Fri, Jan 30, 2026
[Archive]
Volume 2, Issue 4 (Summer 2024)
CPR 2024, 2(4): 221-232 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jafarpoor F, Zardkhane S A. 6SQuID Framework and Its Application in Designing an Intervention to Reduce Sedentary Behavior Among Employees: A Review. CPR 2024; 2 (4) :221-232
URL: http://cpr.mazums.ac.ir/article-1-141-en.html
URL: http://cpr.mazums.ac.ir/article-1-141-en.html
Department of Psychology, Faculty of Education & Psychology, Shahid Beheshti University, Tehran, Iran.
Keywords: Clinical interventions, Intervention study, Six steps in quality intervention development (6SQuID), Step-by-step strategy
Full-Text [PDF 1608 kb]
(133 Downloads)
| Abstract (HTML) (593 Views)
Full-Text: (86 Views)
Introduction
Interventions are strategies to change behavior in order to solve a problem or improve a situation, implemented in a purposeful manner. Complex interventions address different groups or levels of the target population and attempt to influence multiple outcomes [1, 2]. A complex intervention is ideally developed through the collaboration of diverse interdisciplinary working groups consisting of researchers, psychologists, sociologists, members of the target community, and policymakers. Such collaboration can increase the chance of intervention acceptance by the target community and its success [3, 4]. The process of developing interventions should be such that it can maximize their effectiveness and sustainability; in other words, an intervention should be effective in addition to being efficient; otherwise, there is a risk of misallocation of research resources due to poorly designed interventions [5]. Systematic development and promotion of the effectiveness of interventions is as important as, or even more important than, their evaluation. Despite the extensive literature on how to evaluate interventions [2, 6, 7], little information is available to guide researchers on how to develop interventions and maximize their effectiveness. Maximizing the effectiveness of interventions can avoid spending large sums on implementing weak interventions or ineffective evaluations [4].
Given the need to develop a systematic framework for developing interventions, different articles have been published on various approaches to developing interventions in recent years [8, 9]. Skivington et al. [6] consider the development processes of an intervention to include design, pilot, evaluation, and report. The UK medical research council [2, 6], in its guidance on the development and evaluation of complex interventions, describes three stages of development, feasibility, and implementation. Of course, the starting and ending points of the development stages of an intervention are not always clear, and there may be overlap between the design stage and the feasibility/pilot stages, as some feasibility studies are often part of the intervention development stage [10].
So far, several strategies have been proposed for developing interventions, including intervention mapping, the behavior change wheel, and the multi-phase optimization strategy [11, 12]. Although existing strategies for developing interventions attempt to bring about individual behavior change through psychosocial interventions, each has its own limitations. For example, the intervention mapping strategy has an individual and socio-psychological orientation, and its implementation requires highly specialized skills, and it may take years [4, 13]. In the behavior change wheel strategy, the sequence of steps has been criticized as inconsistent or conceptually unclear, and some of the adjustments used have been reported to be confusing [13, 14]. The UK Medical Research Council (MRC) guidelines outline only three general steps and provide little detail on the intervention development methodology [4, 6, 11]. Therefore, Wight et al. [4] presented 6SQuID framework, based on the strengths and full attention to the possible limitations of existing strategies, as well as the need to develop a systematic and sufficiently detailed framework for developing interventions. The present study aimed to explain the standard stages of the 6SQuID model based on a previously implemented intervention for reducing the sedentary behaviors of employees.
Materials and Methods
This study was designed as a descriptive review with the aim of introducing and elaborating the 6SQuID framework while also demonstrating its practical relevance through an illustrative example. The review process was guided by the objective of providing both a conceptual understanding of the framework and an applied perspective on how it can be utilized in the development of interventions. To achieve this, the methodological approach comprised several interrelated activities. First, key scholarly sources that originally developed, refined, or reported applications of the 6SQuID framework were identified and examined. Foundational methodological articles were prioritized, and additional empirical papers were selected when they explicitly described the sequential use of the model. Sources were located through targeted searches in international academic databases, including PubMed, Scopus, and Web of Science, and were complemented by citation tracking and reference list screening. Second, the identified sources were subjected to a structured qualitative synthesis, focusing on the theoretical underpinnings, conceptual clarity, and methodological principles of the framework. Each of the six stages of 6SQuID was extracted and critically analyzed in order to highlight its role in ensuring systematic and transparent intervention development. This analytical process allowed the model to be synthesized and presented in a coherent manner that is both accessible to readers and transferable across different fields of application.
Finally, to strengthen the practical dimension of the review, one representative intervention study employing 6SQuID was included as an illustrative case. The example was not analyzed as empirical evidence within this study; rather, it was used to demonstrate how the six steps of the framework can be operationalized in practice. This integration was intended to bridge the gap between theoretical explanation and applied implementation. This review emphasized methodological transparency, conceptual rigor, and applicability. It should therefore be regarded not as a systematic review of all available evidence, but as a methodological and narrative synthesis designed to clarify the structure, purpose, and utility of the 6SQuID framework for guiding the development of educational, clinical, and social interventions.
Results
The 6SQuID model of Wight et al. [4] was developed with a focus on public health. The goal of this model is to provide a practical framework for researchers and professionals who face complex issues and diverse contexts in designing, implementing, and evaluating interventions. This model attempts to provide a systematic approach to developing effective interventions, taking into account field realities. This model emphasizes careful problem analysis, identification of modifiable factors, context-appropriate intervention design, and continuous evaluation and modification. The step-by-step structure and logical arrangement of the model’s components are among the features that make it a suitable option for cases where specific guidance is not available. Some researchers believe that the model, although clearly structured, provides more of a general framework than a detailed and precise strategy [4, 11]. This view is not because of the model’s shortcomings, but because of its flexible nature for different types of interventions. Although not based on a specific theory in psychology or social science, the 6SQuID model is based on key concepts drawn from behavioral science, public health, and implementation studies. Concepts such as context analysis, identification of influential factors, behavior change mechanisms, and formative evaluation are integrated into the various stages of this model.
Another important feature of this model is the emphasis on the active participation of stakeholders in all stages of intervention design and development; a participation that helps increase the coherence, acceptability, and effectiveness of the intervention. Also, attention to resource efficiency, the ability to implement in real conditions, and the design of detection and correction mechanisms are among the features that make the 6SQuID model very useful for applied studies and health policy-making.
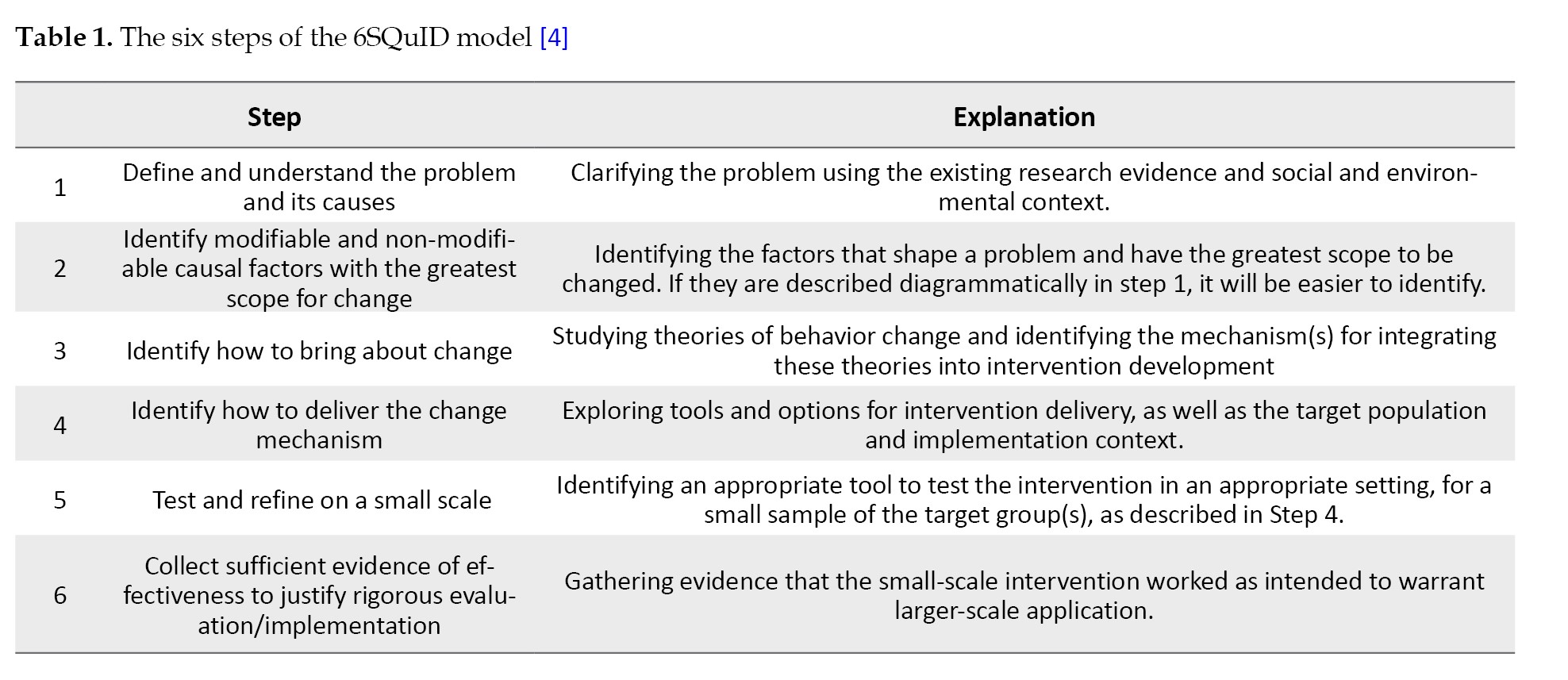
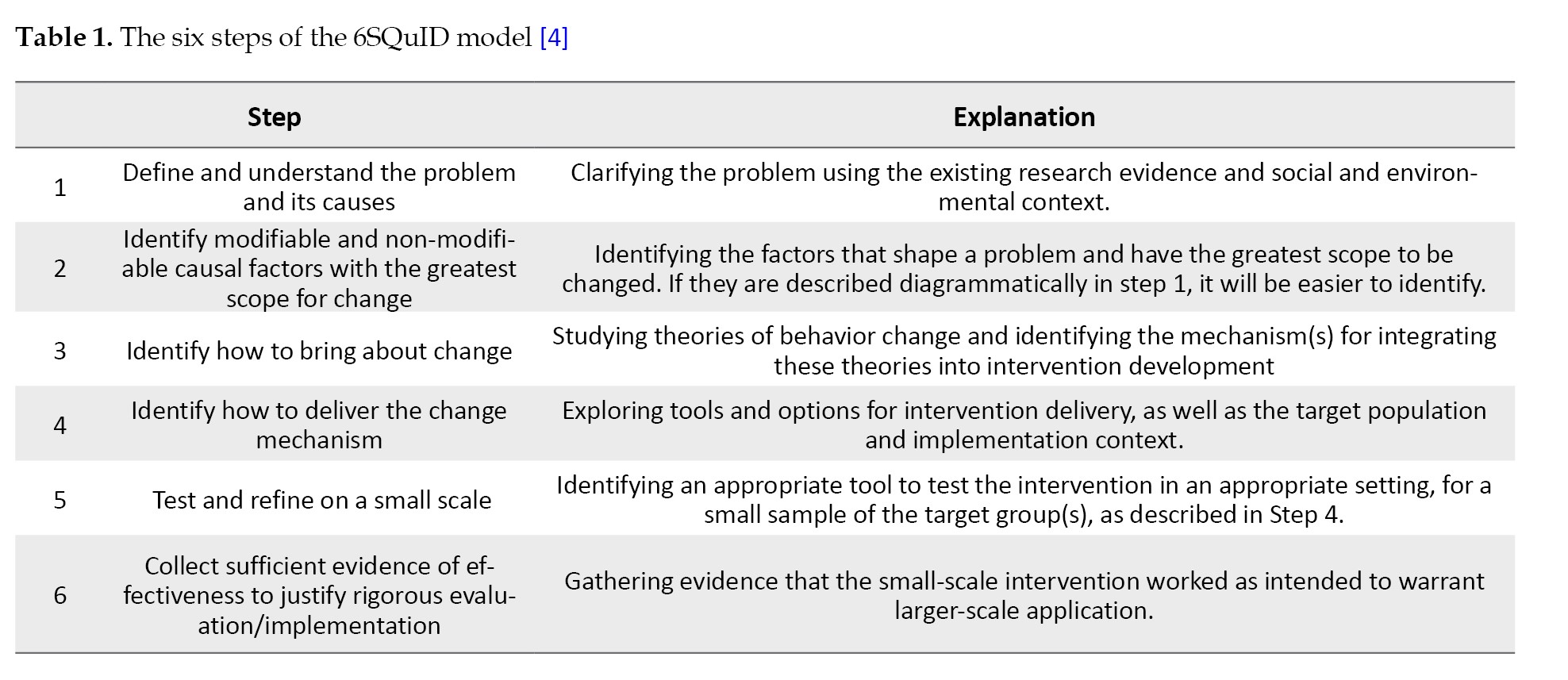
The 6SQuID model has been successfully used for designing a diverse range of behavioral and social interventions such as family-based interventions to facilitate HIV testing [15], intervention for promoting positive behaviors in adolescents [16], intervention for supporting adolescent kinship caregivers [17], brief interventions to reduce alcohol use in patients with breast cancer [18], and an intervention to reduce sedentary behavior in contact centers [19]. The six steps of the 6SQuID model are presented in Table 1.
Step 1: Defining the problem and its causes
The first step in the process of developing an intervention is to clearly define the problem that requires intervention. Many social and psychological issues, especially in the field of public health, have multiple dimensions and may not be easily defined or measured. Furthermore, there may be different perceptions of a problem among researchers, policymakers, and other stakeholders. Therefore, the problem definition should be clear, specific, and evidence-based to avoid confusion at later stages.
The process of clarifying the problem is usually carried out through a combination of methods, including: analyzing the needs of the target group, consulting with stakeholders, and reviewing existing research evidence. Once the problem is identified, its spatial and demographic distribution should be analyzed. This analysis helps us understand in which groups and in which locations the problem is most prevalent or severe. This information serves as the basis for determining the target group for intervention and designing subsequent steps. Depending on the type of problem and the context of the intervention, the target group may include individuals, families, and employees of an organization, high-risk groups, or even a local community. The 6SQuID model does not prescribe any target group in advance, but rather emphasizes that the researcher makes appropriate decisions based on empirical data and consultation with stakeholders.
In the first step, it should also be determined who is most likely to benefit from the intervention and which groups may be less affected. A precise understanding of the demographic structure of the problem has a direct impact on determining the scope of the intervention and its implementation and evaluation methods. On the other hand, it is essential to review the history of similar interventions in the same area, because awareness of the ineffectiveness or challenges of previous interventions can prevent the repetition of errors and pave the way for designing more effective interventions. In addition, analyzing the underlying and structural causes of the problem, such as economic, social, environmental, or historical conditions, plays a key role in understanding causal pathways and selecting intervention components. Answering the following questions is a useful guide in this step [20]: What is the nature and extent of the problem? At what individual, interpersonal, organizational, or societal levels does the problem exist? What are the consequences for those directly and indirectly affected? What is the history? What are its causes and which causes are most important? What has been effective in addressing the problem?
For example, in the first phase of designing the “Stand Up for Health” intervention by Tirman et al. [19], which aimed to reduce sedentary behaviors of employees, a systematic review of the existing evidence was first conducted. Then, standard questionnaires were used to measure physical activity and occupational sitting, in addition to focus group discussion sessions, which were held with employees to gain a qualitative understanding of the problem. This multi-layered process led to the identification of factors influencing sedentary behavior and ultimately, a more precise definition of the intervention.
Step 2: Identifying the causal factors with the greatest scope for change
In the second step, the focus is on identifying the causal or contextual factors that have the greatest potential for change. This step builds on the findings of the first step, where the problem is well defined and its causal pathways are clearly delineated. The goal of this step for the researcher is to select a set of influencing factors with the greatest scope for change, both scientifically and operationally, taking into account resource, time, and operational constraints. The chain of causal factors helps the researcher to emphasize the points along the causal pathway where intervention can have the greatest impact, rather than addressing general or vague causes. Although causal factors may lie at different levels of this chain, in general, modifying “upstream” structural factors – such as macro policies, organizational structures, or cultural factors – requires more time, more extensive resources, and more complex interventions than “downstream” factors, such as individual attitudes or behaviors. However, if achieved, such interventions can have broader and more lasting impacts. In interventions for complex problems, causal pathways are often intertwined and multi-layered. If these pathways have been described diagrammatically in the first step, it will be easier to identify where the intervention should focus. Also, it may be necessary to implement the intervention at multiple points simultaneously or sequentially to achieve the necessary effect. Interventions can be designed and implemented at various levels, including individual, interpersonal, community, organizational, environmental, or macro policy. In many cases, interventions that cover multiple levels simultaneously have a greater chance of sustainability and long-term effectiveness because they reduce barriers to behavioral change from multiple pathways by creating synergies across multiple dimensions [4]. Answering the following questions is necessary in step 2: Which of the factors are modifiable? How big is the impact of each factor? How does the target group interact with these factors? Is implementing the intervention at one level sufficient, or is there a need for action at multiple levels?
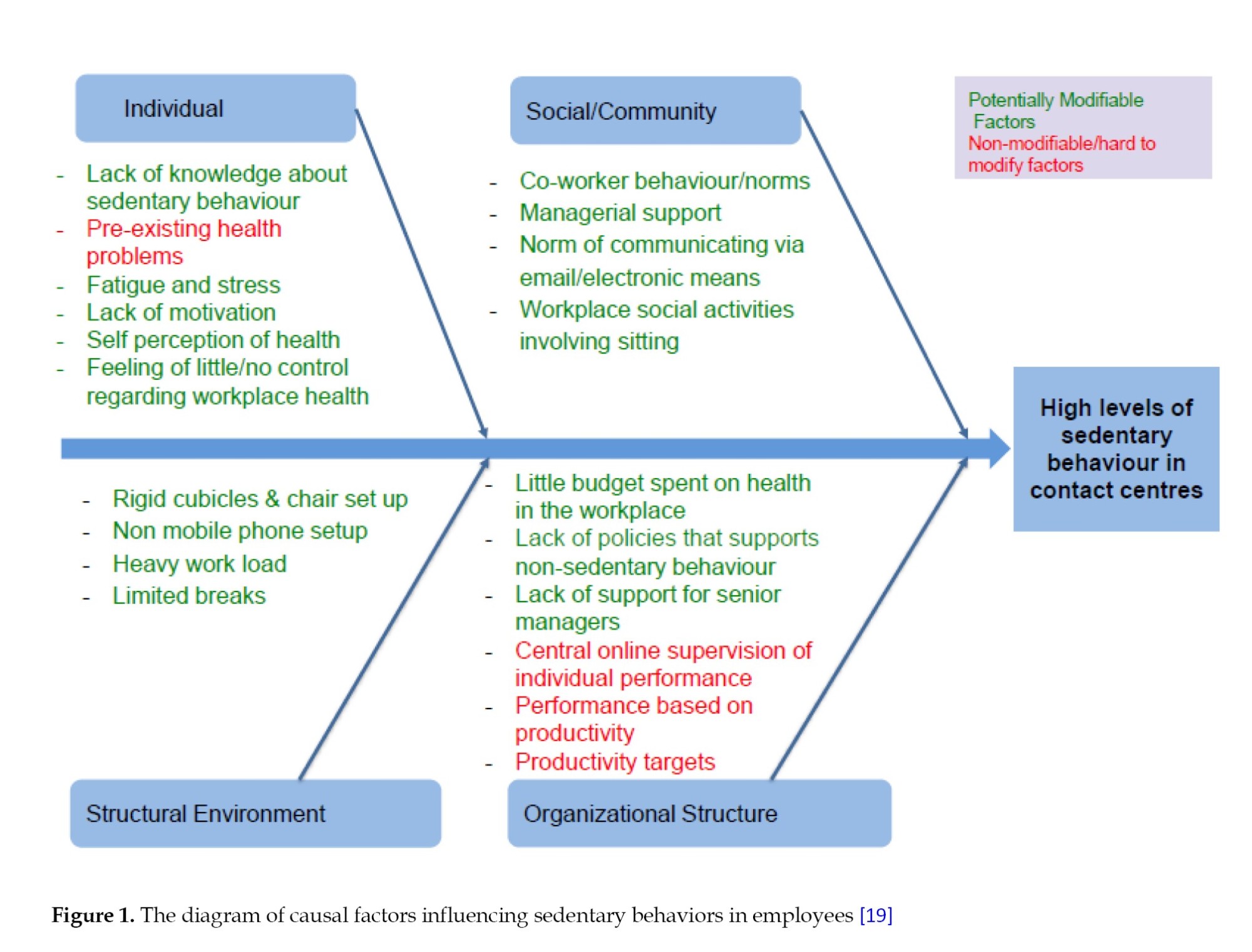
For example, in designing the “stand up for health” intervention [19], the researchers identified and analyzed a set of influential factors based on the findings from the first step. These factors were then divided into two categories: “Modifiable” and “unmodifiable” based on the possibility of change (Figure 1). These factors were further categorized into four levels: Individual, social/community, organizational, and environmental. This classification helped researchers tailor intervention design based on the strengths and weaknesses of each level and avoid overlapping or neglecting key factors.
Step 3: Identifying how to bring about change
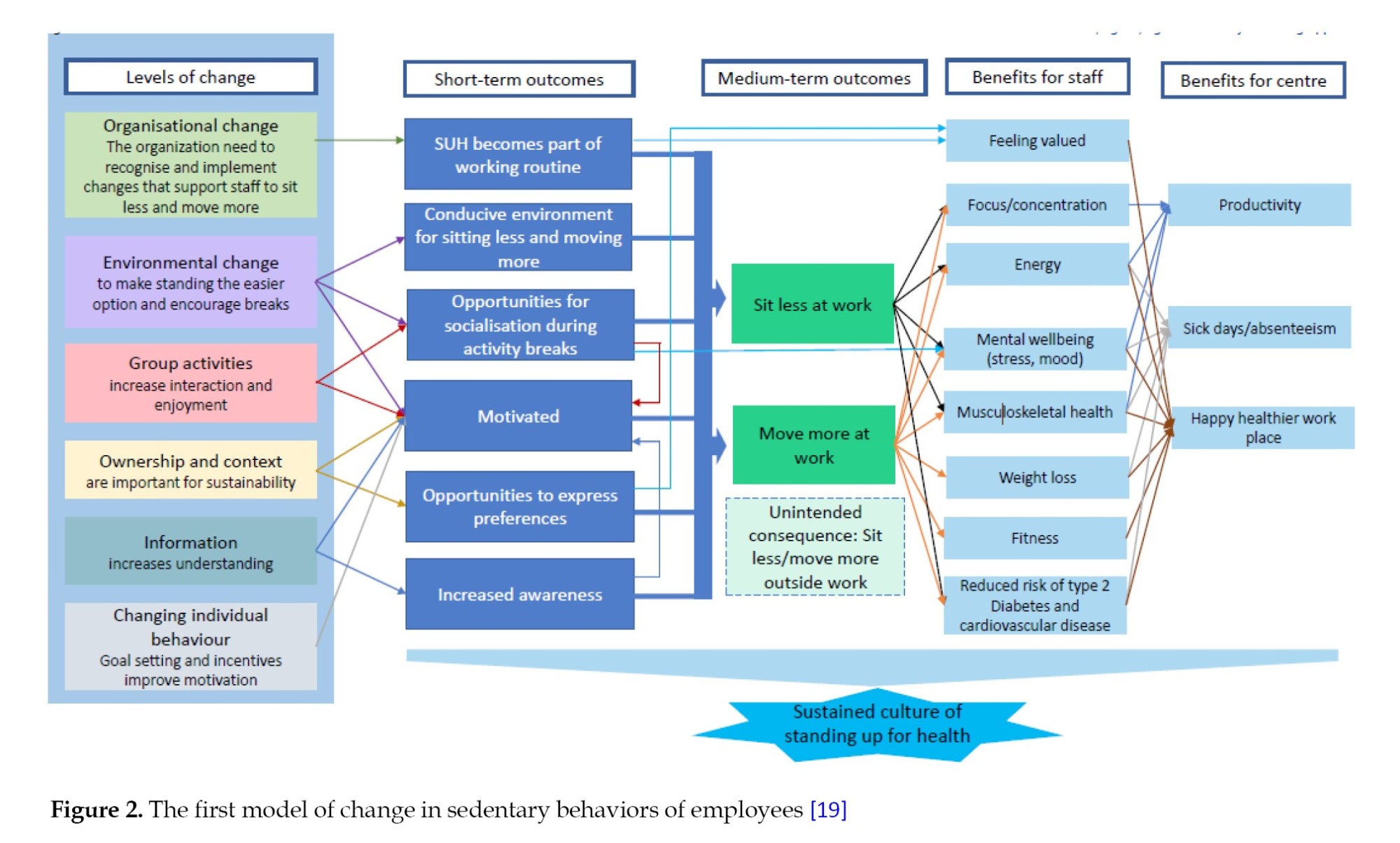
In the third step of intervention development, after identifying modifiable causal factors, the mechanism for influencing these factors to change them is determined. Determining the change mechanism is a vital process that leads to change in individuals, groups, or communities. In other words, it is very important in developing an intervention to clearly articulate the change mechanisms in the form of the theoretical and operational foundations of the intervention, and therefore, these mechanisms must be based on solid theoretical and operational foundations [4]. Ideally, a range of stakeholders should participate in developing the theoretical and practical foundations of the intervention, and if they have strong predictive and explanatory power, it can be very helpful. However, it should be noted that many conventional theories of behavior change, such as social cognition theory [21], are not comprehensive because they often focus on a single causal pathway (cognitions or motivations) and do not address socio-environmental determinants [22, 23]. The 6SQuID model allows for the achievement of goals at different levels: Short-term (changes in individuals’ knowledge, attitudes, beliefs, or skills), medium-term (changes in individual behaviors or in organizational and executive processes), and long-term (improvement of macro-outcomes such as mental health, reduction of social harms, or reduction of existing inequalities).
As an example, the third step of developing the “Stand Up for Health” intervention [19] addressed how each modifiable factor identified in the second step can be changed at four levels: Individual, social, environmental, and organizational, through the design of specific mechanisms (Figure 2).
Step 4: Identifying how to deliver the change mechanism
After identifying the modifiable factors in step 3, step 4 requires determining what mechanisms can be used to change these factors and how these change mechanisms can be delivered. A careful review of the research literature conducted in the previous steps helps to identify effective intervention components in similar contexts. The participation of stakeholders with relevant practical expertise at this step can also lead to a more realistic, implementable, and culturally and operationally appropriate design. It should be noted that implementation options are not necessarily diverse in every context. For example, in some cases, change mechanisms are only possible through legislation. Therefore, the choice of change mechanism should be made by considering the social and administrative context, available resources, structural constraints, and target group.
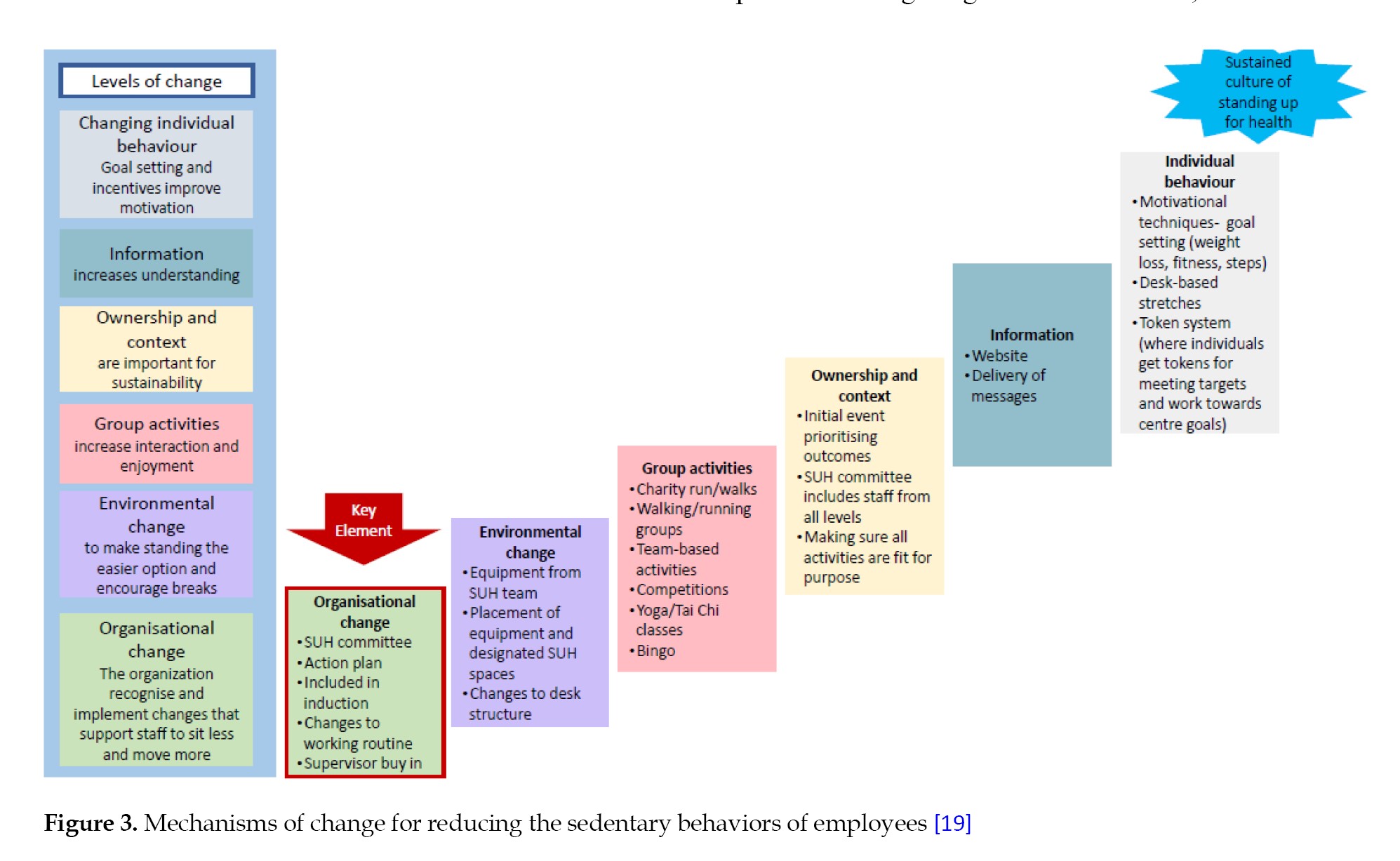
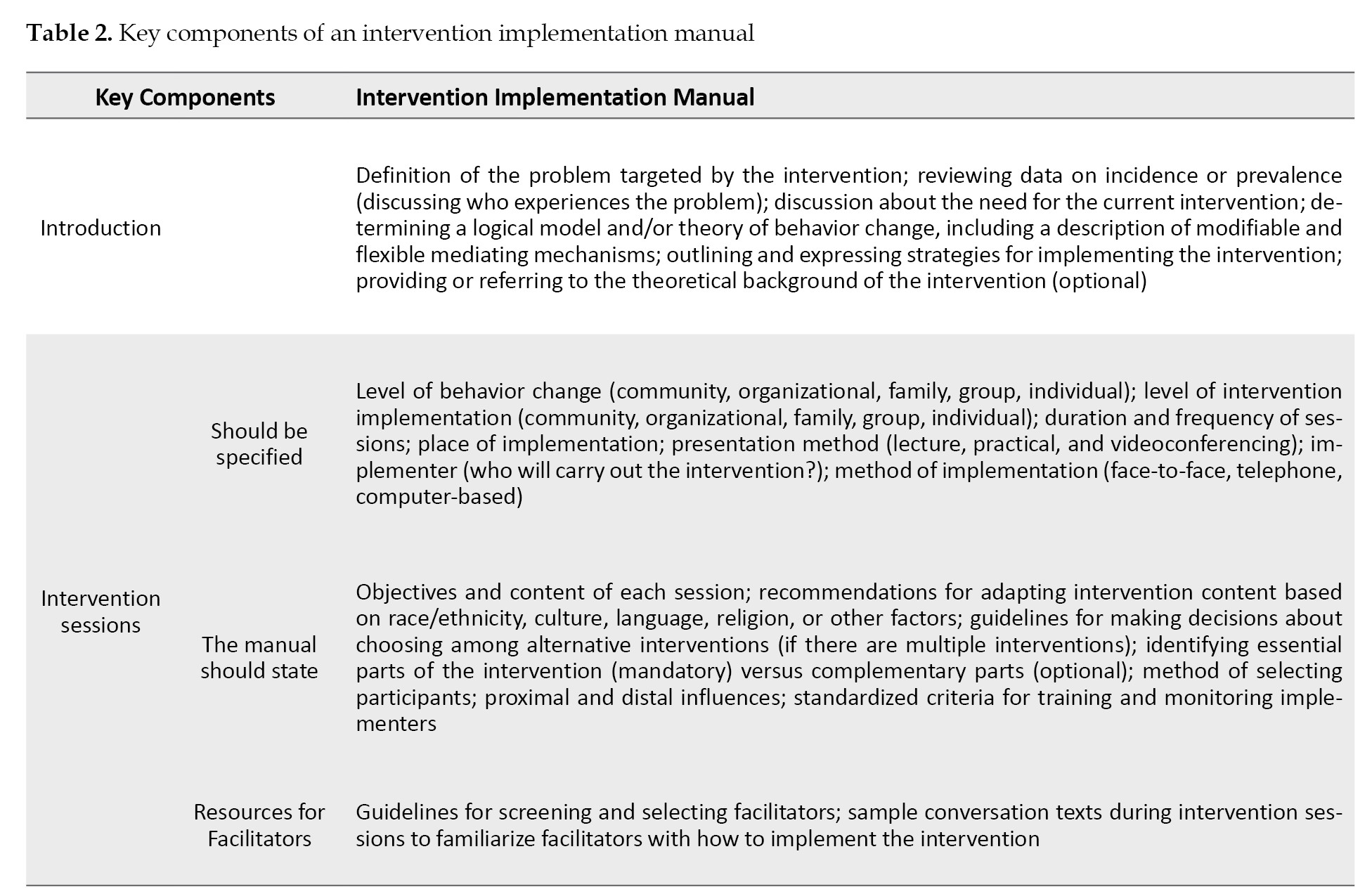
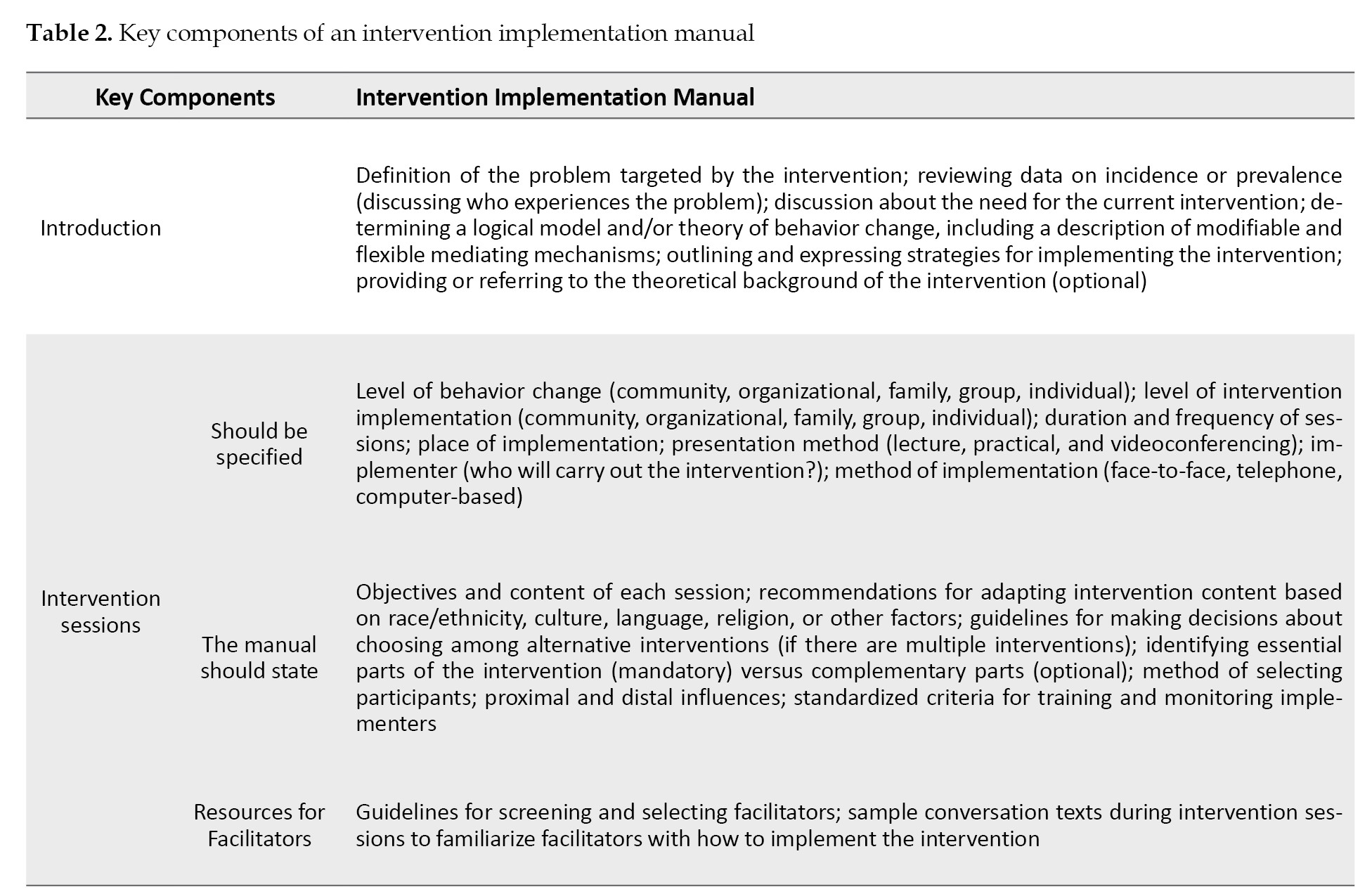
In step 4, it is necessary to assess the background, implementation requirements and potential risks of the intervention. For example, if the intervention is to be implemented by psychologists, it must be ensured that sufficient numbers of these professionals are available everywhere. In contexts such as low-income countries (including Iran), access to skilled facilitators or adequate funding for training intervention providers can be a major challenge. It is also necessary to predict potential unintended effects and harms of the intervention [24]. Lorenc and Oliver [25] divided these harms into five categories: Direct harms (e.g. risk of injury in public exercise programs), psychological harms (e.g. anxiety caused by media campaigns), equity harms (e.g. exacerbating existing inequalities by benefiting privileged groups), group/social harms (e.g. labeling obese people in interventions targeting obesity or social isolation), and opportunity harms (e.g. committing resources to ineffective/less effective interventions and losing resources to effective/more effective interventions). In step 4, a theoretical model of the intervention is also developed to outline the mechanisms of change in a structured manner. For example, in developing the “Stand Up for Health” intervention [19], the researchers used a theory of action to explain the relationship between mechanisms and outcomes (Figure 3). The final output of this step is the draft of an intervention implementation manual. Although this manual is drafted at this step, it is not exclusive to this step and is present in all steps, but is modified and improved as the intervention development progresses. The manual provides facilitators with an implementation plan for the intervention and includes the following key elements: Target population and level of intervention (individual, interpersonal, family, organizational, community, or combined), theoretical mechanisms of behavior change, implementation stages and sessions (including number, structure, and content of sessions and training methods), methods of interaction (face-to-face, telephone, digital) and implementation monitoring. Since incomplete or ambiguous instructions can lead to inconsistent implementation, invalid data, or implementation failure, the careful and clear development of this manual plays a critical role in the success of the intervention. In this regard, in 2025, a group of health experts presented a 33-item checklist for developing evidence-based implementation guidelines, which contains practical recommendations and real-world examples [26]. Therefore, in step 4, considering these recommendations along with the items mentioned in Table 2 can lead to the development of a clear and efficient intervention implementation manual.
Step 5: Testing on a small scale
This step assesses the feasibility, acceptability, and relative effectiveness of key components of the intervention in limited, controlled settings. This step provides an opportunity for the intervention to be tested before being implemented on a large scale and to be modified and optimized based on feedback and data collected. It should be noted that piloting all types of interventions is not easily possible. For example, interventions that require the adoption of major policies or national legislation are difficult to pilot before full implementation. In these cases, phased region-by-region implementation can be a suitable alternative and help to gradually adapt the intervention to local conditions and implementation processes; however, the scope is improving the mechanisms of intervention implementation, not redefining the theory of its change. In interventions designed at the individual or community level–especially innovative interventions– the implementation process typically requires a long process of repeated tests and modification, which is known as “formative evaluation”. Pilot study, especially in these cases, plays a vital role in the success of the intervention. In step 5, the following questions about the intervention should be answered: Is the intervention acceptable to the target group and its implementers? Are the time, content, location, and presentation method appropriate to the cultural and organizational context? What are the barriers to the full implementation of the intervention? How can the intervention’s coverage be expanded at the community level? Indicators such as participation rates, session retention rates, optimum content, program fidelity, and cultural fit of the intervention can be used to initially measure effectiveness and acceptability. Using feedback forms, implementation fidelity checklists, and initial behavioral change assessment questionnaires are appropriate tools for collecting data in step 5.
Pilot designs are usually simple and quasi-experimental, and are often conducted as a single-group or single-case study. In some cases, participants are asked to provide direct feedback on the program’s delivery and content. Such feedback will allow for revisions to sessions, elimination of ineffective components, and optimization of the delivery process. Given the limited sample size in step 5, using a mixed method (quantitative/qualitative) is preferable to a quantitative method. These methods make the reform path more targeted by providing a deeper understanding of the contexts of intervention success or failure. For example, collecting data repeatedly on a few key indicators is often more effective than conducting a large pre-test/post-test study. Measurements should be done before the intervention and continue through its completion to allow for the trajectory of change over time.
In addition to pilot study, part of the evaluation in step 5 is devoted to efficacy studies. These studies, using rigorous designs such as random assignment to intervention and control groups or robust quasi-experimental designs such as regression discontinuity designs, attempt to analyze the direct causal relationship between intervention implementation and behavioral outcomes. It is important to note that efficacy studies are conducted under strictly controlled conditions and are far from natural conditions. After efficacy studies, real-world effectiveness trials are conducted. These trials examine whether an intervention that was successful in a controlled setting remains effective in the real world—without widespread support, strong infrastructure, or direct researcher control. The effectiveness trial evaluates the quality of implementation, adherence to protocol, educational adequacy, and interaction with the implementation environment [27, 28].
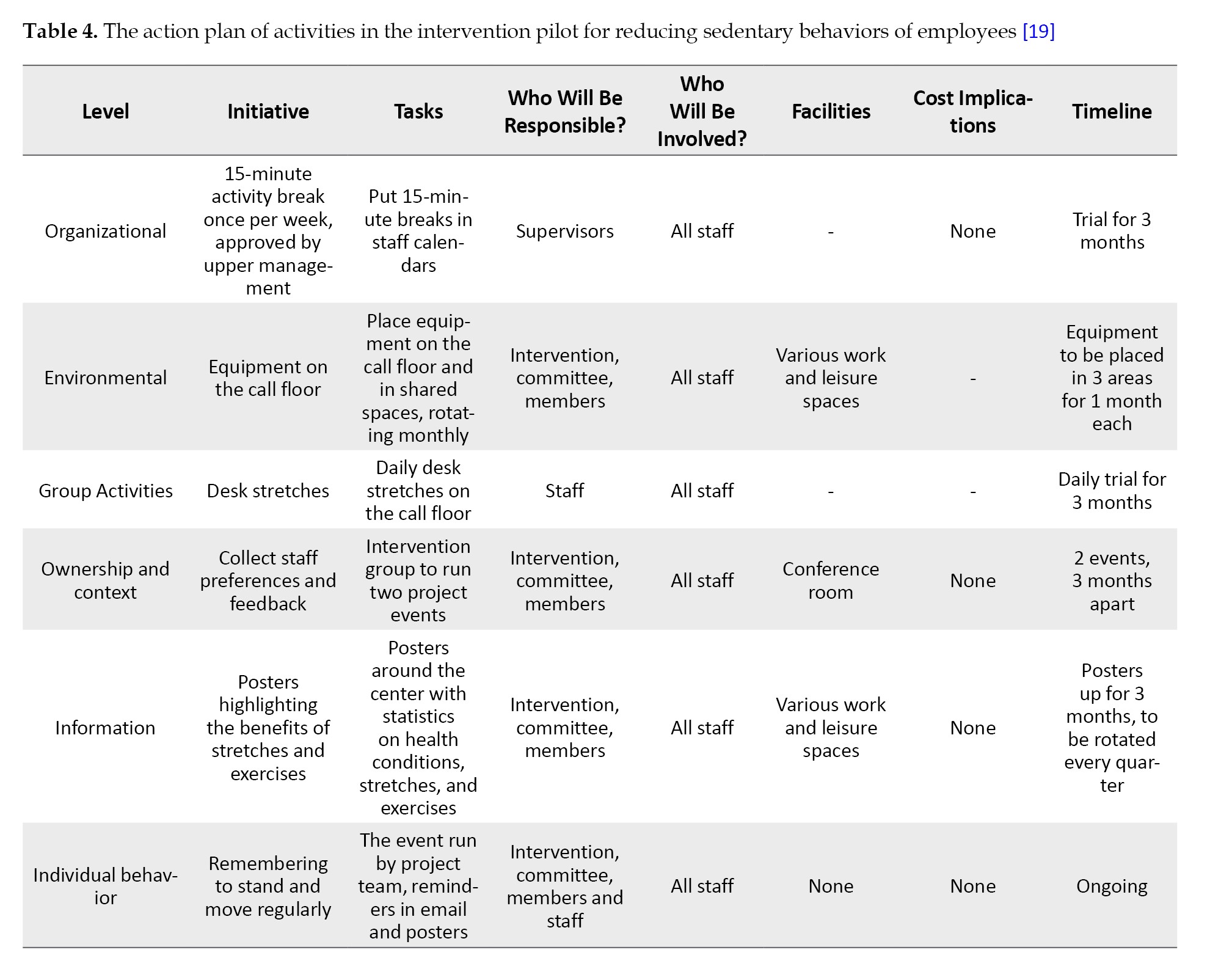
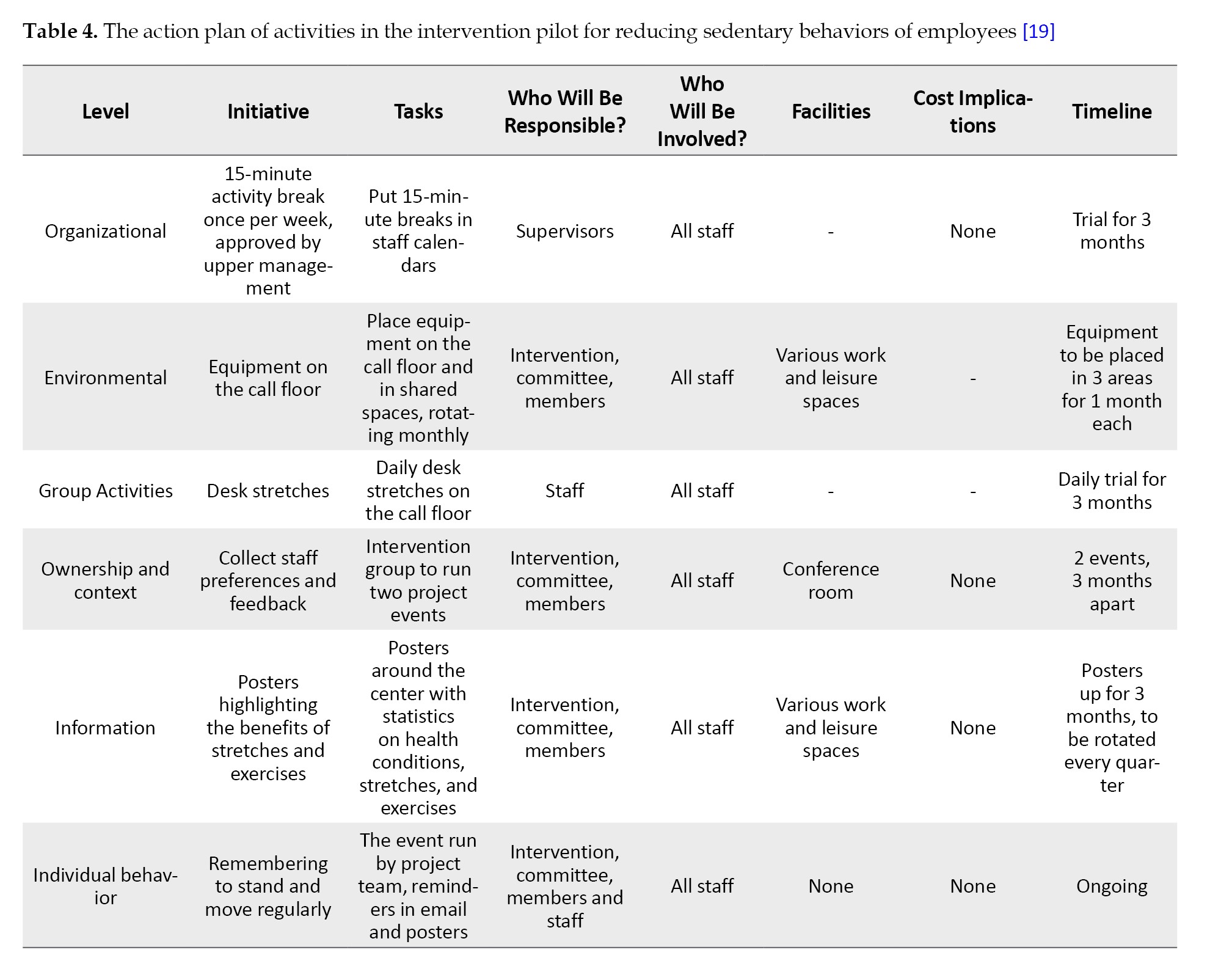
One of the strengths of the 6SQuID model is its flexibility in dealing with different implementation scenarios. Depending on the resources available, the level of stakeholder participation, and the data obtained from the pilot, the researcher can make decisions that are appropriate to the situation. Analyzing these scenarios and their consequences is an integral part of modifying and advancing the intervention. In the study for developing the “Stand Up for Health” intervention [19], step 5 began with a six-month pilot study. In this step, the intended equipment and activities were implemented and evaluated. The action plan for these activities is shown in Table 4, which includes initiatives, tasks, responsibilities, facilities, cost implications, and timeline.
Step 6: Collect sufficient evidence of effectiveness to justify rigorous evaluation/implementation
Before allocating scarce resources to implementing a large-scale intervention, sufficient evidence of the intervention’s effectiveness should be gathered to warrant such an investment. Beyond the world of research, and especially in organizations, the lack of sufficient evidence often means that implementers move toward large-scale intervention implementation without conducting a rigorous evaluation. Therefore, it is of utmost importance to accurately complete Step 6. What is sought at this stage is to obtain evidence that the intervention is proceeding according to schedule, achieving at least some short-term outcomes, and that there are no serious adverse effects. Since proving the influence of causal factors on behavior is not desired at this stage, theory-based evaluation approaches are probably the most appropriate approaches at this stage of intervention development. There are numerous evaluation guides that adequately cover how to carry out step six, but often the most practical way to gather evidence about the effectiveness of an intervention is to examine conditions before and after implementation, or by using collected data. When possible, using a control group greatly increases the strength of the evidence [4]. In the study by Tirman et al. [19], which aimed to reduce sedentary behavior in employees, the intervention was conducted at 11 contact centers in the UK as part of a large National Institute for Health Research (NIHR) feasibility study to collect sufficient evidence for a rigorous evaluation.
Discussion
Developing educational, therapeutic, and social interventions is a complex process that cannot be achieved with good intentions or sufficient resources alone. The difference between successful and unsuccessful interventions often lies in the quality of their design, the degree of adaptation to the local context, and how they are implemented. The use of structured but flexible frameworks can play a decisive role in the ultimate effectiveness of interventions. The 6SQuID model provides a systematic and pragmatic framework for designing, modifying, and implementing multilevel interventions. Originally introduced in the public health field, the model has been successfully applied in recent years to develop interventions in diverse fields, including education, mental health, and social prevention. The six steps of this model, from problem definition and analysis to collecting evidence of effectiveness for large-scale implementation, provide complete coverage from design to implementation. The logical order of intervention development steps, as well as the pragmatic approach of this strategy, make it suitable for use in cases where practical guidance for intervention development is lacking. The recursive and nonlinear nature of this model is also important. Contrary to the superficial perception of numbered stages, intervention development in this framework is a dynamic, iterative, and flexible process. In practice, intervention designers repeatedly return to previous steps, revise the intervention based on evidence, and modify the final structure in response to field feedback. This cycle of redesign prevents the implementation of costly and inefficient interventions, making optimal use of limited resources.
A key feature of the 6SQuID model is the strong focus on stakeholder engagement throughout all stages of intervention development. In this process, stakeholder engagement not only helps improve the acceptability and effectiveness of the intervention but also provides a platform for incremental and modifiable design. Tools such as participatory design, formative evaluation, and continuous feedback play a pivotal role in this regard. Some strategies for engaging with stakeholders include building mutual trust, providing clear communication, and seeking feedback, as recommended by the International Association for Public Participation and the integrated framework for implementation research [29].
Cultural and organizational adaptability is another important advantage of the 6SQuID model. Since it focuses on the design path rather than prescribing fixed content, it has a high ability to adapt to different cultural, social, and organizational characteristics, especially in steps 2, 3, and 4, where analyzing the implementation context and using local feedback have a special place, allowing the designed intervention to adapt to environmental requirements. This model can be used as a dynamic and practical roadmap for designing behavioral, educational, or social interventions in a variety of contexts.
The 6SQuID model is not limited to a specific field and can be very useful, especially in situations where there is a need to design an intervention that is tailored to the socio-cultural context, stakeholder participation, and gradual testing. This model allows for continuous review and modification in steps 3-5 based on feedback, formative evaluation, and contextual conditions. Despite these advantages, the 6SQuID model has some limitations. It can be misinterpreted as a linear model, while the nature of intervention development is often complex, interactive, and nonlinear. Also, the quality of implementation of early stages such as context analysis and change mechanism design is highly dependent on the quality and scope of available evidence, and this can lead to design errors in contexts with poor data. Moreover, practical adaptation of the model to some cultural or institutional contexts may require redefining or combining steps. Finally, although the model emphasizes stakeholder participation, achieving effective participation faces structural and cultural challenges.
Conclusion
The 6SQuID framework offers a systematic, iterative, and pragmatic approach for developing educational, therapeutic, and social interventions. Its six-step structure—from problem definition to rigorous evaluation—provides comprehensive guidance for designing interventions that are contextually tailored, evidence-informed, and actively engage stakeholders. The framework’s flexibility enables adaptation across diverse cultural, organizational, and disciplinary settings, while its emphasis on formative evaluation and iterative refinement enhances feasibility, acceptability, and effectiveness. Despite potential challenges, including misinterpretation of its nonlinear nature and reliance on high-quality contextual evidence, 6SQuID remains a robust model for ensuring methodological rigor and practical relevance in intervention development. Researchers and policymakers are encouraged to adopt this framework to systematically design, implement, and evaluate interventions, thereby optimizing resource use and promoting sustainable outcomes.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank the Faculty of Psychology and Educational Sciences at Shahid Beheshti University for providing the conditions that facilitated this work.
References
Interventions are strategies to change behavior in order to solve a problem or improve a situation, implemented in a purposeful manner. Complex interventions address different groups or levels of the target population and attempt to influence multiple outcomes [1, 2]. A complex intervention is ideally developed through the collaboration of diverse interdisciplinary working groups consisting of researchers, psychologists, sociologists, members of the target community, and policymakers. Such collaboration can increase the chance of intervention acceptance by the target community and its success [3, 4]. The process of developing interventions should be such that it can maximize their effectiveness and sustainability; in other words, an intervention should be effective in addition to being efficient; otherwise, there is a risk of misallocation of research resources due to poorly designed interventions [5]. Systematic development and promotion of the effectiveness of interventions is as important as, or even more important than, their evaluation. Despite the extensive literature on how to evaluate interventions [2, 6, 7], little information is available to guide researchers on how to develop interventions and maximize their effectiveness. Maximizing the effectiveness of interventions can avoid spending large sums on implementing weak interventions or ineffective evaluations [4].
Given the need to develop a systematic framework for developing interventions, different articles have been published on various approaches to developing interventions in recent years [8, 9]. Skivington et al. [6] consider the development processes of an intervention to include design, pilot, evaluation, and report. The UK medical research council [2, 6], in its guidance on the development and evaluation of complex interventions, describes three stages of development, feasibility, and implementation. Of course, the starting and ending points of the development stages of an intervention are not always clear, and there may be overlap between the design stage and the feasibility/pilot stages, as some feasibility studies are often part of the intervention development stage [10].
So far, several strategies have been proposed for developing interventions, including intervention mapping, the behavior change wheel, and the multi-phase optimization strategy [11, 12]. Although existing strategies for developing interventions attempt to bring about individual behavior change through psychosocial interventions, each has its own limitations. For example, the intervention mapping strategy has an individual and socio-psychological orientation, and its implementation requires highly specialized skills, and it may take years [4, 13]. In the behavior change wheel strategy, the sequence of steps has been criticized as inconsistent or conceptually unclear, and some of the adjustments used have been reported to be confusing [13, 14]. The UK Medical Research Council (MRC) guidelines outline only three general steps and provide little detail on the intervention development methodology [4, 6, 11]. Therefore, Wight et al. [4] presented 6SQuID framework, based on the strengths and full attention to the possible limitations of existing strategies, as well as the need to develop a systematic and sufficiently detailed framework for developing interventions. The present study aimed to explain the standard stages of the 6SQuID model based on a previously implemented intervention for reducing the sedentary behaviors of employees.
Materials and Methods
This study was designed as a descriptive review with the aim of introducing and elaborating the 6SQuID framework while also demonstrating its practical relevance through an illustrative example. The review process was guided by the objective of providing both a conceptual understanding of the framework and an applied perspective on how it can be utilized in the development of interventions. To achieve this, the methodological approach comprised several interrelated activities. First, key scholarly sources that originally developed, refined, or reported applications of the 6SQuID framework were identified and examined. Foundational methodological articles were prioritized, and additional empirical papers were selected when they explicitly described the sequential use of the model. Sources were located through targeted searches in international academic databases, including PubMed, Scopus, and Web of Science, and were complemented by citation tracking and reference list screening. Second, the identified sources were subjected to a structured qualitative synthesis, focusing on the theoretical underpinnings, conceptual clarity, and methodological principles of the framework. Each of the six stages of 6SQuID was extracted and critically analyzed in order to highlight its role in ensuring systematic and transparent intervention development. This analytical process allowed the model to be synthesized and presented in a coherent manner that is both accessible to readers and transferable across different fields of application.
Finally, to strengthen the practical dimension of the review, one representative intervention study employing 6SQuID was included as an illustrative case. The example was not analyzed as empirical evidence within this study; rather, it was used to demonstrate how the six steps of the framework can be operationalized in practice. This integration was intended to bridge the gap between theoretical explanation and applied implementation. This review emphasized methodological transparency, conceptual rigor, and applicability. It should therefore be regarded not as a systematic review of all available evidence, but as a methodological and narrative synthesis designed to clarify the structure, purpose, and utility of the 6SQuID framework for guiding the development of educational, clinical, and social interventions.
Results
The 6SQuID model of Wight et al. [4] was developed with a focus on public health. The goal of this model is to provide a practical framework for researchers and professionals who face complex issues and diverse contexts in designing, implementing, and evaluating interventions. This model attempts to provide a systematic approach to developing effective interventions, taking into account field realities. This model emphasizes careful problem analysis, identification of modifiable factors, context-appropriate intervention design, and continuous evaluation and modification. The step-by-step structure and logical arrangement of the model’s components are among the features that make it a suitable option for cases where specific guidance is not available. Some researchers believe that the model, although clearly structured, provides more of a general framework than a detailed and precise strategy [4, 11]. This view is not because of the model’s shortcomings, but because of its flexible nature for different types of interventions. Although not based on a specific theory in psychology or social science, the 6SQuID model is based on key concepts drawn from behavioral science, public health, and implementation studies. Concepts such as context analysis, identification of influential factors, behavior change mechanisms, and formative evaluation are integrated into the various stages of this model.
Another important feature of this model is the emphasis on the active participation of stakeholders in all stages of intervention design and development; a participation that helps increase the coherence, acceptability, and effectiveness of the intervention. Also, attention to resource efficiency, the ability to implement in real conditions, and the design of detection and correction mechanisms are among the features that make the 6SQuID model very useful for applied studies and health policy-making.
The 6SQuID model has been successfully used for designing a diverse range of behavioral and social interventions such as family-based interventions to facilitate HIV testing [15], intervention for promoting positive behaviors in adolescents [16], intervention for supporting adolescent kinship caregivers [17], brief interventions to reduce alcohol use in patients with breast cancer [18], and an intervention to reduce sedentary behavior in contact centers [19]. The six steps of the 6SQuID model are presented in Table 1.
Step 1: Defining the problem and its causes
The first step in the process of developing an intervention is to clearly define the problem that requires intervention. Many social and psychological issues, especially in the field of public health, have multiple dimensions and may not be easily defined or measured. Furthermore, there may be different perceptions of a problem among researchers, policymakers, and other stakeholders. Therefore, the problem definition should be clear, specific, and evidence-based to avoid confusion at later stages.
The process of clarifying the problem is usually carried out through a combination of methods, including: analyzing the needs of the target group, consulting with stakeholders, and reviewing existing research evidence. Once the problem is identified, its spatial and demographic distribution should be analyzed. This analysis helps us understand in which groups and in which locations the problem is most prevalent or severe. This information serves as the basis for determining the target group for intervention and designing subsequent steps. Depending on the type of problem and the context of the intervention, the target group may include individuals, families, and employees of an organization, high-risk groups, or even a local community. The 6SQuID model does not prescribe any target group in advance, but rather emphasizes that the researcher makes appropriate decisions based on empirical data and consultation with stakeholders.
In the first step, it should also be determined who is most likely to benefit from the intervention and which groups may be less affected. A precise understanding of the demographic structure of the problem has a direct impact on determining the scope of the intervention and its implementation and evaluation methods. On the other hand, it is essential to review the history of similar interventions in the same area, because awareness of the ineffectiveness or challenges of previous interventions can prevent the repetition of errors and pave the way for designing more effective interventions. In addition, analyzing the underlying and structural causes of the problem, such as economic, social, environmental, or historical conditions, plays a key role in understanding causal pathways and selecting intervention components. Answering the following questions is a useful guide in this step [20]: What is the nature and extent of the problem? At what individual, interpersonal, organizational, or societal levels does the problem exist? What are the consequences for those directly and indirectly affected? What is the history? What are its causes and which causes are most important? What has been effective in addressing the problem?
For example, in the first phase of designing the “Stand Up for Health” intervention by Tirman et al. [19], which aimed to reduce sedentary behaviors of employees, a systematic review of the existing evidence was first conducted. Then, standard questionnaires were used to measure physical activity and occupational sitting, in addition to focus group discussion sessions, which were held with employees to gain a qualitative understanding of the problem. This multi-layered process led to the identification of factors influencing sedentary behavior and ultimately, a more precise definition of the intervention.
Step 2: Identifying the causal factors with the greatest scope for change
In the second step, the focus is on identifying the causal or contextual factors that have the greatest potential for change. This step builds on the findings of the first step, where the problem is well defined and its causal pathways are clearly delineated. The goal of this step for the researcher is to select a set of influencing factors with the greatest scope for change, both scientifically and operationally, taking into account resource, time, and operational constraints. The chain of causal factors helps the researcher to emphasize the points along the causal pathway where intervention can have the greatest impact, rather than addressing general or vague causes. Although causal factors may lie at different levels of this chain, in general, modifying “upstream” structural factors – such as macro policies, organizational structures, or cultural factors – requires more time, more extensive resources, and more complex interventions than “downstream” factors, such as individual attitudes or behaviors. However, if achieved, such interventions can have broader and more lasting impacts. In interventions for complex problems, causal pathways are often intertwined and multi-layered. If these pathways have been described diagrammatically in the first step, it will be easier to identify where the intervention should focus. Also, it may be necessary to implement the intervention at multiple points simultaneously or sequentially to achieve the necessary effect. Interventions can be designed and implemented at various levels, including individual, interpersonal, community, organizational, environmental, or macro policy. In many cases, interventions that cover multiple levels simultaneously have a greater chance of sustainability and long-term effectiveness because they reduce barriers to behavioral change from multiple pathways by creating synergies across multiple dimensions [4]. Answering the following questions is necessary in step 2: Which of the factors are modifiable? How big is the impact of each factor? How does the target group interact with these factors? Is implementing the intervention at one level sufficient, or is there a need for action at multiple levels?
For example, in designing the “stand up for health” intervention [19], the researchers identified and analyzed a set of influential factors based on the findings from the first step. These factors were then divided into two categories: “Modifiable” and “unmodifiable” based on the possibility of change (Figure 1). These factors were further categorized into four levels: Individual, social/community, organizational, and environmental. This classification helped researchers tailor intervention design based on the strengths and weaknesses of each level and avoid overlapping or neglecting key factors.
Step 3: Identifying how to bring about change
In the third step of intervention development, after identifying modifiable causal factors, the mechanism for influencing these factors to change them is determined. Determining the change mechanism is a vital process that leads to change in individuals, groups, or communities. In other words, it is very important in developing an intervention to clearly articulate the change mechanisms in the form of the theoretical and operational foundations of the intervention, and therefore, these mechanisms must be based on solid theoretical and operational foundations [4]. Ideally, a range of stakeholders should participate in developing the theoretical and practical foundations of the intervention, and if they have strong predictive and explanatory power, it can be very helpful. However, it should be noted that many conventional theories of behavior change, such as social cognition theory [21], are not comprehensive because they often focus on a single causal pathway (cognitions or motivations) and do not address socio-environmental determinants [22, 23]. The 6SQuID model allows for the achievement of goals at different levels: Short-term (changes in individuals’ knowledge, attitudes, beliefs, or skills), medium-term (changes in individual behaviors or in organizational and executive processes), and long-term (improvement of macro-outcomes such as mental health, reduction of social harms, or reduction of existing inequalities).
As an example, the third step of developing the “Stand Up for Health” intervention [19] addressed how each modifiable factor identified in the second step can be changed at four levels: Individual, social, environmental, and organizational, through the design of specific mechanisms (Figure 2).
Step 4: Identifying how to deliver the change mechanism
After identifying the modifiable factors in step 3, step 4 requires determining what mechanisms can be used to change these factors and how these change mechanisms can be delivered. A careful review of the research literature conducted in the previous steps helps to identify effective intervention components in similar contexts. The participation of stakeholders with relevant practical expertise at this step can also lead to a more realistic, implementable, and culturally and operationally appropriate design. It should be noted that implementation options are not necessarily diverse in every context. For example, in some cases, change mechanisms are only possible through legislation. Therefore, the choice of change mechanism should be made by considering the social and administrative context, available resources, structural constraints, and target group.
In step 4, it is necessary to assess the background, implementation requirements and potential risks of the intervention. For example, if the intervention is to be implemented by psychologists, it must be ensured that sufficient numbers of these professionals are available everywhere. In contexts such as low-income countries (including Iran), access to skilled facilitators or adequate funding for training intervention providers can be a major challenge. It is also necessary to predict potential unintended effects and harms of the intervention [24]. Lorenc and Oliver [25] divided these harms into five categories: Direct harms (e.g. risk of injury in public exercise programs), psychological harms (e.g. anxiety caused by media campaigns), equity harms (e.g. exacerbating existing inequalities by benefiting privileged groups), group/social harms (e.g. labeling obese people in interventions targeting obesity or social isolation), and opportunity harms (e.g. committing resources to ineffective/less effective interventions and losing resources to effective/more effective interventions). In step 4, a theoretical model of the intervention is also developed to outline the mechanisms of change in a structured manner. For example, in developing the “Stand Up for Health” intervention [19], the researchers used a theory of action to explain the relationship between mechanisms and outcomes (Figure 3). The final output of this step is the draft of an intervention implementation manual. Although this manual is drafted at this step, it is not exclusive to this step and is present in all steps, but is modified and improved as the intervention development progresses. The manual provides facilitators with an implementation plan for the intervention and includes the following key elements: Target population and level of intervention (individual, interpersonal, family, organizational, community, or combined), theoretical mechanisms of behavior change, implementation stages and sessions (including number, structure, and content of sessions and training methods), methods of interaction (face-to-face, telephone, digital) and implementation monitoring. Since incomplete or ambiguous instructions can lead to inconsistent implementation, invalid data, or implementation failure, the careful and clear development of this manual plays a critical role in the success of the intervention. In this regard, in 2025, a group of health experts presented a 33-item checklist for developing evidence-based implementation guidelines, which contains practical recommendations and real-world examples [26]. Therefore, in step 4, considering these recommendations along with the items mentioned in Table 2 can lead to the development of a clear and efficient intervention implementation manual.
Step 5: Testing on a small scale
This step assesses the feasibility, acceptability, and relative effectiveness of key components of the intervention in limited, controlled settings. This step provides an opportunity for the intervention to be tested before being implemented on a large scale and to be modified and optimized based on feedback and data collected. It should be noted that piloting all types of interventions is not easily possible. For example, interventions that require the adoption of major policies or national legislation are difficult to pilot before full implementation. In these cases, phased region-by-region implementation can be a suitable alternative and help to gradually adapt the intervention to local conditions and implementation processes; however, the scope is improving the mechanisms of intervention implementation, not redefining the theory of its change. In interventions designed at the individual or community level–especially innovative interventions– the implementation process typically requires a long process of repeated tests and modification, which is known as “formative evaluation”. Pilot study, especially in these cases, plays a vital role in the success of the intervention. In step 5, the following questions about the intervention should be answered: Is the intervention acceptable to the target group and its implementers? Are the time, content, location, and presentation method appropriate to the cultural and organizational context? What are the barriers to the full implementation of the intervention? How can the intervention’s coverage be expanded at the community level? Indicators such as participation rates, session retention rates, optimum content, program fidelity, and cultural fit of the intervention can be used to initially measure effectiveness and acceptability. Using feedback forms, implementation fidelity checklists, and initial behavioral change assessment questionnaires are appropriate tools for collecting data in step 5.
Pilot designs are usually simple and quasi-experimental, and are often conducted as a single-group or single-case study. In some cases, participants are asked to provide direct feedback on the program’s delivery and content. Such feedback will allow for revisions to sessions, elimination of ineffective components, and optimization of the delivery process. Given the limited sample size in step 5, using a mixed method (quantitative/qualitative) is preferable to a quantitative method. These methods make the reform path more targeted by providing a deeper understanding of the contexts of intervention success or failure. For example, collecting data repeatedly on a few key indicators is often more effective than conducting a large pre-test/post-test study. Measurements should be done before the intervention and continue through its completion to allow for the trajectory of change over time.
In addition to pilot study, part of the evaluation in step 5 is devoted to efficacy studies. These studies, using rigorous designs such as random assignment to intervention and control groups or robust quasi-experimental designs such as regression discontinuity designs, attempt to analyze the direct causal relationship between intervention implementation and behavioral outcomes. It is important to note that efficacy studies are conducted under strictly controlled conditions and are far from natural conditions. After efficacy studies, real-world effectiveness trials are conducted. These trials examine whether an intervention that was successful in a controlled setting remains effective in the real world—without widespread support, strong infrastructure, or direct researcher control. The effectiveness trial evaluates the quality of implementation, adherence to protocol, educational adequacy, and interaction with the implementation environment [27, 28].
One of the strengths of the 6SQuID model is its flexibility in dealing with different implementation scenarios. Depending on the resources available, the level of stakeholder participation, and the data obtained from the pilot, the researcher can make decisions that are appropriate to the situation. Analyzing these scenarios and their consequences is an integral part of modifying and advancing the intervention. In the study for developing the “Stand Up for Health” intervention [19], step 5 began with a six-month pilot study. In this step, the intended equipment and activities were implemented and evaluated. The action plan for these activities is shown in Table 4, which includes initiatives, tasks, responsibilities, facilities, cost implications, and timeline.
Step 6: Collect sufficient evidence of effectiveness to justify rigorous evaluation/implementation
Before allocating scarce resources to implementing a large-scale intervention, sufficient evidence of the intervention’s effectiveness should be gathered to warrant such an investment. Beyond the world of research, and especially in organizations, the lack of sufficient evidence often means that implementers move toward large-scale intervention implementation without conducting a rigorous evaluation. Therefore, it is of utmost importance to accurately complete Step 6. What is sought at this stage is to obtain evidence that the intervention is proceeding according to schedule, achieving at least some short-term outcomes, and that there are no serious adverse effects. Since proving the influence of causal factors on behavior is not desired at this stage, theory-based evaluation approaches are probably the most appropriate approaches at this stage of intervention development. There are numerous evaluation guides that adequately cover how to carry out step six, but often the most practical way to gather evidence about the effectiveness of an intervention is to examine conditions before and after implementation, or by using collected data. When possible, using a control group greatly increases the strength of the evidence [4]. In the study by Tirman et al. [19], which aimed to reduce sedentary behavior in employees, the intervention was conducted at 11 contact centers in the UK as part of a large National Institute for Health Research (NIHR) feasibility study to collect sufficient evidence for a rigorous evaluation.
Discussion
Developing educational, therapeutic, and social interventions is a complex process that cannot be achieved with good intentions or sufficient resources alone. The difference between successful and unsuccessful interventions often lies in the quality of their design, the degree of adaptation to the local context, and how they are implemented. The use of structured but flexible frameworks can play a decisive role in the ultimate effectiveness of interventions. The 6SQuID model provides a systematic and pragmatic framework for designing, modifying, and implementing multilevel interventions. Originally introduced in the public health field, the model has been successfully applied in recent years to develop interventions in diverse fields, including education, mental health, and social prevention. The six steps of this model, from problem definition and analysis to collecting evidence of effectiveness for large-scale implementation, provide complete coverage from design to implementation. The logical order of intervention development steps, as well as the pragmatic approach of this strategy, make it suitable for use in cases where practical guidance for intervention development is lacking. The recursive and nonlinear nature of this model is also important. Contrary to the superficial perception of numbered stages, intervention development in this framework is a dynamic, iterative, and flexible process. In practice, intervention designers repeatedly return to previous steps, revise the intervention based on evidence, and modify the final structure in response to field feedback. This cycle of redesign prevents the implementation of costly and inefficient interventions, making optimal use of limited resources.
A key feature of the 6SQuID model is the strong focus on stakeholder engagement throughout all stages of intervention development. In this process, stakeholder engagement not only helps improve the acceptability and effectiveness of the intervention but also provides a platform for incremental and modifiable design. Tools such as participatory design, formative evaluation, and continuous feedback play a pivotal role in this regard. Some strategies for engaging with stakeholders include building mutual trust, providing clear communication, and seeking feedback, as recommended by the International Association for Public Participation and the integrated framework for implementation research [29].
Cultural and organizational adaptability is another important advantage of the 6SQuID model. Since it focuses on the design path rather than prescribing fixed content, it has a high ability to adapt to different cultural, social, and organizational characteristics, especially in steps 2, 3, and 4, where analyzing the implementation context and using local feedback have a special place, allowing the designed intervention to adapt to environmental requirements. This model can be used as a dynamic and practical roadmap for designing behavioral, educational, or social interventions in a variety of contexts.
The 6SQuID model is not limited to a specific field and can be very useful, especially in situations where there is a need to design an intervention that is tailored to the socio-cultural context, stakeholder participation, and gradual testing. This model allows for continuous review and modification in steps 3-5 based on feedback, formative evaluation, and contextual conditions. Despite these advantages, the 6SQuID model has some limitations. It can be misinterpreted as a linear model, while the nature of intervention development is often complex, interactive, and nonlinear. Also, the quality of implementation of early stages such as context analysis and change mechanism design is highly dependent on the quality and scope of available evidence, and this can lead to design errors in contexts with poor data. Moreover, practical adaptation of the model to some cultural or institutional contexts may require redefining or combining steps. Finally, although the model emphasizes stakeholder participation, achieving effective participation faces structural and cultural challenges.
Conclusion
The 6SQuID framework offers a systematic, iterative, and pragmatic approach for developing educational, therapeutic, and social interventions. Its six-step structure—from problem definition to rigorous evaluation—provides comprehensive guidance for designing interventions that are contextually tailored, evidence-informed, and actively engage stakeholders. The framework’s flexibility enables adaptation across diverse cultural, organizational, and disciplinary settings, while its emphasis on formative evaluation and iterative refinement enhances feasibility, acceptability, and effectiveness. Despite potential challenges, including misinterpretation of its nonlinear nature and reliance on high-quality contextual evidence, 6SQuID remains a robust model for ensuring methodological rigor and practical relevance in intervention development. Researchers and policymakers are encouraged to adopt this framework to systematically design, implement, and evaluate interventions, thereby optimizing resource use and promoting sustainable outcomes.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank the Faculty of Psychology and Educational Sciences at Shahid Beheshti University for providing the conditions that facilitated this work.
References
- Bahiraei S, Amiri Jomi Lo R. [The effect of intervention programs on balance of individual with down syndrome: A systematic review (Persian)]. J Paramed Sci Rehabil. 2023; 11(4):107-24. [DOI:10.22038/jpsr.2023.58386.2264]
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: Update of medical research council guidance. BMJ. 2021; 374:n2061. [DOI:10.1136/bmj.n2061] [PMID]
- Mahmoudi H, Daneshmandi H, Shamsi Majelan A. [Intervention mapping; A framework to design health promotion interventions with an emphasis on physical activity: A review of Literature (Persian)]. J Paramed Sci Rehabil. 2023; 12(1):99-116. [DOI:10.22038/jpsr.2023.61609.2329]
- Wight D, Wimbush E, Jepson R, Doi L. Six steps in quality intervention development (6SQuID). J Epidemiol Community Health. 2016; 70(5):520-5. [DOI:10.1136/jech-2015-205952] [PMID]
- Guay B, Berinsky AJ, Pennycook G, Rand D. How to think about whether misinformation interventions work. Nat Hum Behav. 2023; 7(8):1231-3. [DOI:10.1038/s41562-023-01667-w] [PMID]
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. Int J Nurs Stud. 2024; 154:104705. [DOI:10.1016/j.ijnurstu.2024.104705] [PMID]
- Cham H, Lee H, Migunov I. Quasi-experimental designs for causal inference: An overview. Asia Pacific Educ Rev. 2024; 25(3):611-27. [DOI:10.1007/s12564-024-09981-2]
- Leroy JL, Frongillo EA, Kase BE, Alonso S, Chen M, Dohoo I, et al. Strengthening causal inference from randomised controlled trials of complex interventions. BMJ Glob Health. 2022; 7(6):e008597. [DOI:10.1136/bmjgh-2022-008597] [PMID]
- Colquhoun HL, Squires JE, Kolehmainen N, Fraser C, Grimshaw JM. Methods for designing interventions to change healthcare professionals' behaviour: A systematic review. Implement Sci. 2017; 12(1):30. [DOI:10.1186/s13012-017-0560-5] [PMID]
- Bond C, Lancaster GA, Campbell M, Chan C, Eddy S, Hopewell S, et al. Pilot and feasibility studies: Extending the conceptual framework. Pilot Feasibility Stud. 2023; 9(1):24. [DOI:10.1186/s40814-023-01233-1] [PMID]
- O'Cathain A, Croot L, Sworn K, Duncan E, Rousseau N, Turner K, Yardley L, Hoddinott P. Taxonomy of approaches to developing interventions to improve health: A systematic methods overview. Pilot Feasibility Stud. 2019; 5:41. [DOI:10.1186/s40814-019-0425-6] [PMID]
- Shalani B, Azadfallah P, Farahani H, Roshan R, Esrafilian F. [Practical steps in designing therapeutic, interventional and educational packages in psychological researches: Intervention mapping approach (Persian)]. Clin Psychol Pers. 2022; 20(1):177-97. [DOI:10.22070/cpap.2022.16313.1235]
- Hansen S, Kanning M, Lauer R, Steinacker JM, Schlicht W. MAP-IT: A practical tool for planning complex behavior modification interventions. Health Promot Pract. 2017; 18(5):696-705. [DOI:10.1177/1524839917710454] [PMID]
- Janols R, Lindgren H. A method for co-designing theory-based behavior change systems for health promotion. Stud Health Technol Inf. 2017; 235:368-72. [DOI:10.3233/978-1-61499-753-5-368]
- van Rooyen H, Essack Z, Rochat T, Wight D, Knight L, Bland R, et al. Taking HIV testing to families: Designing a family-based intervention to facilitate HIV testing, disclosure, and intergenerational communication. Front Public Health. 2016; 4:154. [DOI:10.3389/fpubh.2016.00154] [PMID]
- Pringle J, Doi L, Jindal-Snape D, Jepson R, McAteer J. Adolescents and health-related behaviour: using a framework to develop interventions to support positive behaviours. Pilot Feasibility Stud. 2018; 4:69. [DOI:10.1186/s40814-018-0259-7] [PMID]
- Hartley JE, McAteer J, Doi L, Jepson R. CARE: The development of an intervention for kinship carers with teenage children. Qual Soc Work. 2019; 18(6):926-43. [DOI:10.1177/1473325018783823] [PMID]
- Sinclair JMA, Dutey-Magni PF, Anderson AS, Baird J, Barker ME, Cutress RI, et al. A context-specific digital alcohol brief intervention in symptomatic breast clinics (abreast of health): Development and usability study. JMIR Res Protoc. 2020; 9(1):e14580. [DOI:10.2196/14580] [PMID]
- Tirman L, Biggs H, Morrison K, Manner J, Sivaramakrishnan D, Baker G, et al. Stand up for health: Programme theory for an intervention to reduce sedentary behaviour in contact centres. Eval Program Plann. 2021; 89:102002. [DOI:10.1016/j.evalprogplan.2021.102002] [PMID]
- Funnell SC, Rogers PJ. Purposeful program theory: Effective use of theories of change and logic models. Hoboken: John Wiley & Sons; 2011. [Link]
- Islam KF, Awal A, Mazumder H, Munni UR, Majumder K, Afroz K, et al. Social cognitive theory-based health promotion in primary care practice: A scoping review. Heliyon. 2023; 9(4):e14889. [DOI:10.1016/j.heliyon.2023.e14889] [PMID]
- Prestwich A, Kenworthy J, Conner M. Health behavior change: Theories, methods and interventions. Oxfordshire: Routledge; 2024. [DOI:10.4324/9781003302414]
- Hashemzadeh M, Rahimi A, Zare-Farashbandi F, Alavi-Naeini AM, Daei A. Transtheoretical model of health behavioral change: A systematic review. Iran J Nurs Midwifery Res. 2019; 24(2):83-90. [DOI:10.4103/ijnmr.IJNMR_94_17] [PMID]
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. 2nd Edition. Chichester: John Wiley & Sons; 2019. [DOI:10.1002/9781119536604]
- Lorenc T, Oliver K. Adverse effects of public health interventions: A conceptual framework. J Epidemiol Community Health. 2014; 68(3):288-90. [DOI:10.1136/jech-2013-203118] [PMID]
- Chan AW, Boutron I, Hopewell S, Moher D, Schulz KF, Collins GS, et al. SPIRIT 2025 statement: Updated guideline for protocols of randomised trials. Lancet. 2025; 405(10491):e19-27. [DOI:10.1016/S0140-6736(25)00770-6]
- Wald N. Efficacy and effectiveness. J Med Screen. 2021; 28(2):57-8. [DOI:10.1177/0969141321995223] [PMID]
- Burches E, Burches M. Efficacy, effectiveness and efficiency in the health care: The need for an agreement to clarify its meaning. Int Arch Public Health Commun Med. 2020; 4:035. [DOI:10.23937/2643-4512/1710035]
- Holcomb J, Ferguson GM, Sun J, Walton GH, Highfield L. Stakeholder engagement in adoption, implementation, and sustainment of an evidence-based intervention to increase mammography adherence among low-income women. J Cancer Educ. 2022; 37(5):1486-95. [DOI:10.1007/s13187-021-01988-2] [PMID]
Type of Study: Research |
Subject:
Educational Psychology
Received: 2025/05/4 | Accepted: 2025/09/19 | Published: 2025/09/19
Received: 2025/05/4 | Accepted: 2025/09/19 | Published: 2025/09/19
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |