Sun, Feb 1, 2026
[Archive]
Volume 2, Issue 2 (Winter 2024)
CPR 2024, 2(2): 103-112 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Norouzinia R, Aghabarary M, Rosenstein A H, Rahmatpour P. Disruptive Behaviors of Iranian Physicians and Nurses in the Emergency Departments and Its Consequences. CPR 2024; 2 (2) :103-112
URL: http://cpr.mazums.ac.ir/article-1-95-en.html
URL: http://cpr.mazums.ac.ir/article-1-95-en.html
Health Sciences Research Unit: Nursing (UICISA: E), Nursing School of Coimbra (ESEnfC), Coimbra, Portugal.
Full-Text [PDF 733 kb]
(400 Downloads)
| Abstract (HTML) (1205 Views)
Full-Text: (470 Views)
Introduction
In the healthcare literature, the concept of disruptive behavior (DB) has become a prevalent topic for discussion, exerting a high influence on the healthcare delivery, nursing care, and patient safety [1, 2]. The DB is defined as any inappropriate behavior, verbal or physical, that causes negative impact on the quality of nursing care. It’s often known as “indirect hostility” or “unprofessional behavior” [3]. Examples of DB include verbal, physical, and emotional abuse, intimidation, harassment, and workplace incivility [4]. The intensity of DB can vary, including lower level (such as incivility) moderate level (such as psychological aggression), and severe level (physical abuse) [3, 5]. The DBs have adverse consequences for healthcare centers, their personnel, and the patients under care. When behaviors such as incivility, bullying, and violence are seen in healthcare settings, they have a profound impact on the work environment, organizational ethical climate, job satisfaction and staff retention [6, 7]. The DBs disrupt morale and teamwork, leading to a breakdown in trust and mutual respect between healthcare professionals and their patients [3, 8]. Moreover, they can lead to medical errors, neglect of essential nursing care, occurrences of “never events”, reduced patient satisfaction, and compromised patient safety [9, 10, 11].
Recent studies underscore the impact of DB on nurses’ work environments. Nurses perceive these behaviors as substantial barriers to their motivation and job satisfaction. Over 60% of nurses have chosen to leave their jobs due to direct violence inflicted upon them by fellow nurses [5]. The DB serves as a wellspring of interpersonal stress and conflict, particularly for nurses, leading to tension, absenteeism and failure [12], which can have detrimental repercussions on patient outcomes [5]. This cascade effect results in diminished morale, decreased job satisfaction, heightened workloads and an increased risk to patient safety [5, 13]. The occurrence of DB is influenced by several individual and organizational factors, including cultural influences, personality traits, social status, organizational policies, ethical considerations and personal conflicts [4, 12]. Healthcare professionals often face a gamut of negative emotions, such as anxiety, anger, hopelessness, shame, frustration and depression, all of which can significantly disrupt their clinical decision-making, thought processes, and overall performance [14]. A qualitative study conducted in Iran identified inappropriate organizational mindset, ineffectual management, complex work conditions in the nursing profession, inadequate standards of education and training for nurses, and personal contributions as key factors contributing to the occurrence of DB [15].
In the high-stress environment such as the emergency departments, where patients are particularly vulnerable to medical errors, disruptions in workplace communication can lead to communication breakdowns during the examination and treatment of patients, inadvertently affecting treatment outcomes [5, 16]. Studies conducted in Iran have indicated a high prevalence of DB, posing a substantial threat to the provision of healthcare services, nursing care, and treatment [17, 18]. Maddineshat et al. in a study in Iran, in 2016, reported that 81% of physicians and 52% of nurses in the emergency departments exhibiting DBs [18].
Given the importance of the DB concept, its prevalence, and the substantial risks it poses to patient health and safety, and considering that it has not been measured in hospitals of Alborz Province in Iran, this study aimed to determine the prevalence and consequences of DBs among physicians and nurses of the emergency departments in hospitals of Alborz Province.
Materials and Methods
Study design and participants
The cross-sectional study was conducted in the emergency departments of two teaching hospitals affiliated to Alborz University of Medical Sciences during May-June 2020. Participants were 149 physicians and nurses working in the emergency departments of two teaching hospitals. Inclusion criteria were at least one year of experience in emergency departments and willingness to participate in the study. Those who declined to continue participation or failed to complete the questionnaires were excluded from the study. Sample selection was done using a convenience sampling method.
Measures
In this study, a two-part questionnaire was used; the first part surveyed demographic information (age, gender, marital status, job, and work experience) and the second part was the DBs scale developed by Rosenstein and O’Daniel [19]. We translated the questionnaire into Persian and then assessed its face and content validity. For face validity assessment, the opinions of five nurses and physicians were used. For determining content validity, the opinions of a panel of experts consisting of 10 faculty members from Alborz University of Medical Sciences in nursing, medical emergency, and emergency were used. Maddineshat et al. also used this questionnaire on the Iranian population and assessed its reliability [18]. The DBs scale consists of 23 multiple choice and open-ended questions, measuring the frequency of DBs (9 items), the consequences of DBs (6 items), the rules for dealing with DBs (5 items), and the reporting of DBs (3 items). The answers to the questions included yes/no, or the Likert scale. After explaining the study objectives to the participants and obtaining their written informed consent, the questionnaires distributed among them in the emergency department of the hospitals. Questionnaires were completed anonymously and participants’ information was kept confidential.
Data analysis
The collected data were analyzed in SPSS software version 20 using descriptive statistics (frequency, percentage, Mean±SD) and t-test to compare the scores.
Results
In the present study, 105 out of 149 eligible individuals participated (response rate: 67%), including 32 physicians and 73 emergency nurses. Most of them were female (n=80, 76.2%) and married (n=86, 81.9%). Their mean age was 32.54±6.77 years (ranged 24-50) and their mean work experience was 6.51±5.62 years.
According to physicians and nurses, the general atmosphere of nurse/physician relationships in the hospitals was mostly positive (7.72±1.50 and 7.69±2.34, respectively, out of 10). All respondents (100%) in both groups witnessed DBs in their hospitals. The specific ward where DBs were most prevalent, according to physicians and nurses, was the resuscitation & triage rooms (45.5%). Both physicians and nurses observed that DBs occur most often among emergency specialists (42.4% and 38.9%, respectively). More than 20% of physicians and less than 5% of nurses had DBs in their hospital. In response to how often DBs occur in the hospital, 45.7% reported that physician DB occurred weekly and 42.9% reported that nurse DB occurred 1-5 items a year (Table 1).
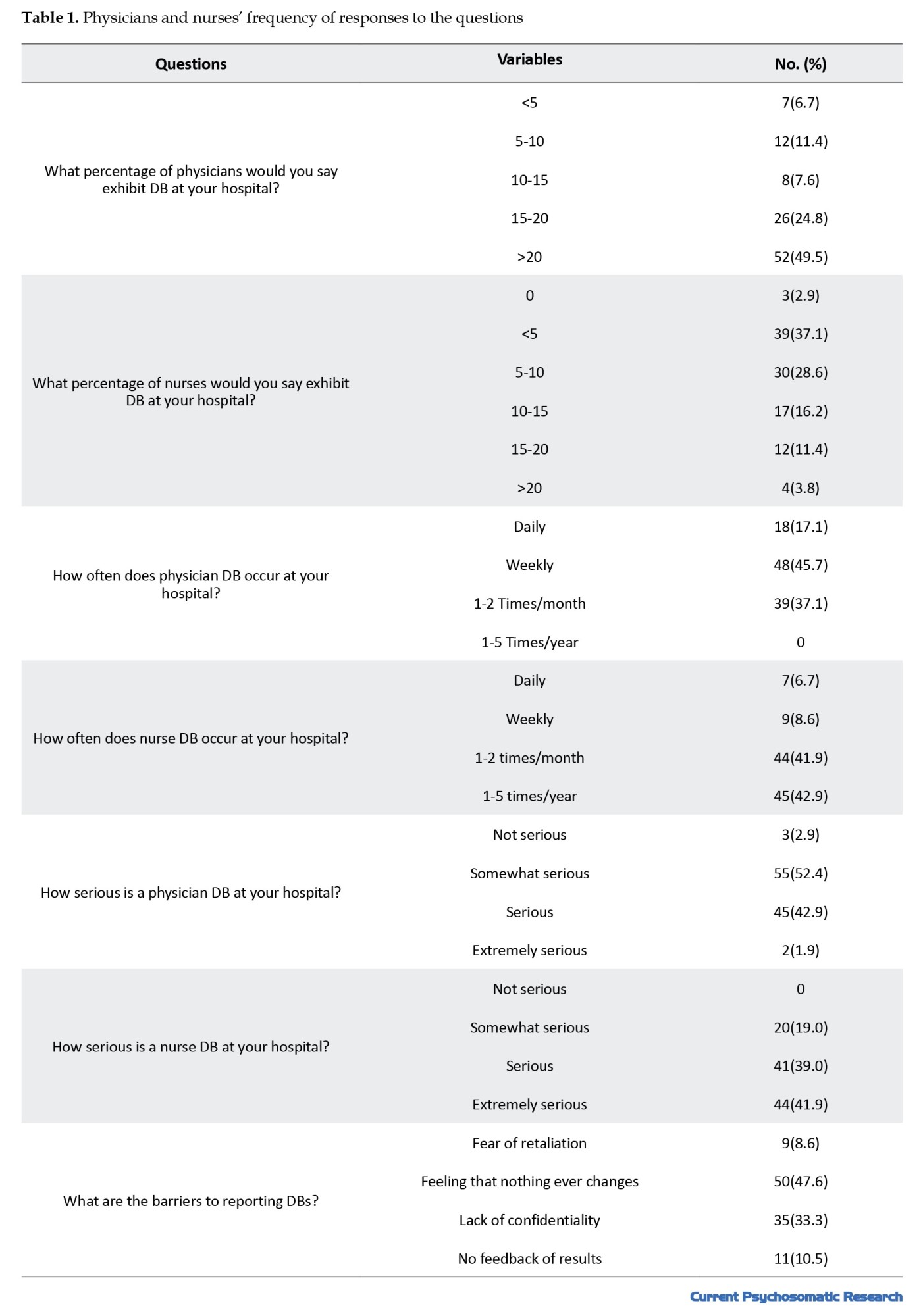
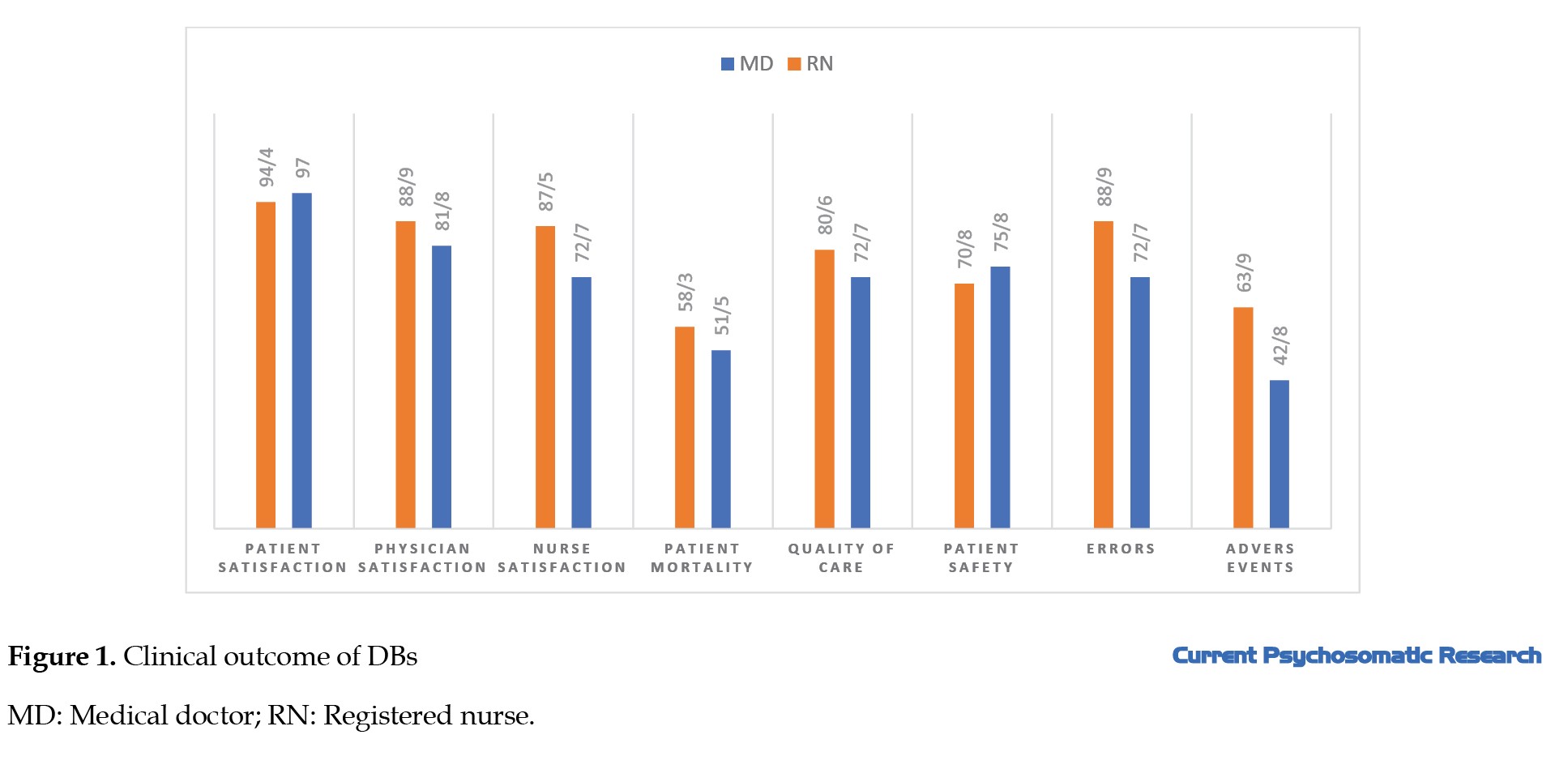
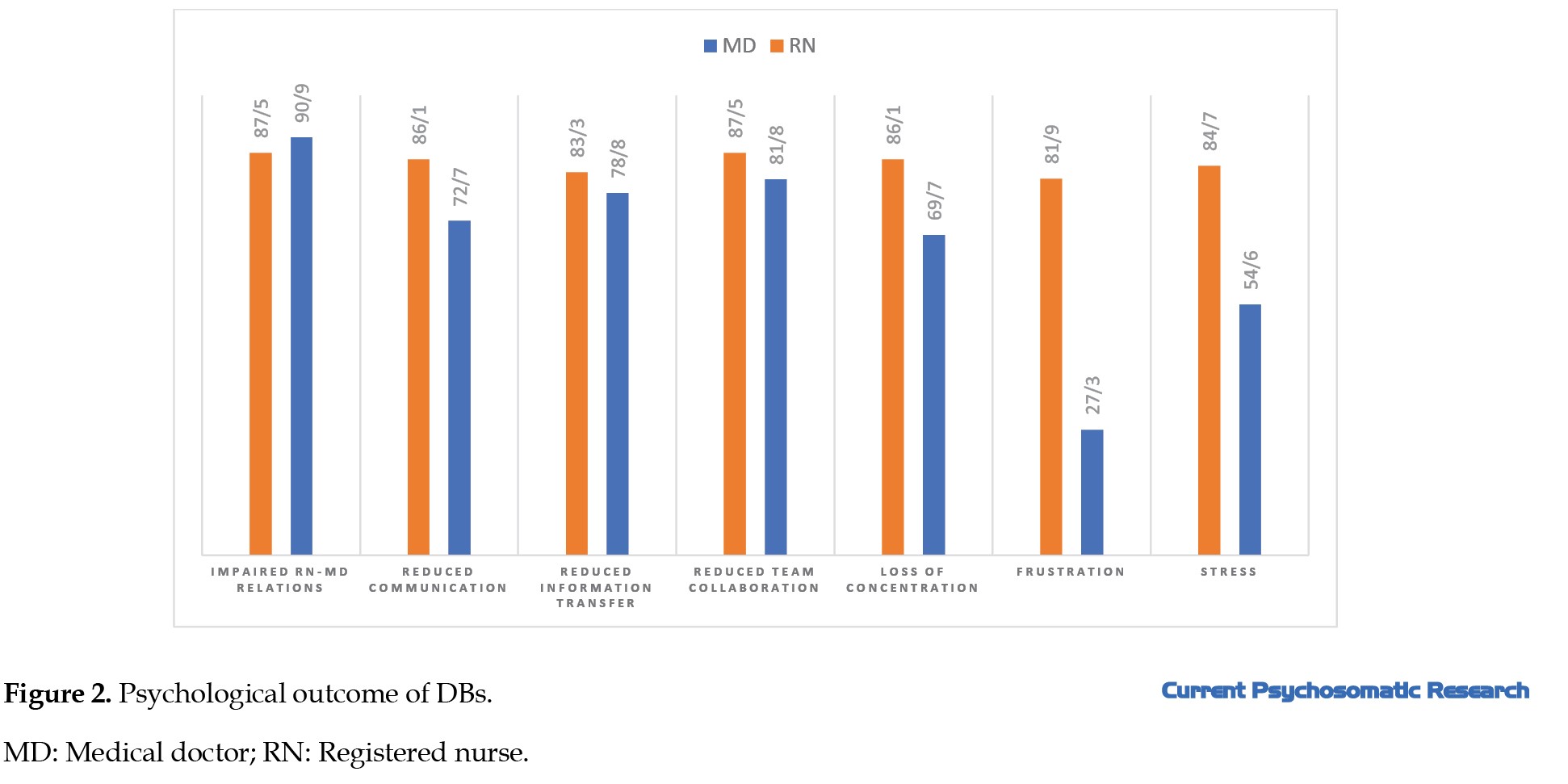
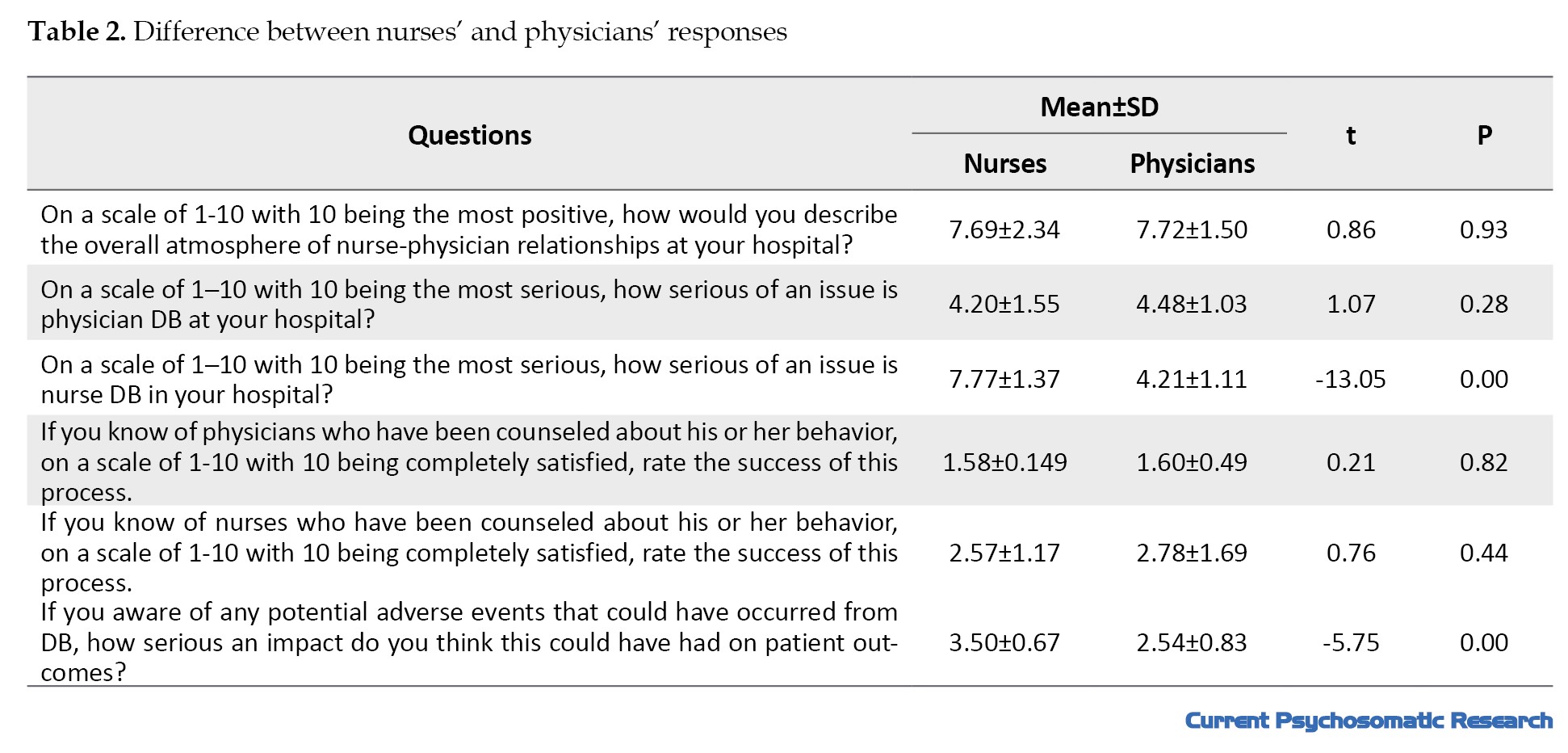
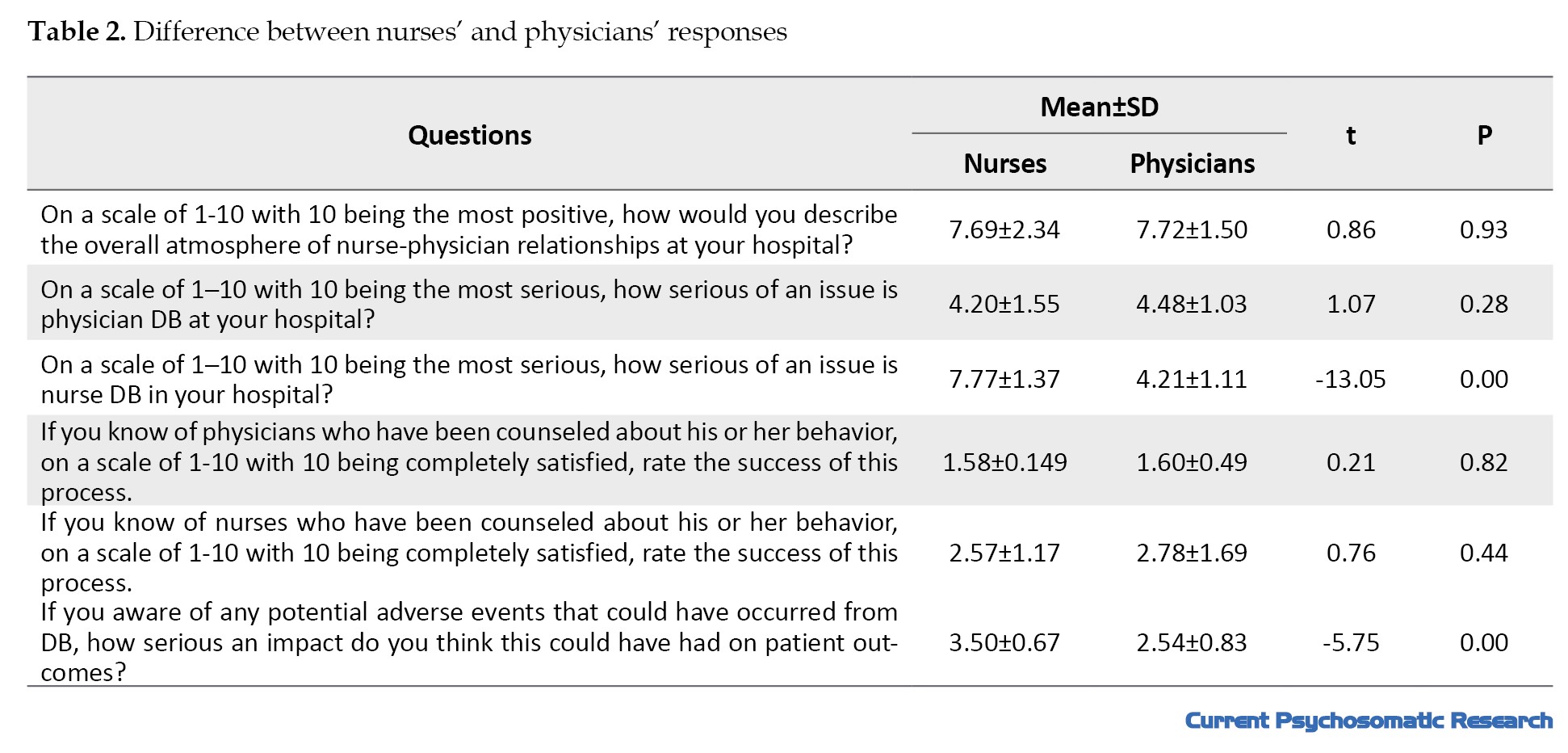
All physician and nurses had awareness of the potential adverse events that could result from DBs, with 55.2% believing that such events could be prevented. The majority of physicians and nurses (81%) indicated that the effect of DBs on patient outcomes ranged from serious to very serious. In addition, 42.4% of physicians and 61.1% of nurses reported that adverse events could be prevented. Both groups believed that clinical outcomes of DBs affect patient satisfaction (Figure 1). The most prevalent psychological outcomes of DBs from the viewpoint of physicians and nurses were impaired nurse-physician relations and reduced nurse-physician collaboration (Figure 2). All respondents perceived that there was no code of conduct or policy to control these behaviors in emergency departments. Also, they stated that there was no non-punitive environment for those who witness/experience DBs in their hospitals. The most common barrier that participants mentioned about the reporting process was the feeling that nothing ever changes (47.6%) (Table 1). The results of independent t-test to compare the responses of nurses and physicians (Table 2) showed a significant difference between their responses to the seriousness of nurse DBs (t=-13.05, P<0.001) and the seriousness of the impact of DBs on patient outcomes (t=-5.75, P<0.001).
Discussion
The aim of this study was to investigate the frequency and consequences of DBs from physicians and nurses in emergency departments. All participants reported the witnessing or experiencing of DBs. Physicians were observed to had such behaviors on a weekly basis, while nurses their occurrence on a yearly basis. These findings are consistent with a previous study, which demonstrated a high prevalence of DBs among nurses and physicians on a weekly basis [20]. In another study, physicians were found to show significantly higher levels of DBs than nurses, with monthly occurrence being more common [12]. Notably, Rosenstein in 2008 noted that 74% of participants had borne witness to physician DBs, while 56% of physicians observed similar behavior in their colleagues. Additionally, 64% of participants observed nurse DBs, with over 70% reporting such behaviors in their colleagues, 1-2 times per month or 5-6 times per year [19]. Rosenstein and Naylor in a study in 2012 revealed that the incidence of DB was higher among physicians than nurses, although the difference was not statistically significant [16]. Conversely, Rosenstein and O’Daniel found that a high number of respondents reported witnessing DBs more frequently among nurses [19]. These findings collectively attest to the pervasive nature of DBs among medical staff.
The present study showed that the most of DBs occurred in the resuscitation & triage rooms, consistent with the results of Antoniadis et al. [21]. Norouzinia et al. in qualitative study in 2020 suggested that emergency department nurses have elevated levels of pressure and stress. This is highly attributed to the shortage of professional nursing staff as well as heavy workload and irregular work shifts [22]. Given the heightened tension and workplace stress endemic to the resuscitation & triage rooms, it becomes imperative for hospital managers to prioritize employee selection, hold continuous training courses on communication skills and anger management, provide outlets for debriefing emotions and feelings in a secure environment with the presence of a counselor and more amenities suitable for the emergency environment.
The results of this study indicated that emergency medicine specialists and general surgeons had the highest percentage of DBs in the emergency department. This finding is in line with the results of a previous studies that demonstrated a higher prevalence of DBs among general surgeons, cardiovascular surgeons, neurosurgeons, orthopedic specialists, and gynecologists. Maddineshat et al. also reported that pediatricians, general surgeons, and obstetricians showed DBs more frequently [18]. The emergency medicine specialists, due to working in stressful environments, such as emergency departments, are potentially more susceptible to exhibiting DBs. On the other hand, this study was coincided with the COVID-19 pandemic, which created more stressors for these professionals.
A majority of participants in our study perceived that more than 20% of physicians exhibit DBs, whereas the corresponding percentage for nurses was less than 5%. Saghaei et al.’s study in 2020 reported a similar results, with the majority reporting that more than 20% of both physicians and nurses exhibit DBs [20]. These findings highlight a disconcerting prevalence of DBs, necessitating a robust response.
All participants in the present study were aware of the potential adverse events as a result of DBs. In contrast, Saghaei et al. found that about half of the respondents were aware of these consequences [20]. This discrepancy may be related to difference in the study population. The current study sampled physicians and nurses, while Saghaei et al.’s study also used non-clinical staff. The participants in our study reported that DBs had significant psychological and clinical outcomes. Maddineshat et al. also suggested that DBs cause a more pronounced negative effect on the psychological well-being of physicians and nurses in comparison to clinical outcomes [12]. Although differences exist in the perspectives of physicians and nurses concerning the consequences of DB, both groups perceived that these behaviors disrupt physician-nurse relations, information transfer, communication quality, and effective teamwork. Notably, nurses reported higher stress and frustration compared to physicians. The most common clinical outcome of DBs was related to dissatisfaction. Furthermore, according to both physician and nurse groups, DBs reduce the quality of nursing care, pose a risk to patient safety, and increase the likelihood of medical errors. Given the high responsibility of healthcare providers to save the lives of individuals, effective management and control of DBs can have a positive impact on the satisfaction of patients and other healthcare providers. Rosenstein and Daniel highlighted that stress, frustration, and impaired communication were the most frequently reported consequences of DBs, while staff dissatisfaction, poor quality of nursing care, and adverse events were the most prevalent clinical outcomes [19]. Another study reported a significant correlation between DBs and medical errors, reduced patient safety, poor care quality and increased patient mortality [16]. Further studies have also indicated the negative impact of DBs on staff well-being, nursing care quality, and efficient resource management [5, 20, 23-25]. Dang et al. suggested the importance of the impact of DBs on patient safety and argued that psychological aggression caused by DBs increases the risk of medical errors [3].
In current study, more than half of the study participants did not report DBs. This is against the findings of previous studies that indicated a greater tendency among staff in some healthcare settings to report such behaviors [12, 18, 26-30]. This discrepancy can be attributed to the negative experiences that the participants in our study of reporting DBs. Furthermore, the participants in our study perceived that hospital managers did not place a strong emphasis on addressing DBs. This finding is consistent with a previous study which demonstrated that hospital managers had more tendency to take nurses’ DBs more seriously than those of physicians, with a significant difference between the two groups. This difference can be related to higher position and social status of physicians compared to nurses in Iran and considering the fact that most authorities and managers in the ministry of health also physicians. As a result, managers may exhibit lower tendency to address physicians’ DBs [12]. In a survey conducted by Fast et al. in 2020, a minority of participants reported DBs, with over 30% admitting that they had never reported such behaviors. Furthermore, only 21% reported satisfaction with managers’ responses to reported cases of DBs. Only one in five participants were satisfied with how managers addressed such reports [31].
The participants uniformly perceived that there were no effective rules to address DBs. This is consistent with a previous research, in which more than half of the participants reported a lack of policies or strategies to manage such behaviors [12]. Saghaei et al. found that the majority of respondents in their study believed that there were no established behavioral guidelines to prevent DBs. Even though such rules existed, there would be insufficient executive support for their implementation [20]. Hospitals require well-defined policies and standards to mitigate the incidence of DBs and hospital managers should encourage the personnel to report DBs and inform them about the adverse consequences of DBs and the benefits of timely reporting for effective management and prevention. On the other hand, appropriate feedback from officials to reported cases can enhance the satisfaction of personnel with managerial performance in addressing DBs. These strategies have the potential to improve job satisfaction, productivity and employee commitment in the healthcare settings [31, 32].
Both physicians and nurses perceived that the attitudes of officials towards DBs can significantly influence the efforts made to control and reduce such behaviors. In Maddineshat et al.’s study, the majority of participants believed that healthcare organizations can implement policies to effectively address these behaviors [12]. Fast et al. also suggested that clear policies and programs are essential to address DBs and enhance employee satisfaction in the healthcare centers. To comprehensively address DBs, healthcare centers should establish a reporting system for physicians, while officials respond appropriately to the reports. This approach is pivotal in building trust and ensuring the implementation of necessary changes [31]. Failure to report DBs can normalize the behaviors over time. Hospital managers should delve into the factors contributing to staff reluctance to report DBs within the system. Younger staff, those without management responsibilities, anesthesiologists, and surgeons refuse to report DBs more than nurses [31].
The participants in our study indicated that the primary barriers to reporting DBs were the feeling that nothing ever changes and lack of confidentiality. This finding is consistent with other studies that identified system inefficiency and frustration with the lack of change as the main reasons for not reporting DBs [12, 18]. However, in one study, fear of retaliation was found to be the most important barrier, although concerns about the lack of change and confidentiality also were reported [20]. Educational interventions and an appropriate reporting system can improve the reporting of DBs [33].
This study observed a significant difference in taking nurse DBs seriously, consistent with Maddineshat et al.’s study [18]. According to the nurses in this study, the hospital authorities consider the nurse DBs more serious than the physician DBs. Furthermore, a significant difference was detected between the nurses’ and physicians’ responses to the seriousness of the impact of DBs on patient outcomes. According to nurses, the impact of DBs on patient outcomes are more serious.
There were a number of limitations to our study. The study was limited to the emergency departments of selected teaching hospitals, and the results cannot be generalized to other departments or hospitals. Also, we used self-reported data, which may be subject to response bias. There was also a small sample size due to difficulty in recutting more samples. Finally, there was a lack of study on the long-term effects of DBs on patient safety, quality of care, patient mortality, nurse satisfaction, physician satisfaction, and patient satisfaction. Based on the findings of study, it is crucial to ensure that medical students, medical staff, hospital managers, and policymakers, understand and recognize the DBs, for addressing the issue effectively. Hospital managers should be informed about the prevalence and impact of DBs. They should take steps to develop clear policies and guidelines to identify, prevent, or manage the occurrence of DBs among medical staff. Moreover, regular monitoring and assessment of these policies is essential to ensure they are implemented effectively. Practical workshops on communication skills should be held to improve the communication and collaboration between physicians and nurses. Given the significant adverse effects of DBs, interventions should be designed and conducted to reduce their incidence and consequences. These interventions can involve educational interventions, support interventions, and strategies to create a culture of respect and collaboration within healthcare settings.
Conclusion
The DBs are prevalent in the emergency departments of selected hospitals in Iran, according to nurses and physicians. Since DBs can negatively affect the well-being of medical staff, patient safety, and quality of nursing care, effective interventions, including policy development, communication skills training, and educational intervention, are needed to improve nurse/physician relationships and reduce DBs in the emergency departments.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Alborz University of Medical Sciences (Code: IR.ABZUMS.REC.1398.144). All methods were carried out in accordance with relevant guidelines and regulation. Informed consent was obtained from all participants.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization and study design: Maryam Aghabarary, Roohangiz Norouzinia and Alan H Rosenstein; Data collection: Roohangiz Norouzinia; Data analysis: Pardis Rahmatpour; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Alborz University of Medical Sciences and all participants for their cooperation.
References
In the healthcare literature, the concept of disruptive behavior (DB) has become a prevalent topic for discussion, exerting a high influence on the healthcare delivery, nursing care, and patient safety [1, 2]. The DB is defined as any inappropriate behavior, verbal or physical, that causes negative impact on the quality of nursing care. It’s often known as “indirect hostility” or “unprofessional behavior” [3]. Examples of DB include verbal, physical, and emotional abuse, intimidation, harassment, and workplace incivility [4]. The intensity of DB can vary, including lower level (such as incivility) moderate level (such as psychological aggression), and severe level (physical abuse) [3, 5]. The DBs have adverse consequences for healthcare centers, their personnel, and the patients under care. When behaviors such as incivility, bullying, and violence are seen in healthcare settings, they have a profound impact on the work environment, organizational ethical climate, job satisfaction and staff retention [6, 7]. The DBs disrupt morale and teamwork, leading to a breakdown in trust and mutual respect between healthcare professionals and their patients [3, 8]. Moreover, they can lead to medical errors, neglect of essential nursing care, occurrences of “never events”, reduced patient satisfaction, and compromised patient safety [9, 10, 11].
Recent studies underscore the impact of DB on nurses’ work environments. Nurses perceive these behaviors as substantial barriers to their motivation and job satisfaction. Over 60% of nurses have chosen to leave their jobs due to direct violence inflicted upon them by fellow nurses [5]. The DB serves as a wellspring of interpersonal stress and conflict, particularly for nurses, leading to tension, absenteeism and failure [12], which can have detrimental repercussions on patient outcomes [5]. This cascade effect results in diminished morale, decreased job satisfaction, heightened workloads and an increased risk to patient safety [5, 13]. The occurrence of DB is influenced by several individual and organizational factors, including cultural influences, personality traits, social status, organizational policies, ethical considerations and personal conflicts [4, 12]. Healthcare professionals often face a gamut of negative emotions, such as anxiety, anger, hopelessness, shame, frustration and depression, all of which can significantly disrupt their clinical decision-making, thought processes, and overall performance [14]. A qualitative study conducted in Iran identified inappropriate organizational mindset, ineffectual management, complex work conditions in the nursing profession, inadequate standards of education and training for nurses, and personal contributions as key factors contributing to the occurrence of DB [15].
In the high-stress environment such as the emergency departments, where patients are particularly vulnerable to medical errors, disruptions in workplace communication can lead to communication breakdowns during the examination and treatment of patients, inadvertently affecting treatment outcomes [5, 16]. Studies conducted in Iran have indicated a high prevalence of DB, posing a substantial threat to the provision of healthcare services, nursing care, and treatment [17, 18]. Maddineshat et al. in a study in Iran, in 2016, reported that 81% of physicians and 52% of nurses in the emergency departments exhibiting DBs [18].
Given the importance of the DB concept, its prevalence, and the substantial risks it poses to patient health and safety, and considering that it has not been measured in hospitals of Alborz Province in Iran, this study aimed to determine the prevalence and consequences of DBs among physicians and nurses of the emergency departments in hospitals of Alborz Province.
Materials and Methods
Study design and participants
The cross-sectional study was conducted in the emergency departments of two teaching hospitals affiliated to Alborz University of Medical Sciences during May-June 2020. Participants were 149 physicians and nurses working in the emergency departments of two teaching hospitals. Inclusion criteria were at least one year of experience in emergency departments and willingness to participate in the study. Those who declined to continue participation or failed to complete the questionnaires were excluded from the study. Sample selection was done using a convenience sampling method.
Measures
In this study, a two-part questionnaire was used; the first part surveyed demographic information (age, gender, marital status, job, and work experience) and the second part was the DBs scale developed by Rosenstein and O’Daniel [19]. We translated the questionnaire into Persian and then assessed its face and content validity. For face validity assessment, the opinions of five nurses and physicians were used. For determining content validity, the opinions of a panel of experts consisting of 10 faculty members from Alborz University of Medical Sciences in nursing, medical emergency, and emergency were used. Maddineshat et al. also used this questionnaire on the Iranian population and assessed its reliability [18]. The DBs scale consists of 23 multiple choice and open-ended questions, measuring the frequency of DBs (9 items), the consequences of DBs (6 items), the rules for dealing with DBs (5 items), and the reporting of DBs (3 items). The answers to the questions included yes/no, or the Likert scale. After explaining the study objectives to the participants and obtaining their written informed consent, the questionnaires distributed among them in the emergency department of the hospitals. Questionnaires were completed anonymously and participants’ information was kept confidential.
Data analysis
The collected data were analyzed in SPSS software version 20 using descriptive statistics (frequency, percentage, Mean±SD) and t-test to compare the scores.
Results
In the present study, 105 out of 149 eligible individuals participated (response rate: 67%), including 32 physicians and 73 emergency nurses. Most of them were female (n=80, 76.2%) and married (n=86, 81.9%). Their mean age was 32.54±6.77 years (ranged 24-50) and their mean work experience was 6.51±5.62 years.
According to physicians and nurses, the general atmosphere of nurse/physician relationships in the hospitals was mostly positive (7.72±1.50 and 7.69±2.34, respectively, out of 10). All respondents (100%) in both groups witnessed DBs in their hospitals. The specific ward where DBs were most prevalent, according to physicians and nurses, was the resuscitation & triage rooms (45.5%). Both physicians and nurses observed that DBs occur most often among emergency specialists (42.4% and 38.9%, respectively). More than 20% of physicians and less than 5% of nurses had DBs in their hospital. In response to how often DBs occur in the hospital, 45.7% reported that physician DB occurred weekly and 42.9% reported that nurse DB occurred 1-5 items a year (Table 1).
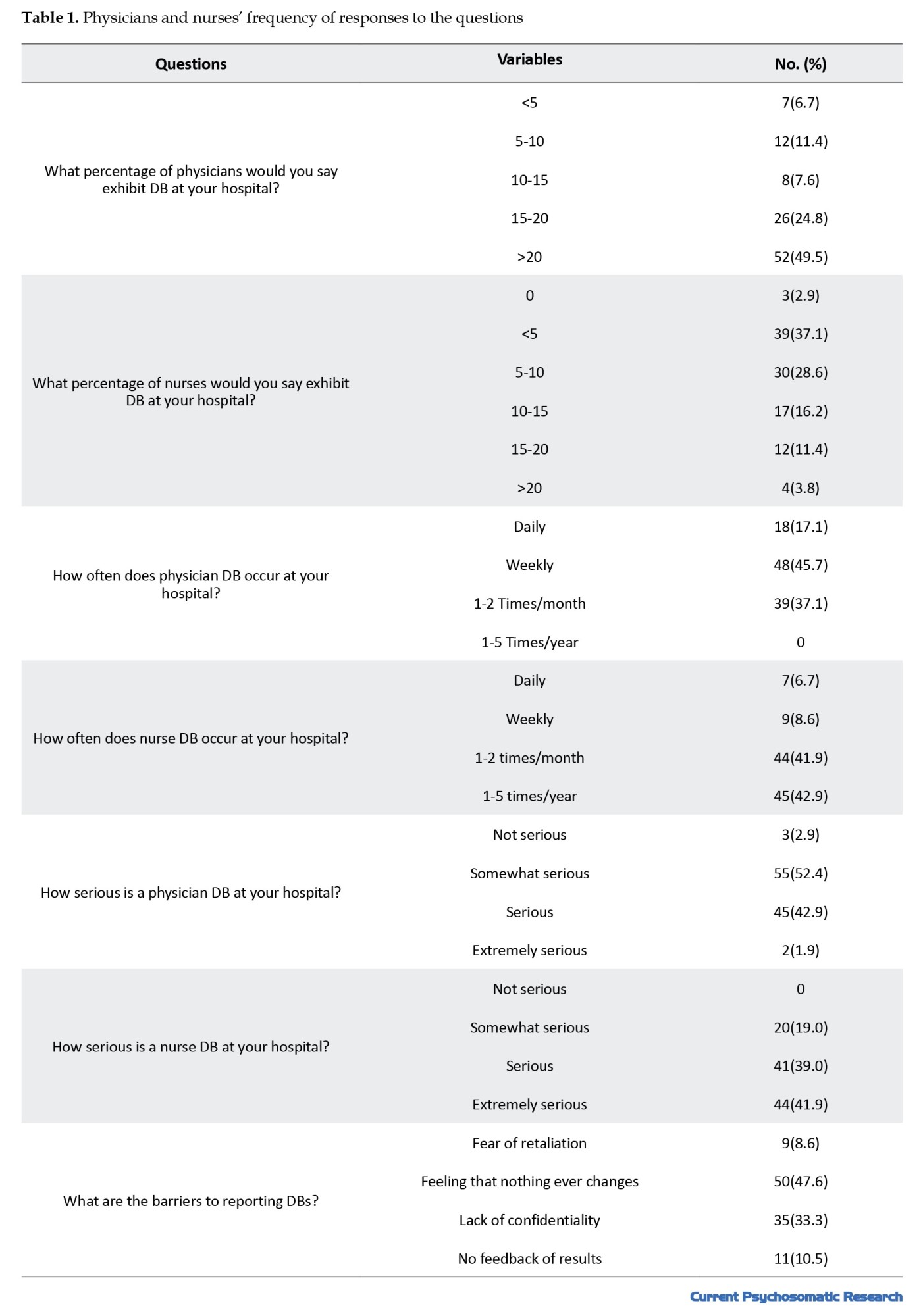
All physician and nurses had awareness of the potential adverse events that could result from DBs, with 55.2% believing that such events could be prevented. The majority of physicians and nurses (81%) indicated that the effect of DBs on patient outcomes ranged from serious to very serious. In addition, 42.4% of physicians and 61.1% of nurses reported that adverse events could be prevented. Both groups believed that clinical outcomes of DBs affect patient satisfaction (Figure 1). The most prevalent psychological outcomes of DBs from the viewpoint of physicians and nurses were impaired nurse-physician relations and reduced nurse-physician collaboration (Figure 2). All respondents perceived that there was no code of conduct or policy to control these behaviors in emergency departments. Also, they stated that there was no non-punitive environment for those who witness/experience DBs in their hospitals. The most common barrier that participants mentioned about the reporting process was the feeling that nothing ever changes (47.6%) (Table 1). The results of independent t-test to compare the responses of nurses and physicians (Table 2) showed a significant difference between their responses to the seriousness of nurse DBs (t=-13.05, P<0.001) and the seriousness of the impact of DBs on patient outcomes (t=-5.75, P<0.001).
Discussion
The aim of this study was to investigate the frequency and consequences of DBs from physicians and nurses in emergency departments. All participants reported the witnessing or experiencing of DBs. Physicians were observed to had such behaviors on a weekly basis, while nurses their occurrence on a yearly basis. These findings are consistent with a previous study, which demonstrated a high prevalence of DBs among nurses and physicians on a weekly basis [20]. In another study, physicians were found to show significantly higher levels of DBs than nurses, with monthly occurrence being more common [12]. Notably, Rosenstein in 2008 noted that 74% of participants had borne witness to physician DBs, while 56% of physicians observed similar behavior in their colleagues. Additionally, 64% of participants observed nurse DBs, with over 70% reporting such behaviors in their colleagues, 1-2 times per month or 5-6 times per year [19]. Rosenstein and Naylor in a study in 2012 revealed that the incidence of DB was higher among physicians than nurses, although the difference was not statistically significant [16]. Conversely, Rosenstein and O’Daniel found that a high number of respondents reported witnessing DBs more frequently among nurses [19]. These findings collectively attest to the pervasive nature of DBs among medical staff.
The present study showed that the most of DBs occurred in the resuscitation & triage rooms, consistent with the results of Antoniadis et al. [21]. Norouzinia et al. in qualitative study in 2020 suggested that emergency department nurses have elevated levels of pressure and stress. This is highly attributed to the shortage of professional nursing staff as well as heavy workload and irregular work shifts [22]. Given the heightened tension and workplace stress endemic to the resuscitation & triage rooms, it becomes imperative for hospital managers to prioritize employee selection, hold continuous training courses on communication skills and anger management, provide outlets for debriefing emotions and feelings in a secure environment with the presence of a counselor and more amenities suitable for the emergency environment.
The results of this study indicated that emergency medicine specialists and general surgeons had the highest percentage of DBs in the emergency department. This finding is in line with the results of a previous studies that demonstrated a higher prevalence of DBs among general surgeons, cardiovascular surgeons, neurosurgeons, orthopedic specialists, and gynecologists. Maddineshat et al. also reported that pediatricians, general surgeons, and obstetricians showed DBs more frequently [18]. The emergency medicine specialists, due to working in stressful environments, such as emergency departments, are potentially more susceptible to exhibiting DBs. On the other hand, this study was coincided with the COVID-19 pandemic, which created more stressors for these professionals.
A majority of participants in our study perceived that more than 20% of physicians exhibit DBs, whereas the corresponding percentage for nurses was less than 5%. Saghaei et al.’s study in 2020 reported a similar results, with the majority reporting that more than 20% of both physicians and nurses exhibit DBs [20]. These findings highlight a disconcerting prevalence of DBs, necessitating a robust response.
All participants in the present study were aware of the potential adverse events as a result of DBs. In contrast, Saghaei et al. found that about half of the respondents were aware of these consequences [20]. This discrepancy may be related to difference in the study population. The current study sampled physicians and nurses, while Saghaei et al.’s study also used non-clinical staff. The participants in our study reported that DBs had significant psychological and clinical outcomes. Maddineshat et al. also suggested that DBs cause a more pronounced negative effect on the psychological well-being of physicians and nurses in comparison to clinical outcomes [12]. Although differences exist in the perspectives of physicians and nurses concerning the consequences of DB, both groups perceived that these behaviors disrupt physician-nurse relations, information transfer, communication quality, and effective teamwork. Notably, nurses reported higher stress and frustration compared to physicians. The most common clinical outcome of DBs was related to dissatisfaction. Furthermore, according to both physician and nurse groups, DBs reduce the quality of nursing care, pose a risk to patient safety, and increase the likelihood of medical errors. Given the high responsibility of healthcare providers to save the lives of individuals, effective management and control of DBs can have a positive impact on the satisfaction of patients and other healthcare providers. Rosenstein and Daniel highlighted that stress, frustration, and impaired communication were the most frequently reported consequences of DBs, while staff dissatisfaction, poor quality of nursing care, and adverse events were the most prevalent clinical outcomes [19]. Another study reported a significant correlation between DBs and medical errors, reduced patient safety, poor care quality and increased patient mortality [16]. Further studies have also indicated the negative impact of DBs on staff well-being, nursing care quality, and efficient resource management [5, 20, 23-25]. Dang et al. suggested the importance of the impact of DBs on patient safety and argued that psychological aggression caused by DBs increases the risk of medical errors [3].
In current study, more than half of the study participants did not report DBs. This is against the findings of previous studies that indicated a greater tendency among staff in some healthcare settings to report such behaviors [12, 18, 26-30]. This discrepancy can be attributed to the negative experiences that the participants in our study of reporting DBs. Furthermore, the participants in our study perceived that hospital managers did not place a strong emphasis on addressing DBs. This finding is consistent with a previous study which demonstrated that hospital managers had more tendency to take nurses’ DBs more seriously than those of physicians, with a significant difference between the two groups. This difference can be related to higher position and social status of physicians compared to nurses in Iran and considering the fact that most authorities and managers in the ministry of health also physicians. As a result, managers may exhibit lower tendency to address physicians’ DBs [12]. In a survey conducted by Fast et al. in 2020, a minority of participants reported DBs, with over 30% admitting that they had never reported such behaviors. Furthermore, only 21% reported satisfaction with managers’ responses to reported cases of DBs. Only one in five participants were satisfied with how managers addressed such reports [31].
The participants uniformly perceived that there were no effective rules to address DBs. This is consistent with a previous research, in which more than half of the participants reported a lack of policies or strategies to manage such behaviors [12]. Saghaei et al. found that the majority of respondents in their study believed that there were no established behavioral guidelines to prevent DBs. Even though such rules existed, there would be insufficient executive support for their implementation [20]. Hospitals require well-defined policies and standards to mitigate the incidence of DBs and hospital managers should encourage the personnel to report DBs and inform them about the adverse consequences of DBs and the benefits of timely reporting for effective management and prevention. On the other hand, appropriate feedback from officials to reported cases can enhance the satisfaction of personnel with managerial performance in addressing DBs. These strategies have the potential to improve job satisfaction, productivity and employee commitment in the healthcare settings [31, 32].
Both physicians and nurses perceived that the attitudes of officials towards DBs can significantly influence the efforts made to control and reduce such behaviors. In Maddineshat et al.’s study, the majority of participants believed that healthcare organizations can implement policies to effectively address these behaviors [12]. Fast et al. also suggested that clear policies and programs are essential to address DBs and enhance employee satisfaction in the healthcare centers. To comprehensively address DBs, healthcare centers should establish a reporting system for physicians, while officials respond appropriately to the reports. This approach is pivotal in building trust and ensuring the implementation of necessary changes [31]. Failure to report DBs can normalize the behaviors over time. Hospital managers should delve into the factors contributing to staff reluctance to report DBs within the system. Younger staff, those without management responsibilities, anesthesiologists, and surgeons refuse to report DBs more than nurses [31].
The participants in our study indicated that the primary barriers to reporting DBs were the feeling that nothing ever changes and lack of confidentiality. This finding is consistent with other studies that identified system inefficiency and frustration with the lack of change as the main reasons for not reporting DBs [12, 18]. However, in one study, fear of retaliation was found to be the most important barrier, although concerns about the lack of change and confidentiality also were reported [20]. Educational interventions and an appropriate reporting system can improve the reporting of DBs [33].
This study observed a significant difference in taking nurse DBs seriously, consistent with Maddineshat et al.’s study [18]. According to the nurses in this study, the hospital authorities consider the nurse DBs more serious than the physician DBs. Furthermore, a significant difference was detected between the nurses’ and physicians’ responses to the seriousness of the impact of DBs on patient outcomes. According to nurses, the impact of DBs on patient outcomes are more serious.
There were a number of limitations to our study. The study was limited to the emergency departments of selected teaching hospitals, and the results cannot be generalized to other departments or hospitals. Also, we used self-reported data, which may be subject to response bias. There was also a small sample size due to difficulty in recutting more samples. Finally, there was a lack of study on the long-term effects of DBs on patient safety, quality of care, patient mortality, nurse satisfaction, physician satisfaction, and patient satisfaction. Based on the findings of study, it is crucial to ensure that medical students, medical staff, hospital managers, and policymakers, understand and recognize the DBs, for addressing the issue effectively. Hospital managers should be informed about the prevalence and impact of DBs. They should take steps to develop clear policies and guidelines to identify, prevent, or manage the occurrence of DBs among medical staff. Moreover, regular monitoring and assessment of these policies is essential to ensure they are implemented effectively. Practical workshops on communication skills should be held to improve the communication and collaboration between physicians and nurses. Given the significant adverse effects of DBs, interventions should be designed and conducted to reduce their incidence and consequences. These interventions can involve educational interventions, support interventions, and strategies to create a culture of respect and collaboration within healthcare settings.
Conclusion
The DBs are prevalent in the emergency departments of selected hospitals in Iran, according to nurses and physicians. Since DBs can negatively affect the well-being of medical staff, patient safety, and quality of nursing care, effective interventions, including policy development, communication skills training, and educational intervention, are needed to improve nurse/physician relationships and reduce DBs in the emergency departments.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Alborz University of Medical Sciences (Code: IR.ABZUMS.REC.1398.144). All methods were carried out in accordance with relevant guidelines and regulation. Informed consent was obtained from all participants.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization and study design: Maryam Aghabarary, Roohangiz Norouzinia and Alan H Rosenstein; Data collection: Roohangiz Norouzinia; Data analysis: Pardis Rahmatpour; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Alborz University of Medical Sciences and all participants for their cooperation.
References
- Moreno-Leal P, Leal-Costa C, Díaz-Agea JL, Jiménez-Ruiz I, Ramos-Morcillo AJ, Ruzafa-Martínez M, et al. Disruptive behavior at hospitals and factors associated to safer care: A Systematic Review. Healthcare. 2021; 10(1):19. [DOI:10.3390/healthcare10010019] [PMID]
- Oliveira RM, Silva LM, Guedes MV, Oliveira AC, Sánchez RG, Torres RA. [Analyzing the concept of disruptive behavior in healthcare work: An integrative review (Portuguese)]. Rev Esc Enferm USP. 2016; 50(4):695-704. [DOI:10.1590/S0080-623420160000500021] [PMID]
- Dang D, Nyberg D, Walrath JM, Kim MT. Development and validation of the Johns Hopkins Disruptive Clinician Behavior Survey. Am J Med Qual. 2015; 30(5):470-6. [DOI:10.1177/1062860614544193] [PMID]
- Afzali M, Mokhtari Nouri J, Ebadi A, Khademolhoseyni SM, Rejeh N. Perceived distributive injustice, the key factor in nurse's disruptive behaviors: A qualitative study. J Caring Sci. 2017; 6(3):237-47. [DOI:10.15171/jcs.2017.023] [PMID]
- Villafranca A, Fast I, Jacobsohn E. Disruptive behavior in the operating room: Prevalence, consequences, prevention, and management. Curr Opin Anaesthesiol. 2018; 31(3):366-74. [DOI:10.1097/ACO.0000000000000592] [PMID]
- Oyeleye O, Hanson P, O'Connor N, Dunn D. Relationship of workplace incivility, stress, and burnout on nurses' turnover intentions and psychological empowerment. J Nurs Adm. 2013; 43(10):536-42. [DOI:10.1097/NNA.0b013e3182a3e8c9] [PMID]
- Lachman VD. Ethical issues in the disruptive behaviors of incivility, bullying, and horizontal/lateral violence. Medsurg Nurs. 2014; 23(1):56-60. [PMID]
- Harolds JA. Quality and safety in healthcare, part LXXIV: Combating disruptive behavior in healthcare workers. Clin Nucl Med. 2022; 47(1):e1-3. [DOI:10.1097/RLU.0000000000003058] [PMID]
- Laschinger HK. Impact of workplace mistreatment on patient safety risk and nurse-assessed patient outcomes. J Nurs Adm. 2014; 44(5):284-90. [DOI:10.1097/NNA.0000000000000068] [PMID]
- Commission J. Behaviors that undermine a culture of safety. Sentinal Event Alert. 2008; 40:1-3. [Link]
- Hicks S, Stavropoulou C. The effect of health care professional disruptive behavior on patient care: A systematic review. J Patient Saf. 2022; 18(2):138-43. [DOI:10.1097/PTS.0000000000000805] [PMID]
- Maddineshat M, Hashemi M, Tabatabaeichehr M. Evaluation of the disruptive behaviors among treatment teams and its reflection on the therapy process of patients in the operating room: The impact of personal conflicts. J Educ Health Promot. 2017; 6:69. [DOI:10.4103/jehp.jehp_47_16] [PMID]
- Villafranca A, Hiebert B, Hamlin C, Young A, Parveen D, Arora RC, et al. Prevalence and predictors of exposure to disruptive behaviour in the operating room. Can J Anaesth. 2019; 66(7):781-94. [DOI:10.1007/s12630-019-01333-8] [PMID]
- Leape LL, Shore MF, Dienstag JL, Mayer RJ, Edgman-Levitan S, Meyer GS, et al. Perspective: A culture of respect, part 1: The nature and causes of disrespectful behavior by physicians. Acad Med. 2012; 87(7):845-52. [DOI:10.1097/ACM.0b013e318258338d] [PMID]
- Afzali M, Mokhtari J, Ebadi A, Rezaiye M. Factors facilitating destructive behaviors in nurses towards other healthcare workers in Iranian Healthcare Organizations: A qualitative study. 2021; [Unpublished]. [DOI:10.21203/rs.3.rs-189820/v1]
- Rosenstein AH, Naylor B. Incidence and impact of physician and nurse disruptive behaviors in the emergency department. J Emerg Med. 2012; 43(1):139-48. [DOI:10.1016/j.jemermed.2011.01.019] [PMID]
- Teymourzadeh E, Rashidian A, Arab M, Akbari-Sari A, Hakimzadeh SM. Nurses exposure to workplace violence in a large teaching hospital in Iran. Int J Health Policy Manag. 2014; 3(6):301-5. [DOI:10.15171/ijhpm.2014.98] [PMID]
- Maddineshat M, Rosenstein AH, Akaberi A, Tabatabaeichehr M. Disruptive behaviors in an emergency department: the perspective of physicians and nurses. J Caring Sci. 2016; 5(3):241-9. [DOI:10.15171/jcs.2016.026] [PMID]
- Rosenstein AH, O'Daniel M. A survey of the impact of disruptive behaviors and communication defects on patient safety. Jt Comm J Qual Patient Saf. 2008; 34(8):464-71. [DOI:10.1016/S1553-7250(08)34058-6] [PMID]
- Saghaei M, Ahmadzadeh G, Haghighat S. The prevalence and outcome of disruptive behaviors in nurses and physicians: A descriptive study in Iranian Health care context. Iran J Psychiatry Behav Sci. 2020. 14(4):e106514. [DOI:10.5812/ijpbs.106514]
- Antoniadis S, Passauer-Baierl S, Baschnegger H, Weigl M. Identification and interference of intraoperative distractions and interruptions in operating rooms. J Surg Res. 2014; 188(1):21-9. [DOI:10.1016/j.jss.2013.12.002] [PMID]
- Norouzinia R, Yarmohammadian MH, Ferdosi M, Masoumi G, Ebadi A. [Professional resilience among trauma emergency department nurses in Iran: A qualitative study (Persian)]. Adv J Emerg Med. 2020; 4(3):9. [Link]
- Laschinger HK, Grau AL, Finegan J, Wilk P. New graduate nurses' experiences of bullying and burnout in hospital settings. J Adv Nurs. 2010; 66(12):2732-42. [DOI:10.1111/j.1365-2648.2010.05420.x] [PMID]
- Rosenstein AH, O'Daniel M. Disruptive behavior and clinical outcomes: Perceptions of nurses and physicians. Am J Nurs. 2005; 105(1):54-64. [DOI:10.1097/00000446-200501000-00025] [PMID]
- Saxton R, Hines T, Enriquez M. The negative impact of nurse-physician disruptive behavior on patient safety: A review of the literature. J Patient Saf. 2009; 5(3):180-3. [DOI:10.1097/PTS.0b013e3181b4c5d7] [PMID]
- Berry PA, Gillespie GL, Gates D, Schafer J. Novice nurse productivity following workplace bullying. J Nurs Scholarsh. 2012; 44(1):80-7. [DOI:10.1111/j.1547-5069.2011.01436.x] [PMID]
- Rosenstein AH. Physician disruptive behaviors: Five year progress report. World J Clin Cases. 2015; 3(11):930-4. [DOI:10.12998/wjcc.v3.i11.930] [PMID]
- Swafford L. Lateral violence in the emergency department [master thesis]. Boiling Springs: Gardner-Webb University; 2014. [Link]
- Vessey JA, Demarco RF, Gaffney DA, Budin WC. Bullying of staff registered nurses in the workplace: A preliminary study for developing personal and organizational strategies for the transformation of hostile to healthy workplace environments. J Prof Nurs. 2009; 25(5):299-306. [DOI:10.1016/j.profnurs.2009.01.022] [PMID]
- Walrath JM, Dang D, Nyberg D. An organizational assessment of disruptive clinician behavior: Findings and implications. J Nurs Care Qual. 2013; 28(2):110-21. [DOI:10.1097/NCQ.0b013e318270d2ba] [PMID]
- Fast I, Villafranca A, Henrichs B, Magid K, Christodoulou C, Jacobsohn E. Disruptive behaviour in the operating room is under-reported: An international survey. Can J Anaesth. 2020; 67(2):177-85. [DOI:10.1007/s12630-019-01540-3] [PMID]
- Moreira FTLDS, Callou RCM, Albuquerque GA, Oliveira RM. [Effective communication strategies for managing disruptive behaviors and promoting patient safety (Portuguese)]. Revista Gaucha de Enfermagem. 2019; 40(spe):e20180308. [DOI:10.1590/1983-1447.2019.20180308] [PMID]
- Katz MG, Rockne WY, Braga R, McKellar S, Cochran A. An improved patient safety reporting system increases reports of disruptive behavior in the perioperative setting. American Journal of Surgery. 2020; 219(1):21-26. [DOI:10.1016/j.amjsurg.2019.05.012] [PMID]
Type of Study: Research |
Subject:
Psychology
Received: 2023/09/2 | Accepted: 2023/11/23 | Published: 2024/01/1
Received: 2023/09/2 | Accepted: 2023/11/23 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |