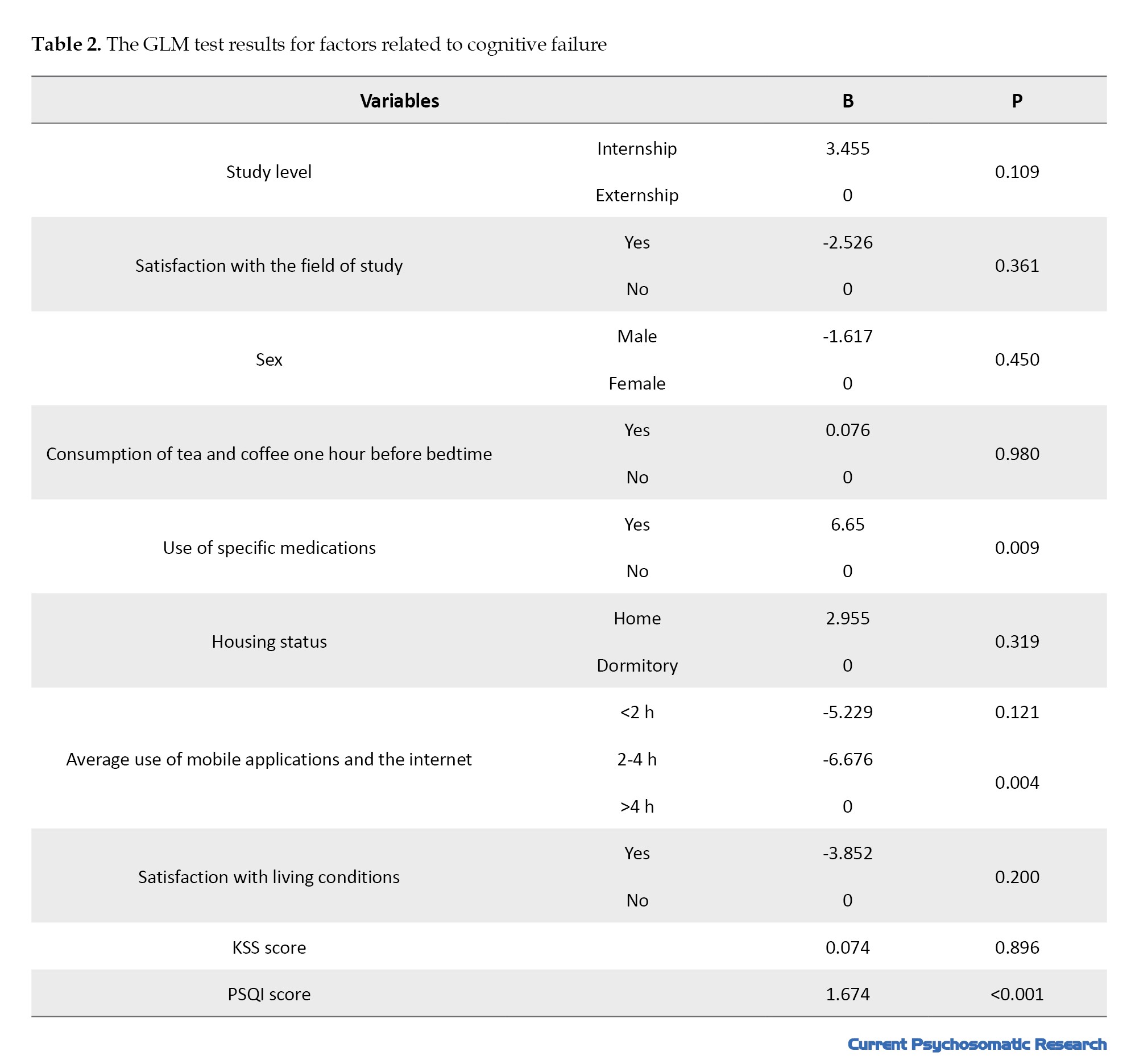
For every one-unit increase in PSQI score, the average CFQ score increased by 1.674 units. With the use of specific medications, the CFQ score increased by 6.65 units. Also, the use of mobile applications and the internet for only 2-4 hours a day can reduce the CFQ score by 6.67 units.
Discussion
According to the findings, more than three-quarters of BUMS medical students did not have adequate sleep quality, and about one-quarter of them suffered from sleepiness during work. Also, the prevalence of high/severe cognitive failures among them was 30.9%. In univariate analyses, a significantly positive association was observed between poor sleep quality and the occurrence of cognitive failure. In multivariate analyses, this association remained significant after controlling for the effects of confounding variables. In the present study, 24.6% of medical students had high daytime sleepiness. This is significantly lower than the rates reported in other studies for medical students in Morocco (36.3%) [10], Brazil (46.5%) [22], Malaysia (35.5%) [23], India (30.6%) [2], Pakistan (39.5%) [24], and Saudi Arabia (37.8%) [25], as well as the rate (35.9%) reported in a systematic review and meta-analysis by Seoane et al. [26]. The reasons for this discrepancy can be due to differences in demographic characteristics, sample size, educational levels, educational centers, work shift allocation, rest facilities, and nutrition of students and the type of measurement tools. In the mentioned studies, the Epworth sleepiness scale (ESS) was used to assess sleepiness, while we used the KSS.
There are several reasons why BUMS medical students had a high daytime sleepiness. One possible reason for this situation could be the students’ short nighttime sleep duration. Studies have found that students who get less sleep at night or whose sleep does not follow a regular schedule are more likely to experience daytime sleepiness [27-29]. According to the National Sleep Foundation, people aged 18-25 need 7-9 hours of sleep per night [30]. Therefore, it is expected that medical students sleep at least 7 hours per day, but in the present study, the majority of medical students (95.7%) had less than 7 hours of sleep at night. In the study by Seoane et al. only 29.1% of students had insufficient sleep duration [26].
In the present study, 83.3% of medical students had poor sleep quality. This rate is much higher than the rates reported in studies conducted on Moroccan (58.2%) [10], Brazilian (62.2%) [22], Indian (32.53%) [31], and Saudi Arabian (74.2%) [32] medical students. This discrepancy can be due to the fact that these studies were conducted on medical students of different ages, in different years of study, and in different countries. In a study by Hangouche et al., 3rd- to 5th-year medical students had lower sleep quality than 1st- to 2nd-year students [10]. Nojomi et al. showed a positive and significant relationship between the age of students and poor sleep quality [33].
In the present study, 30.9% of medical students had high cognitive failures. Those with higher study levels (interns compared to externs), medication use, higher hours of mobile application/internet use, higher frequency of buying shifts per month, and lower sleep quality had higher cognitive failure. Additionally, a positive relationship was found between poor sleep quality and cognitive failure. In a study among medical students, Varalakshmi et al. reported a 51.7% incidence of cognitive failures. Poor diet, poor interpersonal relationships, degree of adaptation to university life and relationships with new friends, living conditions in dormitories, and parents’ financial status were identified as risk factors [34]. In other studies, other factors such as age [35], gender [4, 36-38], marital status [35], and shift work [35, 36] were also associated with the incidence of cognitive failures. The findings of our study are consistent with those of Singla et al. Their findings also showed that inappropriate use of the Internet, low physical activity, and poor sleep quality were associated with cognitive decline [39]. Higher frequency of buying shifts and long work shifts can increase the incidence of cognitive failure in interns compared to externs, by increasing fatigue and applying more work pressure. The results of a relatively similar study in South Korea [40] showed that shift workers made more mistakes at work than non-shift workers, possibly due to their depressed mood, poor sleep quality, and cognitive impairment. In the study by Hong et al., lower sleep quality was also associated with more cognitive failures in daily life [41]. The relationship between sleep quality and cognitive failure is complex and bidirectional. Sleep disturbance, in various ways such as increased wakefulness or sleep fragmentation, can cause excessive neural activity without sufficient time for homeostasis, and subsequently lead to dysfunction of the nervous system [7].
One of the limitations of this study was the lack of in-depth analysis of the role of potential confounding factors (such as stress or academic burden), which is recommended to be investigated in future studies. Other limitations of this study included the use of self-report tools, a cross-sectional design (which precludes inferring causality), and the potential for response bias.
Conclusion
Given the prevalence of poor sleep quality in more than three-quarters of interns and externs at BUMS, and the direct relationship between this factor and a high level of cognitive failure in them, the authorities are recommended to implement measures to improve sleep quality and reduce the problem of sleepiness among medical students, such as more careful management of shifts, improving sleeping and resting conditions, making dietary changes, and educating on sleep hygiene, with the aim of preventing cognitive failures, reduced teaching quality, and the occurrence of medical errors.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Babol University of Medical Sciences, Babol, Iran (Code: IR.MUBABOL.HRI.REC.1402.019).
Funding
This study was financially supported by Babol University of Medical Sciences, Babol, Iran.
Authors' contributions
Study design and conceptualization: Aram Tirgar; Data collection, initial draft preparation: Sara Mohammadi Daniali; Data analysis: Zahra Garaeili; Investigation, review and editing: Aram Tirgar and Samaneh Pourhadi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all students who participated in this study for their cooperation, as well as the Deputy for Research and Technology of Babol University of Medical Sciences for financial support.
References
- Demir G. Daytime sleepiness and related factors in nursing students. Nurse Educ Today. 2017; 59:21-5. [DOI:10.1016/j.nedt.2017.08.003] [PMID]
- Giri PA, Baviskar MP, Phalke DB. Study of sleep habits and sleep problems among medical students of Pravara Institute of Medical Sciences Loni, Western Maharashtra, India. Ann Med Health Sci Res. 2013; 3(1):51-4. [DOI:10.4103/2141-9248.109488] [PMID]
- Carley DW, Farabi SS. Physiology of sleep. Diabetes Spectr. 2016; 29(1):5-9. [DOI:10.2337/diaspect.29.1.5] [PMID]
- Mohammady MJ, Sedighi A, Khaleghdoost T, Nejad EK, Javadi-Pashaki N. [Relationship between nurses’ subjective workload and occupational cognitive failure in intensive care units (Persian)]. J Crit Care Nurs. 2018; 11:53-61. [Link]
- Azizian Kohan N, Fathi D. Prediction of Cognitive Failure at Work Based on Job Stress and Workload with the Mediating Role of Organizational Climate in Physical Education Staff. J Occup Health Epidemiol. 2020; 9(2):110-6. [DOI:10.29252/johe.9.2.110]
- Zavecz Z, Tamás N, Galkó A, Nemeth D, Janacsek K. The relationship between subjective sleep quality and cognitive performance in healthy young adults: Evidence from three empirical studies. bioRxiv. 2019. [DOI:10.1101/328369]
- Gilley RR. The role of sleep in cognitive function: The value of a good night’s rest. Clin EEG Neurosci. 2023; 54(1):12-20. [DOI:10.1177/15500594221090067] [PMID]
- Hua J, Sun H, Shen Y. Improvement in sleep duration was associated with higher cognitive function: A new association. Aging (Albany NY). 2020; 12(20):20623-44. [DOI:10.18632/aging.103948] [PMID]
- Adel Hammouda MA, ElRafey DS. Sleep quality and its effect on academic performance among fourth year medical students at Zagazig university. Zagazig Univ Med J. 2024; 30:76. [Link]
- Hangouche AJE, Jniene A, Aboudrar S, Errguig L, Rkain H, Cherti M, et al. Relationship between poor quality sleep, excessive daytime sleepiness and low academic performance in medical students. Adv Med Educ Pract. 2018; 9:631-8. [DOI:10.2147/AMEP.S162350] [PMID]
- Rathore MA, Khan M, Irfan Z, Amir E. Quality and quantity of sleep and its effects on academic performance among medical and nonmedical students. Pak Armed Forces Med J. 2024; 74(3):609. [Link]
- Atchaya S, Pandeeswari MS, Dhanya N. Sleep Quality and Cognitive Failure among College Students. Int J Indian Psychol. 2025; 13(1):1622-31. [Link]
- Evasco MA, Santos J, Albino M, Rinion L, Salina S, Fernando A. The relationship between sleep quality impact and Cognitive failure among undergraduate student commuters of the polytechnic university of the Philippines - Manila. Manila: Polytechnic University of the Philippines; 2025. [Link]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
- Sheikhi-Nasab S, Mehrabizadeh M, Makvandi B. [The relationship between stress, sleep quality and perfectionism with chronic fatigue in Ahwaz special school teachers (Persian)]. Paper presented at: International Conference on Psychology and the Culture of Life. 27 August 2015; Istanbul, Turkey. [Link]
- Afshari Saleh L, Rahimpour F, Rafeemanesh E, Ahmadi F, Vakili V, Yazdani F. Shift Work as a Risk Factor for Poor Sleep Quality and Daytime Sleepiness in Khorasan Railway Personnel in Iran.Shiraz E-Med J. 2022; 24(1):e130052. [DOI:10.5812/semj-130052]
- Smart D, James L, Odom-Maryon T, Rowan S. Effect of subjective sleepiness on critical skills performance in National Guard medical personnel during extensive disaster training. Health Emerg Disaster Nurs. 2020; 7(1):17-26. [DOI:10.24298/hedn.2019-0007]
- Zare R, Choobineh A, Keshavarzi S, Moghateli S. [Investigation of the relationship of sleep quality, sleepiness and sickness absence (Persian)]. Iran J Ergon. 2016; 4(2):1-7. [DOI:10.21859/joe-040230]
- Voortman M, De Vries J, Hendriks CMR, Elfferich MDP, Wijnen PAHM, Drent M. Everyday cognitive failure in patients suffering from neurosarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2019; 36(1):2-10. [DOI:10.36141/svdld.v36i1.7412] [PMID]
- Wallace JC. Confirmatory factor analysis of the cognitive failures questionnaire: Evidence for dimensionality and construct validity. Pers Individ Dif. 2004; 37(2):307-24. [DOI:10.1016/j.paid.2003.09.005]
- Abolghasemi A, Kiamarsi A. [The relationship between metacognition and cognitive failures in the elderly (Persian)]. Adv Cogn Sci. 2009; 11(1):8-15. [Link]
- Perotta B, Arantes-Costa FM, Enns SC, Figueiro-Filho EA, Paro H, Santos IS, et al. Sleepiness, sleep deprivation, quality of life, mental symptoms and perception of academic environment in medical students. BMC Med Educ. 2021; 21(1):111. [DOI:10.1186/s12909-021-02544-8] [PMID]
- Zailinawati AH, Teng CL, Chung YC, Teow TL, Lee PN, Jagmohni KS. Daytime sleepiness and sleep quality among Malaysian medical students. Med J Malaysia. 2009; 64(2):108-10. [PMID]
- Surani AA, Zahid S, Surani A, Ali S, Mubeen M, Khan RH. Sleep quality among medical students of Karachi, Pakistan. J Pak Med Assoc. 2015; 65(4):380-2. [PMID]
- Al-Zahrani JM, Aldossari KK, Abdulmajeed I, Al-Ghamdi SH, Al-Shamrani AM, Al-Qahtani NS. Daytime sleepiness and academic performance among medical students. Health Sci J. 2016; 10(3):13. [Link]
- Seoane HA, Moschetto L, Orliacq F, Orliacq J, Serrano E, Cazenave MI, et al. Sleep disruption in medicine students and its relationship with impaired academic performance: A systematic review and meta-analysis. Sleep Med Rev. 2020; 53:101333. [DOI:10.1016/j.smrv.2020.101333] [PMID]
- Huang CF, Yang LY, Wu LM, Liu Y, Chen HM. Determinants of daytime sleepiness in first-year nursing students: A questionnaire survey. Nurse Educ Today. 2014; 34(6):1048-53. [DOI:10.1016/j.nedt.2013.11.005] [PMID]
- Regestein Q, Natarajan V, Pavlova M, Kawasaki S, Gleason R, Koff E. Sleep debt and depression in female college students. Psychiatry Res. 2010; 176(1):34-9. [DOI:10.1016/j.psychres.2008.11.006] [PMID]
- Taher YA, Samud AM, Ratimy AH, Seabe AM. Sleep complaints and daytime sleepiness among pharmaceutical students in Tripoli. Libyan J Med. 2012; 7. [DOI:10.3402/ljm.v7i0.18930] [PMID]
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National sleep foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health. 2015; 1(1):40-3. [DOI:10.1016/j.sleh.2014.12.010] [PMID]
- Priya J, Singh J, Kumari S, Res A. Study of the factors associated with poor sleep among medical students. Indian J Basic Appl Med Res. 2017; 6(3):422-9. [Link]
- Siddiqui AF, Al-Musa H, Al-Amri H, Al-Qahtani A, Al-Shahrani M, Al-Qahtani M. Sleep patterns and predictors of poor sleep quality among medical students in King Khalid University, Saudi Arabia. Malays J Med Sci. 2016; 23(6):94-102. [DOI:10.21315/mjms2016.23.6.10] [PMID]
- Nojomi M, Ghalhe Bandi MF, Kaffashi S. Sleep pattern in medical students and residents. Arch Iran Med. 2009; 12(6):542-9. [PMID]
- Varalakshmi VS, Karthick S, Jothy J. Prevalence of elevated blood pressure, stress, and anxiety and its association with cognitive failure among medical students-A crosssectional study. Natl J Physiol Pharm Pharmacol. 2020; 10(3):232-5. [DOI:10.5455/njppp.2020.10.001012020300012020]
- Yousef Zade A, Mazloumi A, Abbasi M, Akbar Zade A. [Investigating the relationship between cognitive failures and workload among nurses of Imam Khomeini and Vali-e-Asr hospitals in Tehran (Persian)]. J Health Saf Work. 2016; 6(2):57-68. [Link]
- Mehri F, Babaei-Pouya A, Karimollahi M. Intensive care unit nurses in iran: occupational cognitive failures and job content. Front Public Health. 2022; 10:786470. [DOI:10.3389/fpubh.2022.786470] [PMID]
- Rostampour A, Mohammadi H, Rahimpoor R, Sarvi F, Dortaj E, Ziaei M, et al. The survey of relationship between the sleep quality with cognitive failures and job performance among airport staff. Iran J Ergon. 2022; 9(4):175-86. [DOI:10.18502/iehfs.v9i4.14297]
- Hendriks C, Drent M, De Kleijn W, Elfferich M, Wijnen P, De Vries J. Everyday cognitive failure and depressive symptoms predict fatigue in sarcoidosis: A prospective follow-up study. Respir Med. 2018; 138S:S24-S30. [DOI:10.1016/j.rmed.2017.11.008] [PMID]
- Singla D, Desai OP, Basista R, Khan SA. Association between internet use, sleep, cognition and physical activity levels during COVID-19 lockdown. Sleep Vigil. 2023; 1-10. [DOI:10.1007/s41782-023-00232-9] [PMID]
- Yeo H, Lee J, Jeon S, Lee S, Hwang Y, Kim J, et al. Sleep disturbances, depressive symptoms, and cognitive efficiency as determinants of mistakes at work in shift and non-shift workers. Front Public Health. 2022; 10:1030710. [DOI:10.3389/fpubh.2022.1030710] [PMID]
- Hong W, Liu RD, Ding Y, Sheng X, Zhen R. Mobile phone addiction and cognitive failures in daily life: The mediating roles of sleep duration and quality and the moderating role of trait self-regulation. Addict Behav. 2020; 107:106383.[DOI:10.1016/j.addbeh.2020.106383] [PMID]
Type of Study: Research |
Subject:
Epidymology
Received: 2025/03/17 | Accepted: 2025/09/23 | Published: 2024/07/8
Received: 2025/03/17 | Accepted: 2025/09/23 | Published: 2024/07/8
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |