Thu, Feb 19, 2026
[Archive]
Volume 2, Issue 3 (Spring 2024)
CPR 2024, 2(3): 163-172 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Esmailpour Moalem A, Shafipour V, Shafipour L, Jafari H. Factors Associated With Nurses’ Professional Autonomy: A Narrative Review. CPR 2024; 2 (3) :163-172
URL: http://cpr.mazums.ac.ir/article-1-131-en.html
URL: http://cpr.mazums.ac.ir/article-1-131-en.html
Department of Medical Surgical Nursing, Traditional and Complementary Medicine Research Center, School of Nursing and Midwifery, Mazandaran University of Medical Sciences, Sari, Iran.
Full-Text [PDF 871 kb]
(1025 Downloads)
| Abstract (HTML) (1002 Views)
Quality assessment
In this narrative review, an informal evaluation of the studies included was carried out to assess their methodological rigor and relevance. The assessment considered aspects such as the study design, the selection of participants, the methods of data collection, and the measures to measure the results. Although no formal quality assessment tool was used, the studies were assessed based on their clarity and relevance to the research topic. Higher-quality studies were prioritized in synthesizing findings to ensure the review provides a comprehensive literature overview.
Data extraction
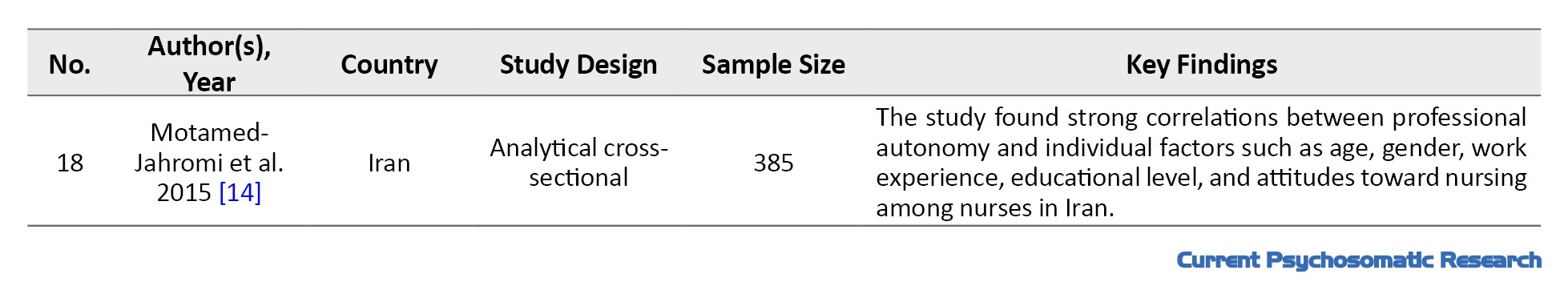
A summary of each study, including study objectives, study design methodology, details of participants, data collection methods, and study results, was prepared to extract the basic data relevant to the research question. The extracted data also included key information such as authors, year of publication, sample size, key findings, and country of origin. This complex data set has been structured in tables to facilitate comparison and analysis across studies.
Results
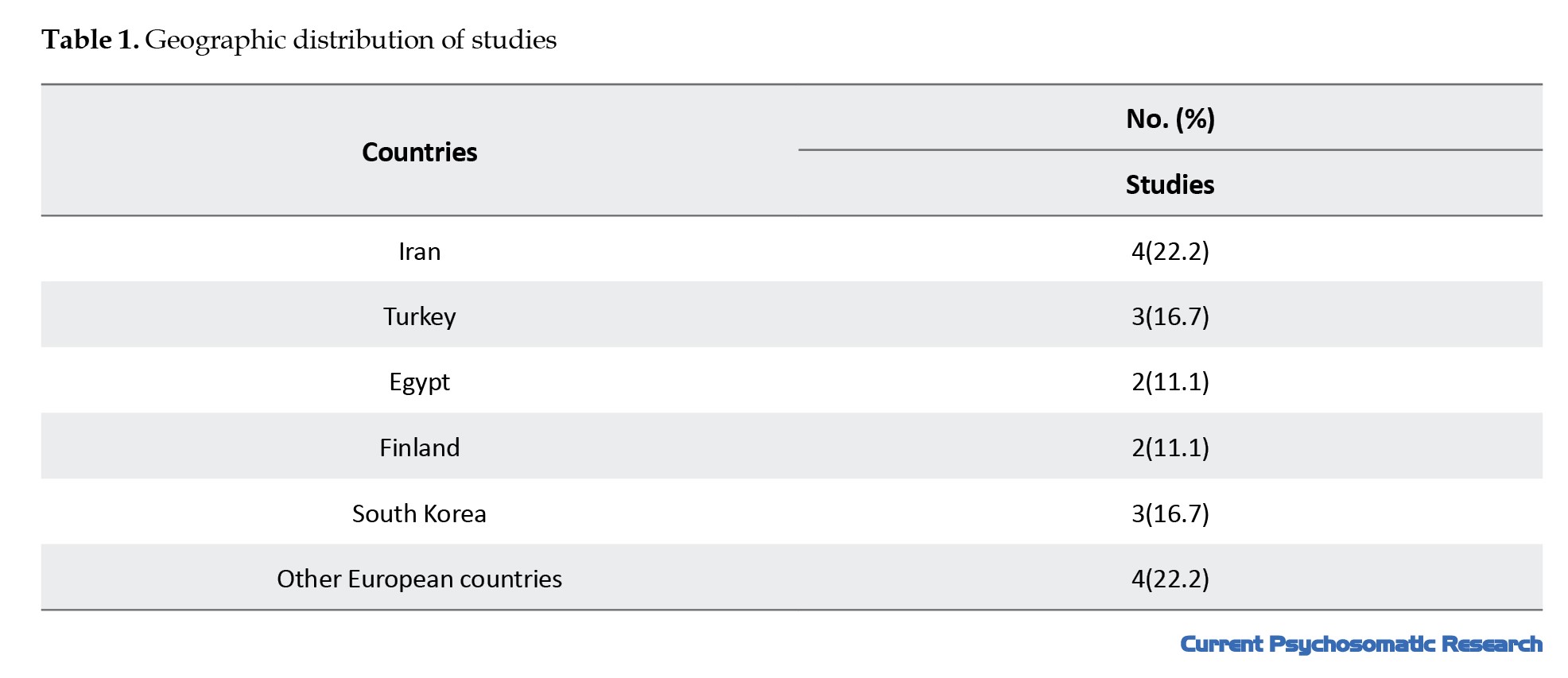
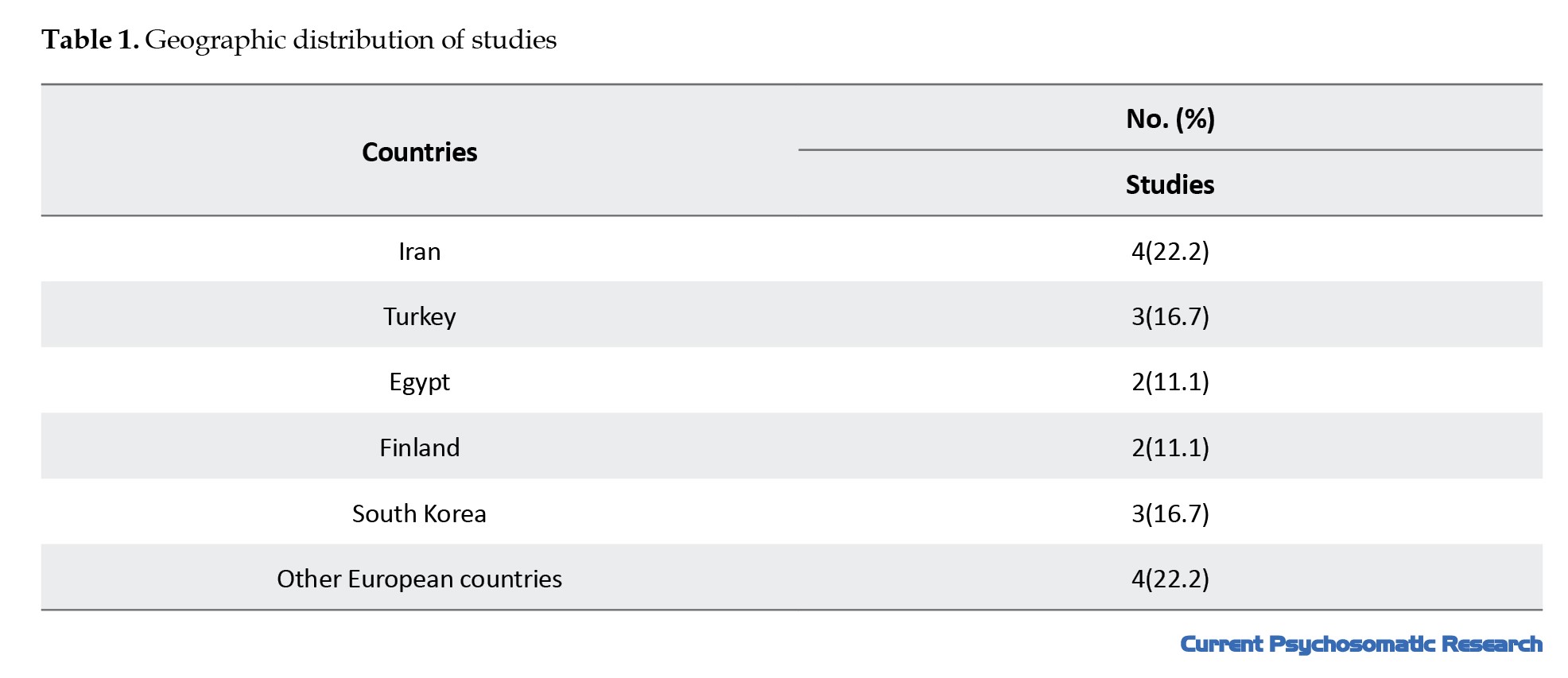
This review article analyzes studies conducted from January 2010 to December 2024. Ultimately, 18 studies were included in this review, which included descriptive quantitative research on diverse groups of nurses in hospitals and health centers. Most studies were conducted in Iran, Turkey, Egypt, Finland, South Korea, and several European countries (Table 1).
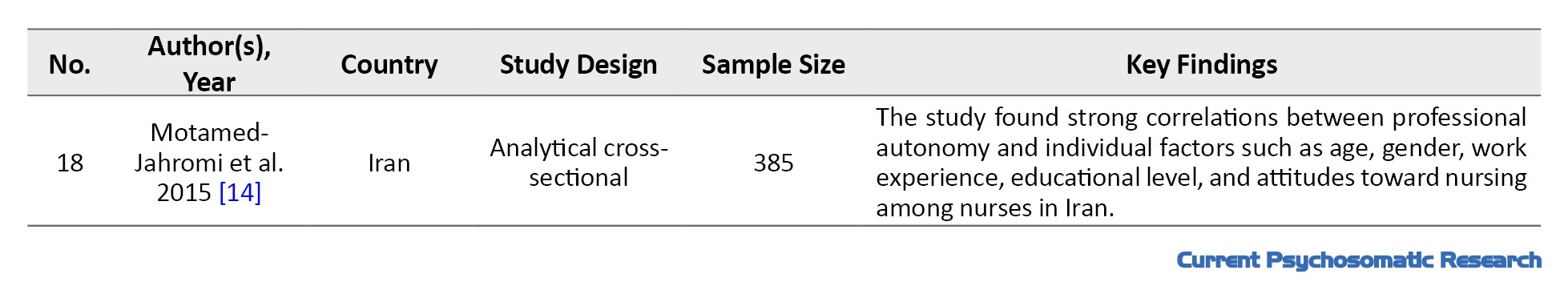
The characteristics of eligible studies are presented in Table 2.

The sample sizes in these studies varied, typically from 100 to 1000 nurses from intensive care units, emergency departments, oncology, and pediatrics. Furthermore, in these studies, the age range of caregivers was generally between 25 and 55 years.
The studies identified several key factors associated with nurses’ professional autonomy. To better understand these factors, they can be divided into six different groups: Individual factors (e.g. age and education), organizational factors (e.g. management support and policies), collaborative factors (e.g. teamwork and interprofessional relationships), professional development factors (e.g. continuing education), psychosocial factors (e.g. job satisfaction and emotional well-being), and external factors (e.g. health system structure). This classification allows for a comprehensive examination of how these various elements work together to shape the autonomy that nurses experience in their practice.
Individual factors
Age and experience: Older nurses or those with more experience may have more professional autonomy [13, 14].
Level of education: Higher education can improve nurses’ decision-making skills and confidence.
Self-efficacy: Nurses’ beliefs in their abilities can influence their professional autonomy [11, 15].
Organizational factors
Support from nursing staff: Nursing managers and leaders can create an environment conducive to professional autonomy [12, 16].
Work environment: A positive work culture and a supportive organizational structure can increase the independence of nurses [17].
Policies and regulations: Clear and supportive guidelines for nursing practice can empower nurses [18].
Collaborative factors
Interprofessional collaboration: Effective communication and collaboration with physicians and other healthcare professionals can increase the autonomy of nursing staff [10].
Teamwork: A collaborative team environment can help nurses make independent decisions [12].
Professional development factors
Continuing education: Opportunities for ongoing training and education can improve nurses’ skills and confidence [11].
Role clarity: Clearly defined roles and responsibilities can help nurses understand their scope of practice [19, 20].
Psychosocial factors
Job satisfaction: Higher job satisfaction is often associated with greater job autonomy.
Emotional well-being: Burnout, stress, and ethical pressures can negatively impact a nurse’s sense of autonomy [21].
External factors
Health system structure: The overall structure of the health system, including bureaucratic constraints, can impact the autonomy of nursing staff [22].
Cultural attitudes: Societal perceptions of nursing roles can influence the level of independence nurses experience in practice [23].
These categories include a range of factors that may influence nurses’ professional independence. Understanding these factors is critical to developing strategies to improve autonomy in nursing practice, ultimately leading to better job satisfaction, retention, and patient care outcomes.
Discussion
The findings of this review underline the multi-faceted nature of the factors affecting the professional autonomy of nurses, and they are consistent with and critically different from the previous literature. Below, we will elaborate on the clinical implications, synthesize key comparisons, and address the existing studies’ consistency and inconsistencies.
Our analysis corroborates the pivotal role of organizational support in fostering nurses’ autonomy, as demonstrated in multiple studies [24, 25, 26]. For instance, AbdolAmaleki et al [27] and Labrague et al. [28] emphasized that supportive leadership and participative decision-making significantly enhance nurses’ ability to exercise autonomous judgment, which aligns with our observation that collaborative practices and clear policies are critical enablers [27, 28]. Similarly, the positive correlation between educational attainment and autonomy resonates with findings from Hsiu-Ying et al [19]. and Mrayyan et al. [26] who identified education as a cornerstone for clinical decision-making skills [19, 26]. This synergy highlights the universal importance of institutional investments in continuing education and leadership development.
However, our review reveals notable discrepancies regarding the interplay between moral distress and autonomy. While Borhani et al. [29] and Papathanassoglou et al. [10] reported that diminished autonomy exacerbates moral distress [10, 29], our findings suggest a paradoxical relationship. For example, a study by Abdolmaleki et al. [27] found that nurses with higher autonomy in high-stakes environments (e.g. emergency departments) often face greater moral distress due to insufficient systemic support [27]. This divergence may stem from contextual factors such as cultural attitudes toward nursing roles or variability in interprofessional collaboration across healthcare systems. In Iran and Turkey, hierarchical structures often limit nurses’ authority despite formal autonomy, creating conflict between responsibility and resource constraints [22, 30].
Our results align with global studies demonstrating that autonomy directly enhances job satisfaction [22, 25]. For instance, a cross-sectional study in Turkey reported a significant positive correlation between autonomy and satisfaction, mirroring our conclusion that empowered nurses exhibit higher retention rates and workplace morale [25]. This consistency underscores autonomy as a universal driver of nurse well-being.
While our review emphasizes collaborative teamwork as a catalyst for autonomy, findings from Benha University Hospital revealed that 73.3% of nurses perceived low organizational support, correlating with moderate autonomy levels [25]. This finding contrasts with studies in Finland and South Korea, where participatory leadership models yielded higher autonomy [13]. The discrepancy may reflect resource allocation disparities or differences in managerial training across regions.
A striking divergence emerges in the relationship between autonomy and moral distress. Whereas Falatah & Alif linked low autonomy to burnout [31], our analysis identified contexts where high autonomy without adequate institutional backing increased moral distress [30]. For example, Iranian emergency nurses with greater decision-making authority reported intensified distress due to unmet support from physicians [27, 30]. This result suggests that autonomy’s benefits depend on systemic enablers such as interprofessional respect and resource accessibility.
Furthermore, the challenges to achieving autonomy identified in our review are echoed in other studies, particularly in the context of nursing in Iran. Systematic reviews and qualitative studies highlight barriers such as inadequate managerial support, heavy workloads, and poorly defined professional boundaries. For example, a study by Jafari et al. emphasizes that unclear organizational policies and insufficient collaboration between nurses and other healthcare professionals hinder the realization of professional autonomy [11]. Similarly, a study on nursing challenges in Iran reveals that hierarchical structures and physician dominance in decision-making processes significantly limit nurses’ ability to act autonomously [32-34]. These systemic issues align with broader global challenges, such as resource constraints and a lack of participatory leadership models [32]. Without addressing these barriers—both at the organizational and policy levels—efforts to enhance nurses’ autonomy may remain ineffective. Addressing these challenges requires targeted interventions, including improved managerial training and fostering interprofessional respect within healthcare teams.
Conclusion
The results of our review highlight the importance of fostering a supportive work environment for nurses. By enhancing organizational support and implementing clear policies, healthcare institutions can empower nurses to exercise greater autonomy. This, in turn, is likely to lead to improved job satisfaction, retention rates, and ultimately better patient care outcomes. Nursing leaders and administrators must recognize the role of continuous education and professional development in promoting nurses’ confidence and decision-making abilities.
The strength of this study lies in its comprehensive analysis of various research findings, which provides valuable insights into how these factors interact to shape the autonomy nurses experience in different clinical settings. However, the study also has limitations, such as the possibility of publication bias and the variability of methods in the reviewed studies, which may affect the generalizability of the results. Future research should focus on longitudinal studies to better understand the causal relationships between these factors and professional autonomy and examine innovative strategies to improve nurses’ independence in practice.
Future studies should investigate cultural mediators of autonomy using cross-national comparative designs to address these complexities and understand how different healthcare systems influence nurses’ professional autonomy. Additionally, developing intervention studies is essential to test strategies that balance autonomy with systemic support, such as implementing mentorship programs for junior nurses to foster their confidence and decision-making skills. Furthermore, exploring gender-specific dynamics in nursing autonomy is crucial, as preliminary data suggest that male nurses report higher levels of autonomy in specific contexts. By examining these areas, researchers can provide valuable insights that inform policy and practice to enhance nurses’ professional autonomy across diverse settings.
This review highlights the dual role of autonomy as both an empowerment tool and a potential stressor, contingent on organizational and cultural contexts. By addressing these nuances, healthcare systems can better leverage autonomy to improve nurse retention, patient care quality, and ethical practice.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Atefe Esmailpour Moalem; Data analysis and interpretation: Atefe Esmailpour Moalem and Hedayat Jafari; Drafting of the manuscript: Vida Shafipour; Critical revision of the manuscript for important intellectual content: Leila Shafipour; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate the support of Mazandaran University of Medical Sciences, Sari, Iran, which provided the necessary resources for conducting this comprehensive literature review.
References
Full-Text: (429 Views)
Introduction
Professional autonomy is a multi-faceted concept in nursing, including the ability to independently make informed decisions based on professional knowledge and judgment [1]. In nursing, professional autonomy is understood as the ability to make informed decisions based on one’s professional experience and judgment and to act independently about the care of patients [2]. Independence and autonomy are often used interchangeably; however, they possess distinct ings crucial for understanding their implications in professional practice. Independence refers to a state of self-sufficiency where individuals do not rely on external support. At the same time, autonomy emphasizes self-governance and decision-making based on personal values, even within interdependent relationships. Recognizing these differences is essential for exploring the factors influencing nurses’ professional autonomy, as it highlights the importance of self-determination and collaborative decision-making in nursing practice [3].
Autonomy is essential for achieving professional status and recognition, as it directly impacts job satisfaction, retention, and quality of care [4, 5]. Research shows that independent nurses are more satisfied with their jobs and are likelier to remain in the health care sector than independent colleagues [6]. Conversely, low levels of autonomy are associated with adverse outcomes such as burnout, depression, overwork, absenteeism, and moral distress [7]. Improving nurses’ professional autonomy can directly impact the quality of their working lives, reducing turnover and increasing job satisfaction, ultimately leading to better quality care [5].
The attainment of independence has always been one of the greatest challenges in nursing [8]. Research has identified several key factors concerning the autonomy of nurses, including education and training, support to management, regulatory frameworks, and professional development [9]. A study by Papathanassiou et al. highlights the development of the role of nurses as one of the key strategies for improving professional independence [10]. Another study examined the relationship between educational attainment and professional autonomy and found that nurses with university qualifications tend to have more independence and commitment to their profession [11].
While the existing systematic reviews provide valuable insights into the profession’s autonomy in the nursing sector, their scope is often limited to specific dimensions or contexts, leaving a significant gap in understanding the wider interrelated factors that influence autonomy. For example, Pursio et al. carried out an integrated review highlighting organizational factors such as leadership and cooperation as key determinants of independence. However, the review did not fully address the role of external influences, such as regulatory frameworks or health policies, which are crucial in shaping the development of professional autonomy in the various health systems [12].
Similarly, Rouhi-Balasi et al. carried out a qualitative synthesis examining the conceptual aspects of professional autonomy, focusing on issues such as professional competence and decision-making. Although the study provided a rich theoretical perspective, it did not offer practical recommendations on promoting autonomy in a diverse and dynamic healthcare setting. This limitation highlights the need for further research to bridge the gap between theoretical knowledge and practical strategies [5].
These reviews are valuable but often do not provide a comprehensive view of the interaction between individual characteristics (e.g. training and experience), organizational structures (e.g. managerial support and team dynamics), and external factors (e.g. legal and policy frameworks). Addressing these shortcomings is essential for creating a comprehensive framework that can guide efforts to increase the autonomy of professional practice in the nursing profession. This narrative review aims to synthesize the findings of various studies to provide a more comprehensive understanding of the factors that influence professional autonomy, and, thus, to inform strategies to improve the retention of nurses, job satisfaction, and patient outcomes.
This narrative review aims to fill this gap by summarizing the existing literature and identifying the key factors in the context of the autonomy of nurses. The objective of this review, which looks at recent studies in a wide range of settings and populations, is to provide actionable insights into the factors that influence nurses’ professional autonomy. The ultimate objective is to improve patient performance by reaping the benefits of the autonomy of healthcare professionals. The study will contribute to the existing body of knowledge by providing a comprehensive overview of the factors affecting professional autonomy, thus informing strategies for promoting greater professional autonomy in nursing.
Materials and Methods
This narrative review examines factors related to nurses’ professional autonomy per the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines on the preferred narrative review reporting items.
Search strategy
A comprehensive search strategy has been used to identify the relevant studies. The search was made using several databases in both Persian and English. Reliable sources such as Iranian Research Institute for Information Science and Technology (IranDoc), Magiran, and Scientific Information Database (SID) were used for the Persian search. Established databases, including CINAHL, Scopus, the Web of Science, and PubMed, were accessible for English-language search. The search terms used included “professional autonomy”, “nurses”, “clinical decision-making”, “nursing staff”, and “hospital”. These terms were combined using Boolean operators (AND, OR) to ensure a thorough examination of the literature. For example, the search string could be structured as follows: (“Professional autonomy” OR “autonomy in nursing”) AND (“nurses” OR “nursing staff”) AND (“clinical decision-making” OR “nursing practice”) AND (“hospital” OR “healthcare setting”). A Google Scholar search was also conducted to identify any further relevant articles. To ensure a comprehensive search, the reference lists of included articles were also reviewed to identify additional studies.
Inclusion criteria
The review included observational studies published in English or Persian, which looked at factors related to nurses’ professional autonomy over a defined period. Only studies that provided empirical data on these factors have been included. Articles were excluded if they were not available in full, were aimed at other health professionals or students, or did not specifically address the factors affecting the professional independence of nurses. This approach ensured that the review was based on relevant and high-quality literature that directly contributes to the understanding of the dynamics of the autonomy of the profession in the nursing sector.
Data collection
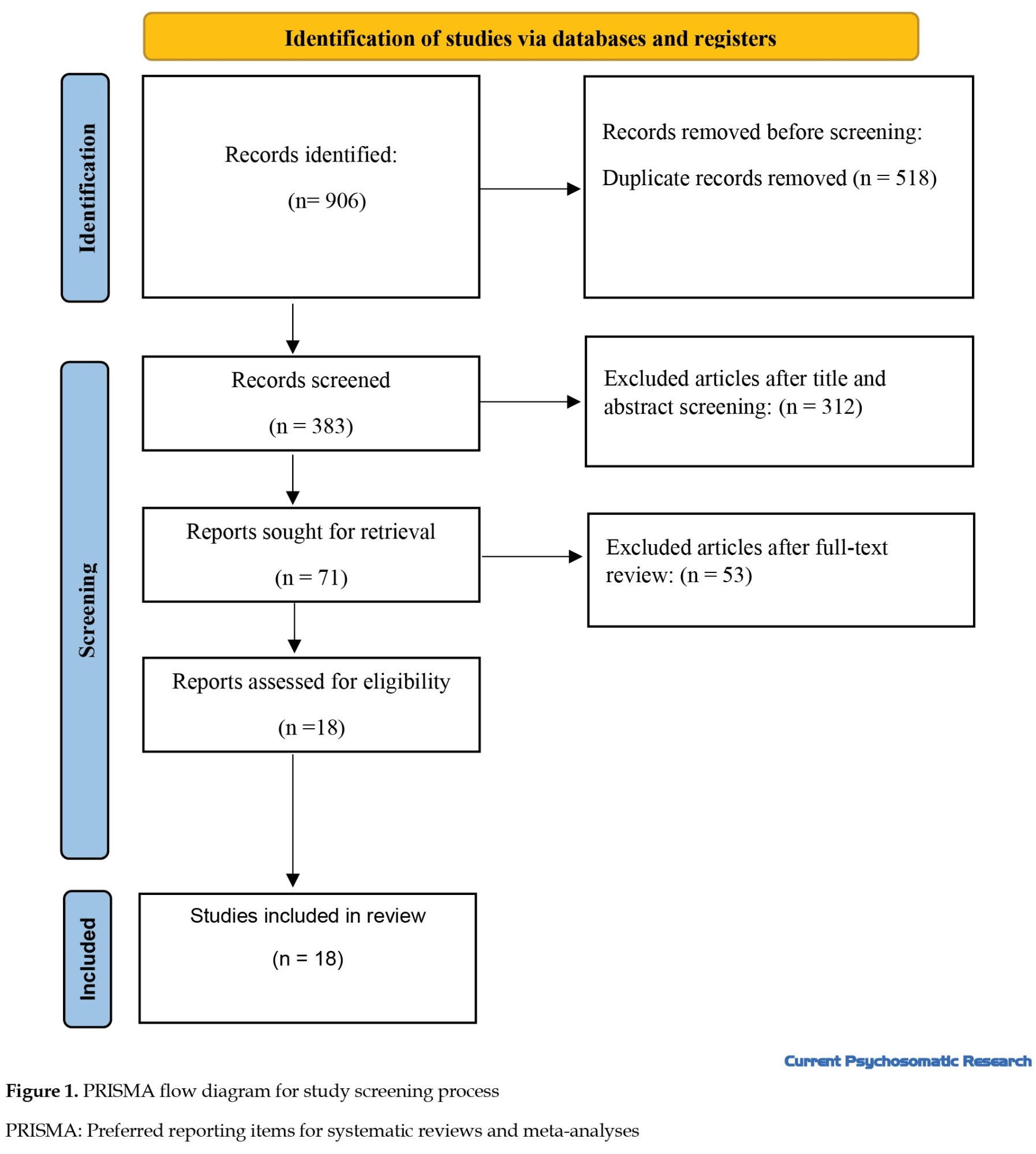
The referral process started with the identification of 906 potentially pertinent studies. After the deletion of duplicates, there were 383 studies. In the second phase, the titles and abstracts were reviewed, and 312 studies were excluded from the review as not meeting the objectives or inclusion criteria. Further studies have been identified by reference to the retained articles. Finally, 71 studies were advanced to the third stage, where two research team members independently evaluated them to minimize potential bias. This full-text analysis resulted in the exclusion of 53 additional studies. Altogether, 18 articles were selected directly relevant to the study objectives. These articles have been peer-reviewed by two members of the research team, who confirmed their relevance for the analysis. In the event of disagreement between researchers, discussions would have been held with third parties; however, the full agreement of both researchers made this unnecessary (Figure 1).
Professional autonomy is a multi-faceted concept in nursing, including the ability to independently make informed decisions based on professional knowledge and judgment [1]. In nursing, professional autonomy is understood as the ability to make informed decisions based on one’s professional experience and judgment and to act independently about the care of patients [2]. Independence and autonomy are often used interchangeably; however, they possess distinct ings crucial for understanding their implications in professional practice. Independence refers to a state of self-sufficiency where individuals do not rely on external support. At the same time, autonomy emphasizes self-governance and decision-making based on personal values, even within interdependent relationships. Recognizing these differences is essential for exploring the factors influencing nurses’ professional autonomy, as it highlights the importance of self-determination and collaborative decision-making in nursing practice [3].
Autonomy is essential for achieving professional status and recognition, as it directly impacts job satisfaction, retention, and quality of care [4, 5]. Research shows that independent nurses are more satisfied with their jobs and are likelier to remain in the health care sector than independent colleagues [6]. Conversely, low levels of autonomy are associated with adverse outcomes such as burnout, depression, overwork, absenteeism, and moral distress [7]. Improving nurses’ professional autonomy can directly impact the quality of their working lives, reducing turnover and increasing job satisfaction, ultimately leading to better quality care [5].
The attainment of independence has always been one of the greatest challenges in nursing [8]. Research has identified several key factors concerning the autonomy of nurses, including education and training, support to management, regulatory frameworks, and professional development [9]. A study by Papathanassiou et al. highlights the development of the role of nurses as one of the key strategies for improving professional independence [10]. Another study examined the relationship between educational attainment and professional autonomy and found that nurses with university qualifications tend to have more independence and commitment to their profession [11].
While the existing systematic reviews provide valuable insights into the profession’s autonomy in the nursing sector, their scope is often limited to specific dimensions or contexts, leaving a significant gap in understanding the wider interrelated factors that influence autonomy. For example, Pursio et al. carried out an integrated review highlighting organizational factors such as leadership and cooperation as key determinants of independence. However, the review did not fully address the role of external influences, such as regulatory frameworks or health policies, which are crucial in shaping the development of professional autonomy in the various health systems [12].
Similarly, Rouhi-Balasi et al. carried out a qualitative synthesis examining the conceptual aspects of professional autonomy, focusing on issues such as professional competence and decision-making. Although the study provided a rich theoretical perspective, it did not offer practical recommendations on promoting autonomy in a diverse and dynamic healthcare setting. This limitation highlights the need for further research to bridge the gap between theoretical knowledge and practical strategies [5].
These reviews are valuable but often do not provide a comprehensive view of the interaction between individual characteristics (e.g. training and experience), organizational structures (e.g. managerial support and team dynamics), and external factors (e.g. legal and policy frameworks). Addressing these shortcomings is essential for creating a comprehensive framework that can guide efforts to increase the autonomy of professional practice in the nursing profession. This narrative review aims to synthesize the findings of various studies to provide a more comprehensive understanding of the factors that influence professional autonomy, and, thus, to inform strategies to improve the retention of nurses, job satisfaction, and patient outcomes.
This narrative review aims to fill this gap by summarizing the existing literature and identifying the key factors in the context of the autonomy of nurses. The objective of this review, which looks at recent studies in a wide range of settings and populations, is to provide actionable insights into the factors that influence nurses’ professional autonomy. The ultimate objective is to improve patient performance by reaping the benefits of the autonomy of healthcare professionals. The study will contribute to the existing body of knowledge by providing a comprehensive overview of the factors affecting professional autonomy, thus informing strategies for promoting greater professional autonomy in nursing.
Materials and Methods
This narrative review examines factors related to nurses’ professional autonomy per the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines on the preferred narrative review reporting items.
Search strategy
A comprehensive search strategy has been used to identify the relevant studies. The search was made using several databases in both Persian and English. Reliable sources such as Iranian Research Institute for Information Science and Technology (IranDoc), Magiran, and Scientific Information Database (SID) were used for the Persian search. Established databases, including CINAHL, Scopus, the Web of Science, and PubMed, were accessible for English-language search. The search terms used included “professional autonomy”, “nurses”, “clinical decision-making”, “nursing staff”, and “hospital”. These terms were combined using Boolean operators (AND, OR) to ensure a thorough examination of the literature. For example, the search string could be structured as follows: (“Professional autonomy” OR “autonomy in nursing”) AND (“nurses” OR “nursing staff”) AND (“clinical decision-making” OR “nursing practice”) AND (“hospital” OR “healthcare setting”). A Google Scholar search was also conducted to identify any further relevant articles. To ensure a comprehensive search, the reference lists of included articles were also reviewed to identify additional studies.
Inclusion criteria
The review included observational studies published in English or Persian, which looked at factors related to nurses’ professional autonomy over a defined period. Only studies that provided empirical data on these factors have been included. Articles were excluded if they were not available in full, were aimed at other health professionals or students, or did not specifically address the factors affecting the professional independence of nurses. This approach ensured that the review was based on relevant and high-quality literature that directly contributes to the understanding of the dynamics of the autonomy of the profession in the nursing sector.
Data collection
The referral process started with the identification of 906 potentially pertinent studies. After the deletion of duplicates, there were 383 studies. In the second phase, the titles and abstracts were reviewed, and 312 studies were excluded from the review as not meeting the objectives or inclusion criteria. Further studies have been identified by reference to the retained articles. Finally, 71 studies were advanced to the third stage, where two research team members independently evaluated them to minimize potential bias. This full-text analysis resulted in the exclusion of 53 additional studies. Altogether, 18 articles were selected directly relevant to the study objectives. These articles have been peer-reviewed by two members of the research team, who confirmed their relevance for the analysis. In the event of disagreement between researchers, discussions would have been held with third parties; however, the full agreement of both researchers made this unnecessary (Figure 1).
Quality assessment
In this narrative review, an informal evaluation of the studies included was carried out to assess their methodological rigor and relevance. The assessment considered aspects such as the study design, the selection of participants, the methods of data collection, and the measures to measure the results. Although no formal quality assessment tool was used, the studies were assessed based on their clarity and relevance to the research topic. Higher-quality studies were prioritized in synthesizing findings to ensure the review provides a comprehensive literature overview.
Data extraction
A summary of each study, including study objectives, study design methodology, details of participants, data collection methods, and study results, was prepared to extract the basic data relevant to the research question. The extracted data also included key information such as authors, year of publication, sample size, key findings, and country of origin. This complex data set has been structured in tables to facilitate comparison and analysis across studies.
Results
This review article analyzes studies conducted from January 2010 to December 2024. Ultimately, 18 studies were included in this review, which included descriptive quantitative research on diverse groups of nurses in hospitals and health centers. Most studies were conducted in Iran, Turkey, Egypt, Finland, South Korea, and several European countries (Table 1).
The characteristics of eligible studies are presented in Table 2.

The sample sizes in these studies varied, typically from 100 to 1000 nurses from intensive care units, emergency departments, oncology, and pediatrics. Furthermore, in these studies, the age range of caregivers was generally between 25 and 55 years.
The studies identified several key factors associated with nurses’ professional autonomy. To better understand these factors, they can be divided into six different groups: Individual factors (e.g. age and education), organizational factors (e.g. management support and policies), collaborative factors (e.g. teamwork and interprofessional relationships), professional development factors (e.g. continuing education), psychosocial factors (e.g. job satisfaction and emotional well-being), and external factors (e.g. health system structure). This classification allows for a comprehensive examination of how these various elements work together to shape the autonomy that nurses experience in their practice.
Individual factors
Age and experience: Older nurses or those with more experience may have more professional autonomy [13, 14].
Level of education: Higher education can improve nurses’ decision-making skills and confidence.
Self-efficacy: Nurses’ beliefs in their abilities can influence their professional autonomy [11, 15].
Organizational factors
Support from nursing staff: Nursing managers and leaders can create an environment conducive to professional autonomy [12, 16].
Work environment: A positive work culture and a supportive organizational structure can increase the independence of nurses [17].
Policies and regulations: Clear and supportive guidelines for nursing practice can empower nurses [18].
Collaborative factors
Interprofessional collaboration: Effective communication and collaboration with physicians and other healthcare professionals can increase the autonomy of nursing staff [10].
Teamwork: A collaborative team environment can help nurses make independent decisions [12].
Professional development factors
Continuing education: Opportunities for ongoing training and education can improve nurses’ skills and confidence [11].
Role clarity: Clearly defined roles and responsibilities can help nurses understand their scope of practice [19, 20].
Psychosocial factors
Job satisfaction: Higher job satisfaction is often associated with greater job autonomy.
Emotional well-being: Burnout, stress, and ethical pressures can negatively impact a nurse’s sense of autonomy [21].
External factors
Health system structure: The overall structure of the health system, including bureaucratic constraints, can impact the autonomy of nursing staff [22].
Cultural attitudes: Societal perceptions of nursing roles can influence the level of independence nurses experience in practice [23].
These categories include a range of factors that may influence nurses’ professional independence. Understanding these factors is critical to developing strategies to improve autonomy in nursing practice, ultimately leading to better job satisfaction, retention, and patient care outcomes.
Discussion
The findings of this review underline the multi-faceted nature of the factors affecting the professional autonomy of nurses, and they are consistent with and critically different from the previous literature. Below, we will elaborate on the clinical implications, synthesize key comparisons, and address the existing studies’ consistency and inconsistencies.
Our analysis corroborates the pivotal role of organizational support in fostering nurses’ autonomy, as demonstrated in multiple studies [24, 25, 26]. For instance, AbdolAmaleki et al [27] and Labrague et al. [28] emphasized that supportive leadership and participative decision-making significantly enhance nurses’ ability to exercise autonomous judgment, which aligns with our observation that collaborative practices and clear policies are critical enablers [27, 28]. Similarly, the positive correlation between educational attainment and autonomy resonates with findings from Hsiu-Ying et al [19]. and Mrayyan et al. [26] who identified education as a cornerstone for clinical decision-making skills [19, 26]. This synergy highlights the universal importance of institutional investments in continuing education and leadership development.
However, our review reveals notable discrepancies regarding the interplay between moral distress and autonomy. While Borhani et al. [29] and Papathanassoglou et al. [10] reported that diminished autonomy exacerbates moral distress [10, 29], our findings suggest a paradoxical relationship. For example, a study by Abdolmaleki et al. [27] found that nurses with higher autonomy in high-stakes environments (e.g. emergency departments) often face greater moral distress due to insufficient systemic support [27]. This divergence may stem from contextual factors such as cultural attitudes toward nursing roles or variability in interprofessional collaboration across healthcare systems. In Iran and Turkey, hierarchical structures often limit nurses’ authority despite formal autonomy, creating conflict between responsibility and resource constraints [22, 30].
Our results align with global studies demonstrating that autonomy directly enhances job satisfaction [22, 25]. For instance, a cross-sectional study in Turkey reported a significant positive correlation between autonomy and satisfaction, mirroring our conclusion that empowered nurses exhibit higher retention rates and workplace morale [25]. This consistency underscores autonomy as a universal driver of nurse well-being.
While our review emphasizes collaborative teamwork as a catalyst for autonomy, findings from Benha University Hospital revealed that 73.3% of nurses perceived low organizational support, correlating with moderate autonomy levels [25]. This finding contrasts with studies in Finland and South Korea, where participatory leadership models yielded higher autonomy [13]. The discrepancy may reflect resource allocation disparities or differences in managerial training across regions.
A striking divergence emerges in the relationship between autonomy and moral distress. Whereas Falatah & Alif linked low autonomy to burnout [31], our analysis identified contexts where high autonomy without adequate institutional backing increased moral distress [30]. For example, Iranian emergency nurses with greater decision-making authority reported intensified distress due to unmet support from physicians [27, 30]. This result suggests that autonomy’s benefits depend on systemic enablers such as interprofessional respect and resource accessibility.
Furthermore, the challenges to achieving autonomy identified in our review are echoed in other studies, particularly in the context of nursing in Iran. Systematic reviews and qualitative studies highlight barriers such as inadequate managerial support, heavy workloads, and poorly defined professional boundaries. For example, a study by Jafari et al. emphasizes that unclear organizational policies and insufficient collaboration between nurses and other healthcare professionals hinder the realization of professional autonomy [11]. Similarly, a study on nursing challenges in Iran reveals that hierarchical structures and physician dominance in decision-making processes significantly limit nurses’ ability to act autonomously [32-34]. These systemic issues align with broader global challenges, such as resource constraints and a lack of participatory leadership models [32]. Without addressing these barriers—both at the organizational and policy levels—efforts to enhance nurses’ autonomy may remain ineffective. Addressing these challenges requires targeted interventions, including improved managerial training and fostering interprofessional respect within healthcare teams.
Conclusion
The results of our review highlight the importance of fostering a supportive work environment for nurses. By enhancing organizational support and implementing clear policies, healthcare institutions can empower nurses to exercise greater autonomy. This, in turn, is likely to lead to improved job satisfaction, retention rates, and ultimately better patient care outcomes. Nursing leaders and administrators must recognize the role of continuous education and professional development in promoting nurses’ confidence and decision-making abilities.
The strength of this study lies in its comprehensive analysis of various research findings, which provides valuable insights into how these factors interact to shape the autonomy nurses experience in different clinical settings. However, the study also has limitations, such as the possibility of publication bias and the variability of methods in the reviewed studies, which may affect the generalizability of the results. Future research should focus on longitudinal studies to better understand the causal relationships between these factors and professional autonomy and examine innovative strategies to improve nurses’ independence in practice.
Future studies should investigate cultural mediators of autonomy using cross-national comparative designs to address these complexities and understand how different healthcare systems influence nurses’ professional autonomy. Additionally, developing intervention studies is essential to test strategies that balance autonomy with systemic support, such as implementing mentorship programs for junior nurses to foster their confidence and decision-making skills. Furthermore, exploring gender-specific dynamics in nursing autonomy is crucial, as preliminary data suggest that male nurses report higher levels of autonomy in specific contexts. By examining these areas, researchers can provide valuable insights that inform policy and practice to enhance nurses’ professional autonomy across diverse settings.
This review highlights the dual role of autonomy as both an empowerment tool and a potential stressor, contingent on organizational and cultural contexts. By addressing these nuances, healthcare systems can better leverage autonomy to improve nurse retention, patient care quality, and ethical practice.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Atefe Esmailpour Moalem; Data analysis and interpretation: Atefe Esmailpour Moalem and Hedayat Jafari; Drafting of the manuscript: Vida Shafipour; Critical revision of the manuscript for important intellectual content: Leila Shafipour; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate the support of Mazandaran University of Medical Sciences, Sari, Iran, which provided the necessary resources for conducting this comprehensive literature review.
References
- Mackenzie C. Relational autonomy, normative authority and perfectionism. J Soc Philos. 2008; 39(4):512-33. [DOI:10.1111/j.1467-9833.2008.00440.x]
- Varjus SL, Leino-Kilpi H, Suominen T. Professional autonomy of nurses in hospital settings--a review of the literature. Scand J Caring Sci. 2011; 25(1):201-7. [DOI:10.1111/j.1471-6712.2010.00819.x] [PMID]
- Feist GJ. Autonomy and independence. In: Runco MA, editor. Encyclopedia of creativity. San diego: Academic Press; 1999. [Link]
- Baykara ZG, Şahinoğlu S. An evaluation of nurses' professional autonomy in Turkey. Nurs Ethics. 2014; 21(4):447-60.[DOI:10.1177/0969733013505307] [PMID]
- Rouhi-Balasi L, Elahi N, Ebadi A, Jahani S, Hazrati M. Professional autonomy of nurses: A qualitative meta-synthesis study. Iran J Nurs Midwifery Res. 2020; 25(4):273-81. [DOI:10.4103/ijnmr.IJNMR_213_19] [PMID]
- Rafferty AM, Ball J, Aiken LH. Are teamwork and professional autonomy compatible, and do they result in improved hospital care? Qual Health Care. 2001; 10(S 2):ii32-7. [DOI:10.1136/qhc.0100032] [PMID]
- Shorofi SA, Karimzadeh M. [Factors associated with burnout in nursing staff: A review article (Persian)]. Clin Exc. 2015; 3(2):56-70. [Link]
- Shohani M, Zamanzadeh V. Nurses' attitude towards professionalization and factors influencing it. J Caring Sci. 2017; 6(4):345-57. [DOI:10.15171/jcs.2017.033] [PMID]
- Parizad N, Judi A, Alinejad V, Mohammadpour Y. [Professional autonomy and its relationship with organizational commitment among nurses of intensive care units in Urmia teaching hospitals in 2022 (Persian)]. Nurs Midwifery J. 2023; 21(6):454-62. [DOI:10.61186/unmf.21.6.454]
- Papathanassoglou ED, Karanikola MN, Kalafati M, Giannakopoulou M, Lemonidou C, Albarran JW. Professional autonomy, collaboration with physicians, and moral distress among European intensive care nurses. Am J Crit Care. 2012; 21(2):e41-52. [DOI:10.4037/ajcc2012205] [PMID]
- Jafari Z, Esmaeili M, Bahramnejad F, Noie A. [The relationship between professional autonomy and commitment with education level in intensive care nurses: A cross-sectional study (Persian)]. J Crit Care Nurs. 2024; 16(4):34-41. [Link]
- Pursio K, Kankkunen P, Sanner-Stiehr E, Kvist T. Professional autonomy in nursing: An integrative review. J Nurs Manag. 2021; 29(6):1565-77. [DOI:10.1111/jonm.13282] [PMID]
- Balasi LR, Hazrati M, Ashouri A, Ebadi A, Elahi N. The status of professional autonomy and its predictors in clinical nurses in Iran. Nurs Open. 2024; 11(9):e70011. [DOI:10.1002/nop2.70011] [PMID]
- Motamed-Jahromi M, Jalali T, Eshghi F, Zaher H, Dehghani SL. Evaluation of professional autonomy and the association with individual factors among nurses in the Southeast of Iran. J Nurs Midwifery Sci. 2015; 2(4):37-42. [Link]
- Jafari H, Khaghanizade M, Mokhtari Nouri J, Sirati Nir M. [Developmental strategies for nursing ethics education (Persian)]. Med Ethics J. 2017; 10(38):81-90. [Link]
- Abd-Elrhaman ESA, Ghoneimy AGH, Ismael ZI. Creative management and mindfulness among head nurses and its relation to nurses’ work thriving and professional nursing autonomy. J Nurs Sci Benha Univ. 2023; 4(1):730-50. [DOI:10.21608/jnsbu.2023.278959]
- Pursio K, Kankkunen P, Mikkonen S, Kvist T. Organizational characteristics of nursing practice environments related to registered nurses' professional autonomy and job satisfaction in two Finnish Magnet-aspiring hospitals: Structural equation modeling study. BMC Nurs. 2024; 23(1):100.[DOI:10.1186/s12912-024-01772-9] [PMID]
- Roshanzadeh M, Aghaei M, Kashani E, Pasaeimehr Z, Tajabadi A. [Strategies for professional autonomy in nursing (Persian)]. Sci J Nurs Midwifery Paramed Fac. 2018; 4(1):1-5. [Link]
- Hsiu-Ying L. "The effect of evidence-based nursing education on nurses' clinical decision-making. J Nurs Res. 2017; 25(2):123-30.
- Seabrook EM. A search for role clarity: A critical discourse analysis of the RN and RPN entry-to-practice competencies that shape nursing curriculum in Ontario, Canada [PhD dissertation]. Ontario: The University of Western Ontario; 2023. [Link]
- Asgari S, Shafipour V, Taraghi Z, Yazdani-Charati J. Relationship between moral distress and ethical climate with job satisfaction in nurses. Nurs Ethics. 2019; 26(2):346-56. [DOI:10.1177/0969733017712083] [PMID]
- Şahan S, Özdemir C. Determining the relationship between nurses› attitudes to professional autonomy and job satisfaction. Mediterr Nurs Midwifery. 2023; 3(2):90-7. [DOI:10.4274/MNM.2023.22144]
- Taleghani F, Dehbozorgi R, Babashahi M, Monemian S, Masoumi M. Analysis of the concept of nurses' autonomy in intensive care units: A hybrid model. Invest Educ Enferm. 2023; 41(2):e17. [DOI:10.17533/udea.iee.v41n2e17] [PMID]
- Weston MJ. Strategies for enhancing autonomy and control over nursing practice. Online J Issues Nurs. 2010; 15(1). [DOI:10.3912/OJIN.Vol15No01Man02]
- Saad ESS, Elsayed SM. Organizational support as perceived by staff nurses and its relation to their autonomy. Evid Based Nurs Res. 2019; 1(3):171-81. [DOI:10.47104/ebnrojs3.v1i3.81]
- Mrayyan MT, Abu Khait A, Rababa M, Algunmeeyn A, Al-Rawashdeh S, AL-Atiyyat N, et al. Professional Autonomy in nursing: A concept analysis. SAGE Open. 2024; 14(4). [DOI:10.1177/21582440241302129]
- Abdolmaleki M, Lakdizaji S, Ghahramanian A, Allahbakhshian A, Behshid M. Relationship between autonomy and moral distress in emergency nurses. Indian J Med Ethics. 2019; 4(1):20-5. [DOI:10.20529/IJME.2018.076] [PMID]
- Labrague LJ, McEnroe-Petitte DM. "Organizational politics, nurses' stress, burnout levels, turnover intention and job satisfaction." Int NursRev. 2017; 64(1):109-16. [DOI:10.1111/inr.12347]
- .Borhani F, Abbaszadeh A, Nakhaee N, Roshanzadeh M. The relationship between moral distress, professional stress, and intent to stay in the nursing profession. J Med Ethics Hist Med. 2014; 7:3. [PMID]
- Sarkoohijabalbarezi Z, Ghodousi A, Davaridolatabadi E. The relationship between professional autonomy and moral distress among nurses working in children's units and pediatric intensive care wards. Int J Nurs Sci. 2017; 4(2):117-21. [DOI:10.1016/j.ijnss.2017.01.007] [PMID]
- Falatah R, Alfi E. Perceived autonomy and anticipated turnover: The mediation role of burnout among critical care nurses. Healthcare. 2025; 13(6):652. [DOI:10.3390/healthcare13060652]
- Haghiri M, Habibpour V, Moharekpour N, Ghasemi M. [Effect of nurses’ autonomy on the quality of patient care based on Kramer and Schmalenberg’s model (Persian)]. J Arak Uni Med Sci. 2022; 25(2):282-95. [DOI:10.32598/jams.25.2.6852.2]
- Jadidi A, Amini R, Hasanian ZM, Maghsoodi Z, Rzavi MR. [Explaining nursing profession policy challenges; a qualitative study (Persian)]. Nurs Dev Health J. 2021; 12(1):1-11. [Link]
- Yadegary MA, Aghajanloo A, Negarandeh R. [Challenges of professional self-regulation in Iranian nursing (Persian)]. J Hayat. 2017; 23(1):1-6. [Link]
- Noh S, Kang Y. The relationships among communication competence, professional autonomy and clinical reasoning competence in oncology nurses. Nurs Open. 2024; 11(8):e70003. [PMID]
- Zaki SS, M Eldeep N, El Hanafy E. Relationship between Health Care Organizational Culture and Professional Nurses' Autonomy. Alexandria Sci Nurs J. 2023; 25(2):1-12. [DOI: 10.21608/asalexu.2023.318208]
- Rouhi Balasi L, Shafaati Shamami H, Alizadeh A, Pasandidehfar S, Makhsoos M, Gholami A. Professional nursing autonomy and safe nursing care in newly graduated nurses working in emergency departments. J Guilan Univ Med Sci. 2024; 33(1):32-41. [DOI:10.32598/JGUMS.33.1.541.1]
- Kurt D, Gurdogan EP. Professional autonomy and patient advocacy in nurses. Collegian. 2023; 30(2):327-34. [DOI:10.1016/j.colegn.2022.09.015]
- Mohamed MH, El-Demerdash SM, Hasanin AG. Nurse/Physician collaboration and its relation to professional nursing autonomy as perceived by nurses. J Nurs Sci Benha Univ. 2021; 2(1):201-13. [Link]
- Mert Ş, Türkmen E. The relationship between work-related variables, job satisfaction, and perceived professional autonomy of radiation oncology nurses in Turkey. J Psychiatr Nurs. 2020; 11(4). [Link]
- Mousavi SR, Amini K, Ramezani-Badr F, Roohani M. Correlation of happiness and professional autonomy in Iranian nurses. J Res Nurs. 2019; 24(8):622-32. [DOI:10.1177/1744987119877421]
- Mousavizadeh SN, Mohtashami J. Correlation between professional autonomy and evidence-based practice in nurses. Med Sci Educ. 2018; 22(94):514-7. [Link]
- Yeganeh MR, Pouralizadeh M, Ghanbari A. The relationship between professional autonomy and moral distress in ICU nurses of Guilan University of Medical Sciences in 2017. Nurs Pract Today. 2019; 6(3):133-41. [Link]
Type of Study: review |
Subject:
Psychiatric Nursing
Received: 2024/01/3 | Accepted: 2024/03/1 | Published: 2024/04/1
Received: 2024/01/3 | Accepted: 2024/03/1 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |