Sun, Jul 27, 2025
[Archive]
Volume 2, Issue 1 (Autumn 2023)
CPR 2023, 2(1): 37-46 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shahhosseini Z, Nikbakht R, Hajipour L, Ghalesari S Z K, Tabaghdehi M H. Factors Predicting Fear of COVID-19 and the Related Anxiety Among Pregnant Women in Mazandaran, Northern Iran. CPR 2023; 2 (1) :37-46
URL: http://cpr.mazums.ac.ir/article-1-78-en.html
URL: http://cpr.mazums.ac.ir/article-1-78-en.html
Zohreh Shahhosseini 

 , Roya Nikbakht
, Roya Nikbakht 

 , Leila Hajipour
, Leila Hajipour 

 , Seyedeh Zeinab Khoshroo Ghalesari
, Seyedeh Zeinab Khoshroo Ghalesari 

 , Monirolsadate Hosseini Tabaghdehi
, Monirolsadate Hosseini Tabaghdehi 




 , Roya Nikbakht
, Roya Nikbakht 

 , Leila Hajipour
, Leila Hajipour 

 , Seyedeh Zeinab Khoshroo Ghalesari
, Seyedeh Zeinab Khoshroo Ghalesari 

 , Monirolsadate Hosseini Tabaghdehi
, Monirolsadate Hosseini Tabaghdehi 


Department of Midwifery, Health Reproductive Research Center, Sari Branch, Islamic Azad University, Sari, Iran.
Full-Text [PDF 637 kb]
(207 Downloads)
| Abstract (HTML) (816 Views)
Full-Text: (335 Views)
Introduction
Women experience subtle mental and physical changes during pregnancy and transition into motherhood. The perinatal period is often associated with mental disorders such as fear and anxiety [1]. The World Health Organization (WHO) has reported that, globally, approximately 10% of pregnant women and 13% of those who have just given birth suffer from a mental disorder. In developing countries, the prevalence is higher, reaching 15.6% during pregnancy and 19.8% in the postpartum period [2]. One of the reasons for the anxiety of pregnant women is the concern about the fetus’s health and the childbirth outcome. Moreover, natural disasters, such as the COVID-19 pandemic, adversely affect pregnant women’s mental health [3]. The pandemic increased stress, anxiety, and depression among pregnant women due to social distancing, concern about the health of family members, and not receiving regular prenatal care [4, 5]. Studies have reported that the prevalence of anxiety among pregnant women during the COVID-19 pandemic ranges from 26% to 57% [6].
Prenatal anxiety and depression can lead to changes in physical activity, nutrition, and sleep quality, affecting the mother’s mood and fetal development [7]. Prenatal anxiety and depression are linked to increased risks of miscarriage, premature birth, low birth weight, and low Apgar scores at birth [8]. Children of mothers with significant stress during pregnancy are more prone to cognitive and behavioral problems [9]. Prenatal anxiety and depression are also associated with changes in children’s brain structure and function [10]. Studies during the COVID-19 pandemic have identified various factors related to COVID-19-related fear and anxiety in pregnant women. The factors including the source of information, food insecurity, ethnicity, social status, history of prenatal anxiety, chronic diseases, pre-pregnancy body mass index, unplanned pregnancy, and lack of spouse support are related to fear of COVID-19, while the factors such as mother’s age, economic status, and concerns about routine care during pregnancy are associated with anxiety about COVID-19 [11, 12]. In Iran, there are also some studies on the fear and anxiety of pregnant women during the COVID-19 pandemic [13, 14]. Given the influence of cultural and social factors on fear and anxiety, there is a need for more studies on the predictive factors to use the results to cope with future crisis situations and pandemics.
Given the potential negative psychological consequences mentioned above, it is crucial to assess the level of mental disorders, including fear and anxiety, in pregnant women during the pandemic, and to identify predictive factors so that targeted interventions can be implemented quickly. Therefore, this study aims to identify the factors predicting COVID-19- related fear and anxiety among pregnant women in Mazandaran, northern Iran.
Materials and Methods
This cross-sectional study was carried out in six cities of Mazandaran province from June to February 2021, on 450 pregnant women referred to the health centers affiliated to Mazandaran University of Medical Sciences. The inclusion criteria were singleton pregnancy, gestational age >32 weeks, having a smartphone, and consent to participate in the study. Exclusion criteria were the death of a close relative in the past six months, infection with COVID-19 during pregnancy, any medical complications related to pregnancy, mental or physical disorders diagnosed by a physician, history of premature birth, and history recurrent miscarriage. Based on a previous study which indicated a 43.9% prevalence of COVID-19-related anxiety among pregnant women [13], and considering a confidence level of 95%, a accuracy level of 0.05, and a error margin of 5%, the sample size was calculated to be 450. A multi-stage sampling approach was used to select participants. In this regard, the province was divided into three regions: East, West, and Center. Two cities were then randomly selected from each region. Neka and Behshahr cities were chosen from the eastern region; Tonekabon and Noor cities from the western region; and Sari and Miandorud cities from the central region. Then, health centers from each city were randomly selected.
For data collection, the questionnaires were completed online by women who had a smartphone. Those without a smartphone or those not intended to complete the questionnaire online were given a paper version. The questionnaires were:
● Sociodemographic/pregnancy form, which surveys age, husband’s age, educational level, husband’s education level, occupation, husband’s occupation, number of pregnancies, number of living children, use of assisted reproductive technologies, unwanted/wanted pregnancy, and history of COVID-19 infection among close contacts during the current pregnancy.
● Fear of COVID-19 scale (FCV-19S): This scale consists of 7 items rated on a 5-point Likert scale from 1 to 5, with a total score ranging from 7 to 35. Its reliability has been validated with a Cronbach’s α of 0.82 and a correlation coefficient of 0.72 [15]. In our study, the Cronbach’s α for the entire scale was calculated to be 0.89, and the minimum α value for each item was 0.87.
● Corona disease anxiety scale (CDAS): This scale has 18 items scored on a Likert scale from 0 to 3, with a total score ranging from 0 to 54. The reliability of this instrument has been confirmed with a Cronbach’s α of 0.919 [16]. In our study, the Cronbach’s α for the entire scale was calculated to be 0.96, and the minimum α value for each item was 0.95.
The data analysis was performed in SPSS software, version 24, and STATA software, version 17, applications, and the significance level was set at 0.05. The categorical data were described using frequency and percentage, while continuous data were described using Mean±standard deviations values. The normality of the data distribution related to fear and anxiety was first assessed using the Kolmogorov-Smirnov test. Given the lack of normality, the generalized linear model (GLM) with gamma distribution a logarithmic link function was used to analyze the data. In this model, an exponential Fourier transform is applied to interpret the coefficients; a coefficient value less than one suggests a reduction, while a coefficient greater than one indicates an increase.
Results
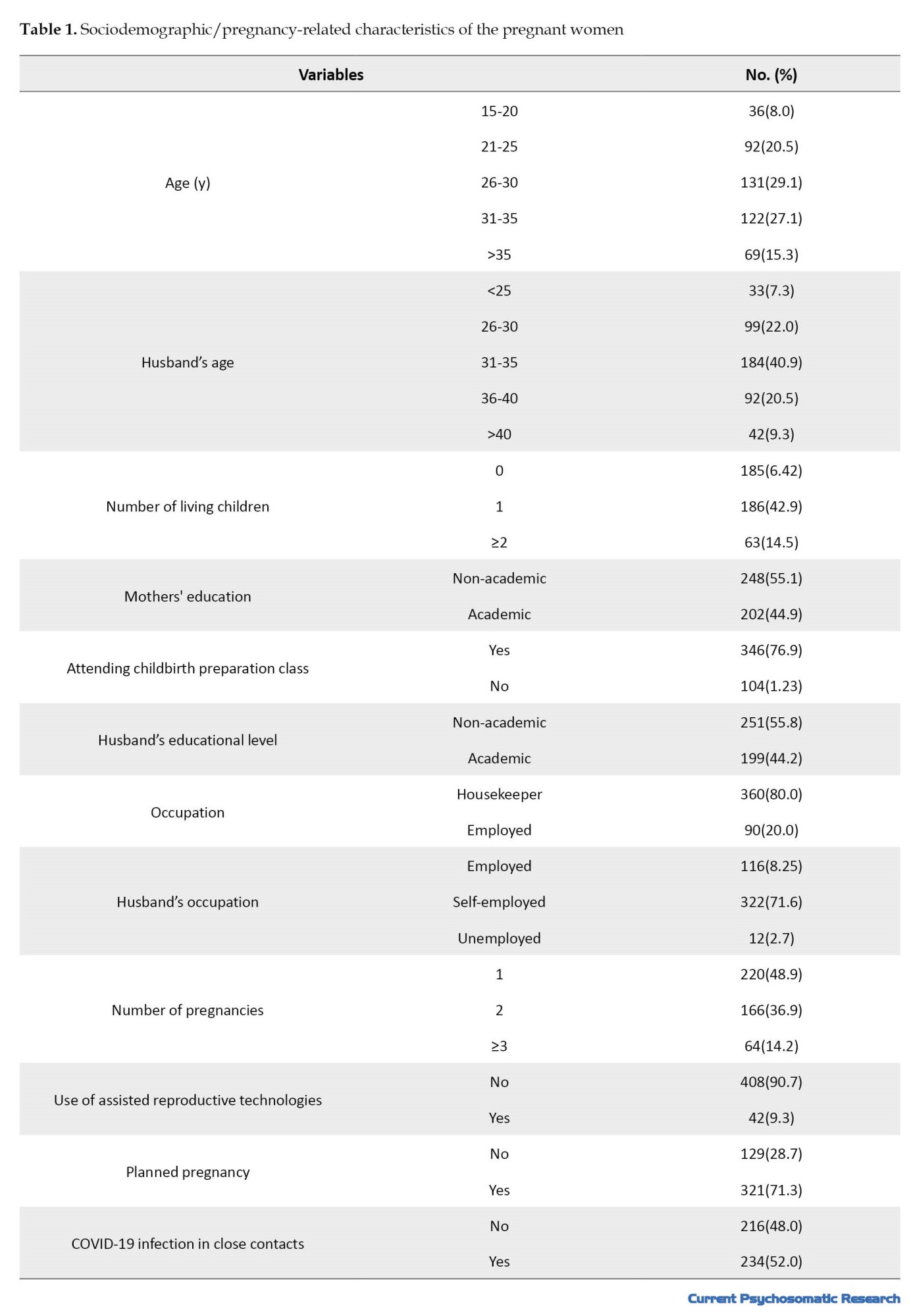
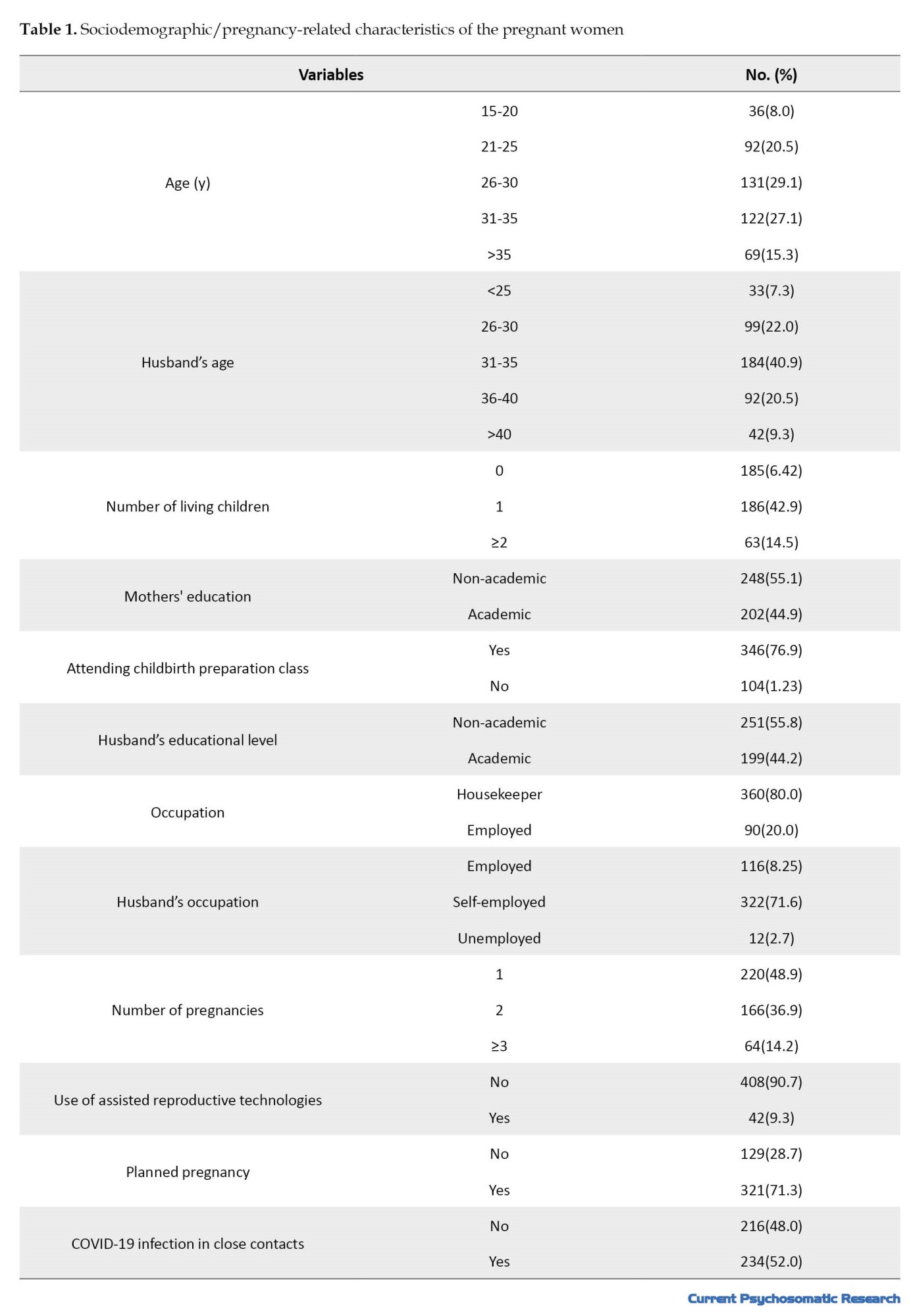
The majority of participants were in the age group of 26-30 years (29.1%) and their husbands’ age was mostly in a range of 31-35 years (40.9%). Additionally, 47.4% had a history of childbirth, while 42.6% had no such history. Other demographic characteristics are presented in Table 1.
The mean scores for COVID-19-related fear and anxiety were 21.89±5.87 and 16.63±11.71, respectively.
In the crude model, fear of COVID-19 was significantly associated with factors such as occupation, husband’s occupation, use of assisted reproductive technologies, geographic region, and COVID-19-related anxiety (P<0.05). After adjusting the model based on the GLM, age, number of pregnancies, number of living children, and COVID-19-related anxiety were found to be significantly associated with fear of COVID-19 (P<0.05) (Table 2).
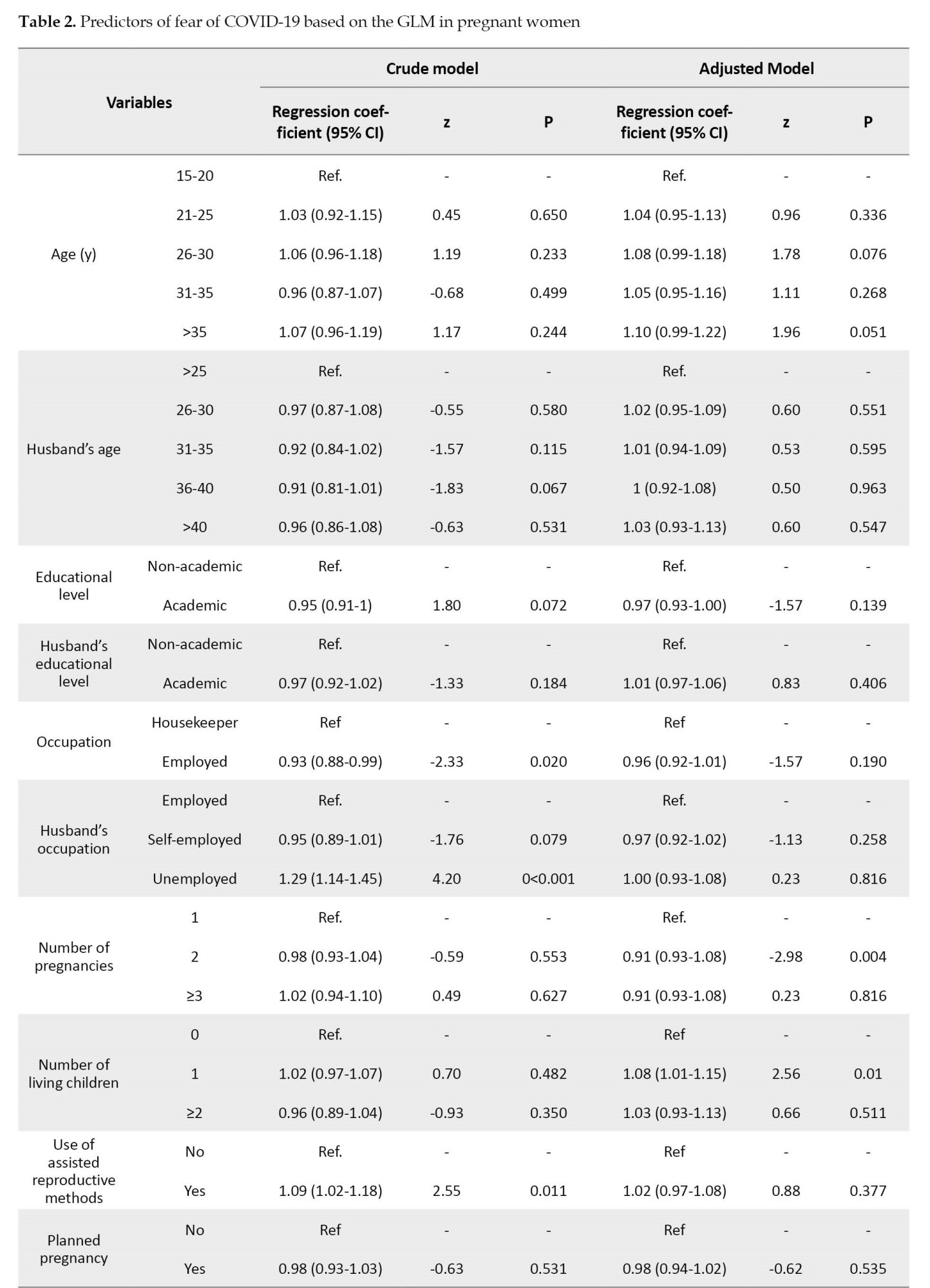
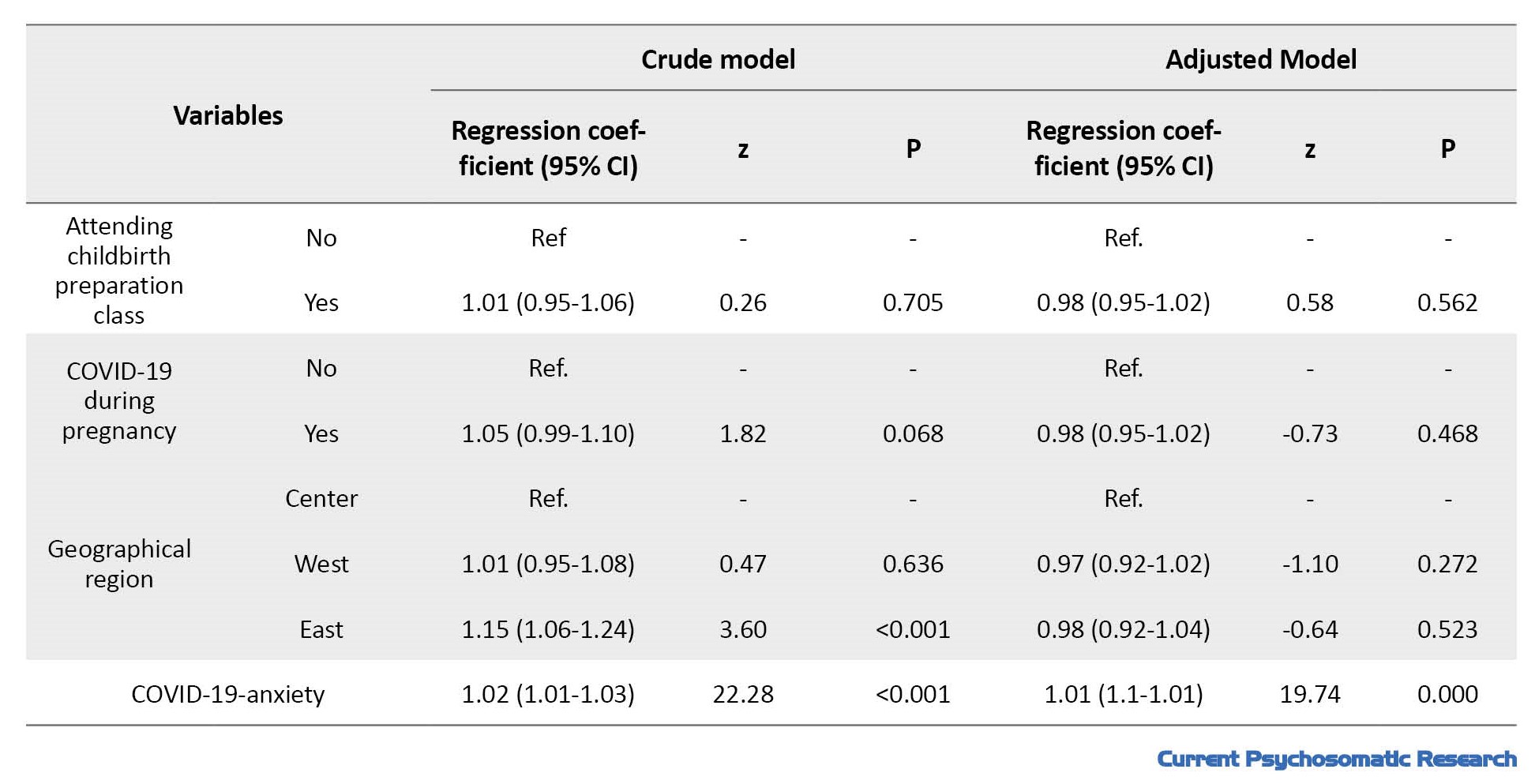
The estimated coefficient value for pregnant women aged >35 years was 1.11, indicating an increase in fear by 0.11 compared to those aged 15-20 years. The estimated coefficient values for women with two pregnancies and those with three or more pregnancies were 0.90 and 0.91, respectively, suggesting a decrease in fear of COVID-19 by 0.10 and 0.09 in them compared to the first-time pregnant women. Moreover, the fear of COVID-19 for women with one child, compared to those without children, increased by 0.09. Moreover, for every one unit increase in COVID-19-related anxiety, the fear of COVID-19 increased by 0.02.
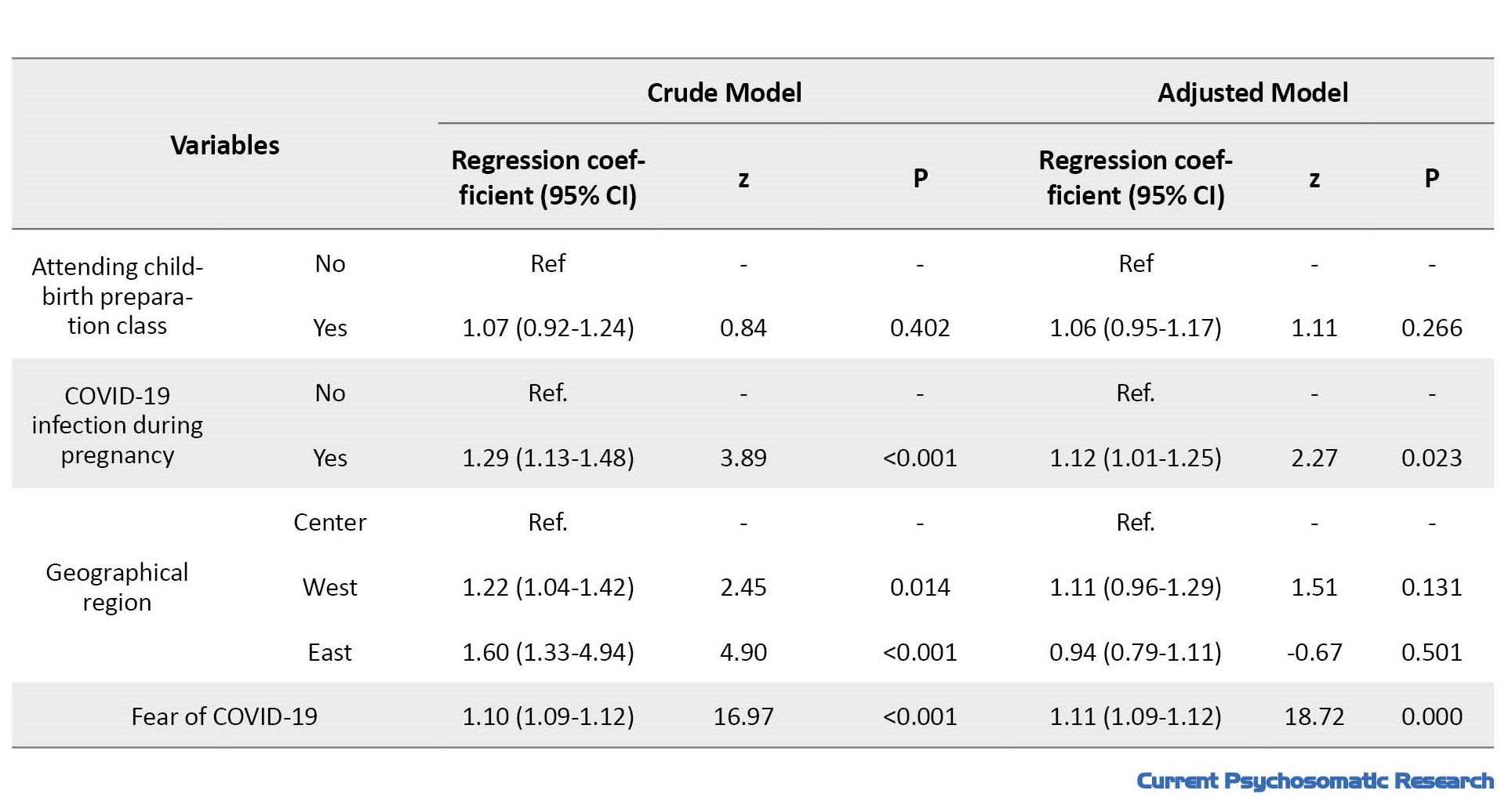
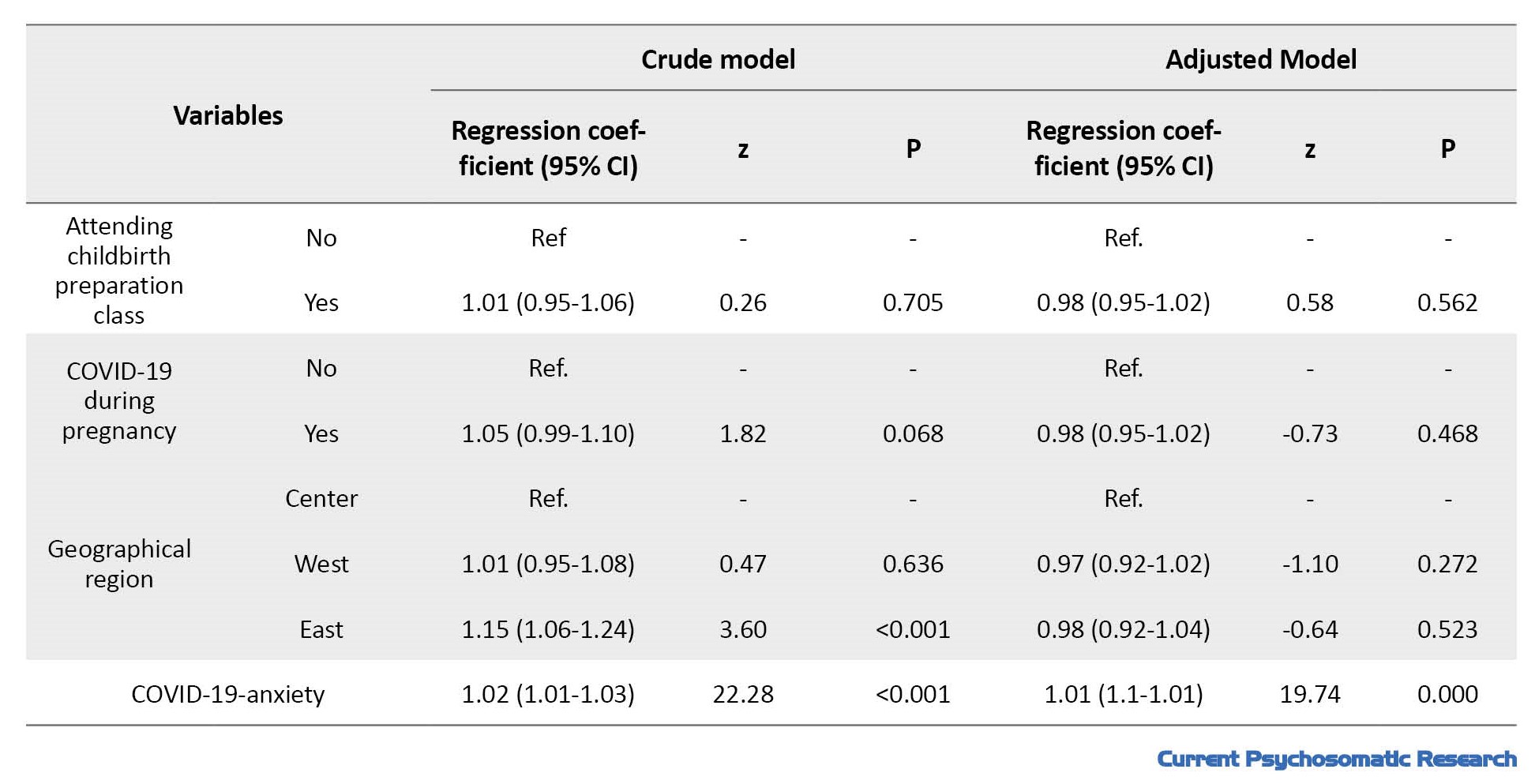
Based on the unadjusted (crude) model, there was a significant relationship between COVID-19-related anxiety and husband’s age, husband’s occupation, use of assisted reproductive methods, contracting COVID-19 during pregnancy, geographic region, and fear of COVID-19 (P<0.05). After adjusting the model, the number of pregnancies, contracting COVID-19 during pregnancy and fear of COVID-19 were significantly related to COVID-19-related anxiety (P<0.05) (Table 3).
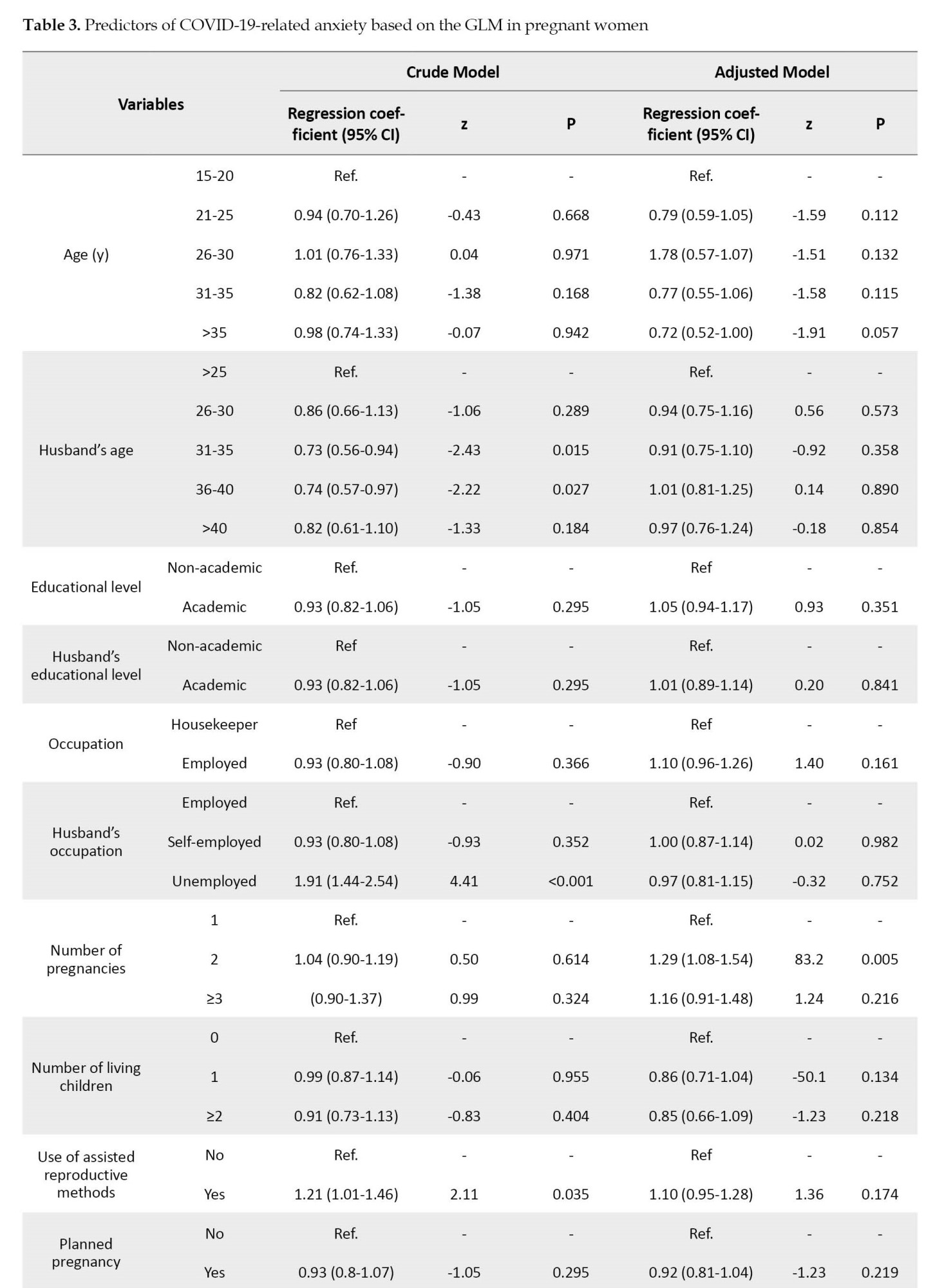
The estimated coefficient value for women with two pregnancies was 1.29, indicating that the COVID-19-related anxiety increased by 0.29 in this group.
Discussion
In this study, using the GLM, the factors of age, number of pregnancies, number of living children, and COVID-19-related anxiety were found to be the predictors of the fear of COVID-19 in pregnant women living in northern Iran. On the other hand, the number of pregnancies, COVID-19 infection in close contacts, and fear of COVID-19 were found to be the predictors of COVID-19-related anxiety in these women. The mean score of FCV-19S in pregnant women in our study was about 22%, which is consistent with the findings of Salehi et al. and Naghizadeh et al. [14, 17]. A meta-analysis reported a mean score of 18.57 for the fear of COVID-19, where women had higher fear than men (20.67 vs. 18.21) [18]. A study in Japan found that pregnant women’s fear of COVID-19 was higher than that of general population, students, and nurses [19]. In our study, the mean score of CDAS was 17. In a study in Alborz province, the mean anxiety score of pregnant women was 15.45 [14]. Lack of knowledge about the virus, lack of sufficient support from significant others such as health providers and spouses, applied restrictions, isolation [2], lack of proper prenatal care, lack of social support, and physical inactivity have been reported to have an effective role in the anxiety of pregnant women during the COVID-19 pandemic [3].
In this study, age was found to be associated with the fear of COVID-19, where the highest level of fear was observed in women aged >35 years. This is against the results of Fan et al., who reported that younger pregnant women experienced higher levels of mental disorders, such as fear and anxiety [6]. One possible explanation for the greater fear among older pregnant women can be that adaptability decreases with aging [20]. A study in Pakistan reported no correlation between COVID-19 fear and age [20]. This discrepancy can be due to differences in sample size and gestational age women.
We found that the fear of COVID-19 level was higher among multiparous women compared to nulliparous women. In a study, no association between the number of pregnancies and fear of COVID-19 was found [20]. A study in Canada revealed that women experiencing their first pregnancy had more fear of COVID-19 than those with second pregnancy [21]. The higher fear in multiparous women during the pandemic can be due to their worry about the health of other children, which can increase their fear. The number of pregnancies was also found to predict the COVID-19-related anxiety, where multiparous women exhibited higher anxiety compared to primiparous women. These findings are consistent with the results of Effati-Daryani et al. [13]. However, there are studies with opposite results. For example, Duncan et al. observed higher anxiety levels in primiparous women [21], while Rezaei et al. found no significant difference in anxiety between primiparous and multiparous women [22]. One possible reason for the lower anxiety level in pregnant women with low number of pregnancies can be their increased interaction with healthcare providers, and receiving more comprehensive and accurate information.
Furthermore, we found a significant relationship between the fear of COVID-19 and COVID-19-related anxiety in pregnant women. A Canadian study reported that women who had fear of COVID-19 were 1.2 times more anxious [21]. The infection with COVID-19 in close contacts during pregnancy was also significantly associated with increased COVID-19-related anxiety. The source of fear is often known or external factors, while the source of anxiety may be unknown threat or internal conflict. Although anxiety is a natural and adaptive response, it can become pathological and impair the ability to successfully cope with various challenges and/or stressful events [23]. Given that pregnant women have high levels of COVID-19-related anxiety during the pandemic, they should receive more attention and emotional support during such critical situations.
Conclusion
Age, number of pregnancies, number of living children, COVID-19-related anxiety are the predictors of the fear of COVID-19, while the number of pregnancies, infection with COVID-19 among close contacts, and fear of COVID-19 are the predictors of COVID-19-related anxiety in pregnant women. The low levels of fear of COVID-19 and COVID-19-related anxiety among pregnant women in this study can indicate successful efforts by health centers and mass media to control negative emotions during the pandemic. The health professionals can significantly contribute to reducing pregnant women’s fear and anxiety by using group and collective training methods
Limitations
One limitation of this study was its cross-sectional design. In this regard, the observed associations between demographic variables and the symptoms of fear and anxiety may not accurately reflect causal relationships due to temporality bias. The fear and anxiety variables were measured using self-report tools, which can lead to information bias. To mitigate this bias, participants were reassured about the confidentiality of their data.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles such as obtaining written informed consent, providing a clear explanation of the research objectives to the participants, ensuring the confidentiality of the collected information, were considered in this study. The ethical approval was obtained from Mazandaran University of Medical Sciences (Code: IR.MAZUMS.REC.1400.174).
Funding
This study was extracted from a research project (number: 9065), funded by Mazandaran University of Medical Sciences.
Authors' contributions
Conceptualization and Supervision: Zohreh Shahhosseini and Monirolsadate Hosseini Tabaghdehi; Methodology: Zohreh Shahhosseini, Monirolsadate Hosseini Tabaghdehi and Roya Nikbakht; Investigation, Writing – original draft, and Writing – review & editing: All authors; Data collection: Leila Hajipour and Seyedeh Zeinab Khoshroo Ghalesari; Data analysis: Roya Nikbakht, Zohreh Shahhosseini and Monirolsadate Hosseini Tabaghdehi; Funding acquisition and Resources: Zohreh Shahhosseini and Monirolsadate Hosseini Tabaghdehi.
Conflict of interest
The authors declared no conflict of interest
Acknowledgments
The authors would like to thank the Deputy for Research of Mazandaran University of Medical Sciences for financial support.
References
Women experience subtle mental and physical changes during pregnancy and transition into motherhood. The perinatal period is often associated with mental disorders such as fear and anxiety [1]. The World Health Organization (WHO) has reported that, globally, approximately 10% of pregnant women and 13% of those who have just given birth suffer from a mental disorder. In developing countries, the prevalence is higher, reaching 15.6% during pregnancy and 19.8% in the postpartum period [2]. One of the reasons for the anxiety of pregnant women is the concern about the fetus’s health and the childbirth outcome. Moreover, natural disasters, such as the COVID-19 pandemic, adversely affect pregnant women’s mental health [3]. The pandemic increased stress, anxiety, and depression among pregnant women due to social distancing, concern about the health of family members, and not receiving regular prenatal care [4, 5]. Studies have reported that the prevalence of anxiety among pregnant women during the COVID-19 pandemic ranges from 26% to 57% [6].
Prenatal anxiety and depression can lead to changes in physical activity, nutrition, and sleep quality, affecting the mother’s mood and fetal development [7]. Prenatal anxiety and depression are linked to increased risks of miscarriage, premature birth, low birth weight, and low Apgar scores at birth [8]. Children of mothers with significant stress during pregnancy are more prone to cognitive and behavioral problems [9]. Prenatal anxiety and depression are also associated with changes in children’s brain structure and function [10]. Studies during the COVID-19 pandemic have identified various factors related to COVID-19-related fear and anxiety in pregnant women. The factors including the source of information, food insecurity, ethnicity, social status, history of prenatal anxiety, chronic diseases, pre-pregnancy body mass index, unplanned pregnancy, and lack of spouse support are related to fear of COVID-19, while the factors such as mother’s age, economic status, and concerns about routine care during pregnancy are associated with anxiety about COVID-19 [11, 12]. In Iran, there are also some studies on the fear and anxiety of pregnant women during the COVID-19 pandemic [13, 14]. Given the influence of cultural and social factors on fear and anxiety, there is a need for more studies on the predictive factors to use the results to cope with future crisis situations and pandemics.
Given the potential negative psychological consequences mentioned above, it is crucial to assess the level of mental disorders, including fear and anxiety, in pregnant women during the pandemic, and to identify predictive factors so that targeted interventions can be implemented quickly. Therefore, this study aims to identify the factors predicting COVID-19- related fear and anxiety among pregnant women in Mazandaran, northern Iran.
Materials and Methods
This cross-sectional study was carried out in six cities of Mazandaran province from June to February 2021, on 450 pregnant women referred to the health centers affiliated to Mazandaran University of Medical Sciences. The inclusion criteria were singleton pregnancy, gestational age >32 weeks, having a smartphone, and consent to participate in the study. Exclusion criteria were the death of a close relative in the past six months, infection with COVID-19 during pregnancy, any medical complications related to pregnancy, mental or physical disorders diagnosed by a physician, history of premature birth, and history recurrent miscarriage. Based on a previous study which indicated a 43.9% prevalence of COVID-19-related anxiety among pregnant women [13], and considering a confidence level of 95%, a accuracy level of 0.05, and a error margin of 5%, the sample size was calculated to be 450. A multi-stage sampling approach was used to select participants. In this regard, the province was divided into three regions: East, West, and Center. Two cities were then randomly selected from each region. Neka and Behshahr cities were chosen from the eastern region; Tonekabon and Noor cities from the western region; and Sari and Miandorud cities from the central region. Then, health centers from each city were randomly selected.
For data collection, the questionnaires were completed online by women who had a smartphone. Those without a smartphone or those not intended to complete the questionnaire online were given a paper version. The questionnaires were:
● Sociodemographic/pregnancy form, which surveys age, husband’s age, educational level, husband’s education level, occupation, husband’s occupation, number of pregnancies, number of living children, use of assisted reproductive technologies, unwanted/wanted pregnancy, and history of COVID-19 infection among close contacts during the current pregnancy.
● Fear of COVID-19 scale (FCV-19S): This scale consists of 7 items rated on a 5-point Likert scale from 1 to 5, with a total score ranging from 7 to 35. Its reliability has been validated with a Cronbach’s α of 0.82 and a correlation coefficient of 0.72 [15]. In our study, the Cronbach’s α for the entire scale was calculated to be 0.89, and the minimum α value for each item was 0.87.
● Corona disease anxiety scale (CDAS): This scale has 18 items scored on a Likert scale from 0 to 3, with a total score ranging from 0 to 54. The reliability of this instrument has been confirmed with a Cronbach’s α of 0.919 [16]. In our study, the Cronbach’s α for the entire scale was calculated to be 0.96, and the minimum α value for each item was 0.95.
The data analysis was performed in SPSS software, version 24, and STATA software, version 17, applications, and the significance level was set at 0.05. The categorical data were described using frequency and percentage, while continuous data were described using Mean±standard deviations values. The normality of the data distribution related to fear and anxiety was first assessed using the Kolmogorov-Smirnov test. Given the lack of normality, the generalized linear model (GLM) with gamma distribution a logarithmic link function was used to analyze the data. In this model, an exponential Fourier transform is applied to interpret the coefficients; a coefficient value less than one suggests a reduction, while a coefficient greater than one indicates an increase.
Results
The majority of participants were in the age group of 26-30 years (29.1%) and their husbands’ age was mostly in a range of 31-35 years (40.9%). Additionally, 47.4% had a history of childbirth, while 42.6% had no such history. Other demographic characteristics are presented in Table 1.
The mean scores for COVID-19-related fear and anxiety were 21.89±5.87 and 16.63±11.71, respectively.
In the crude model, fear of COVID-19 was significantly associated with factors such as occupation, husband’s occupation, use of assisted reproductive technologies, geographic region, and COVID-19-related anxiety (P<0.05). After adjusting the model based on the GLM, age, number of pregnancies, number of living children, and COVID-19-related anxiety were found to be significantly associated with fear of COVID-19 (P<0.05) (Table 2).
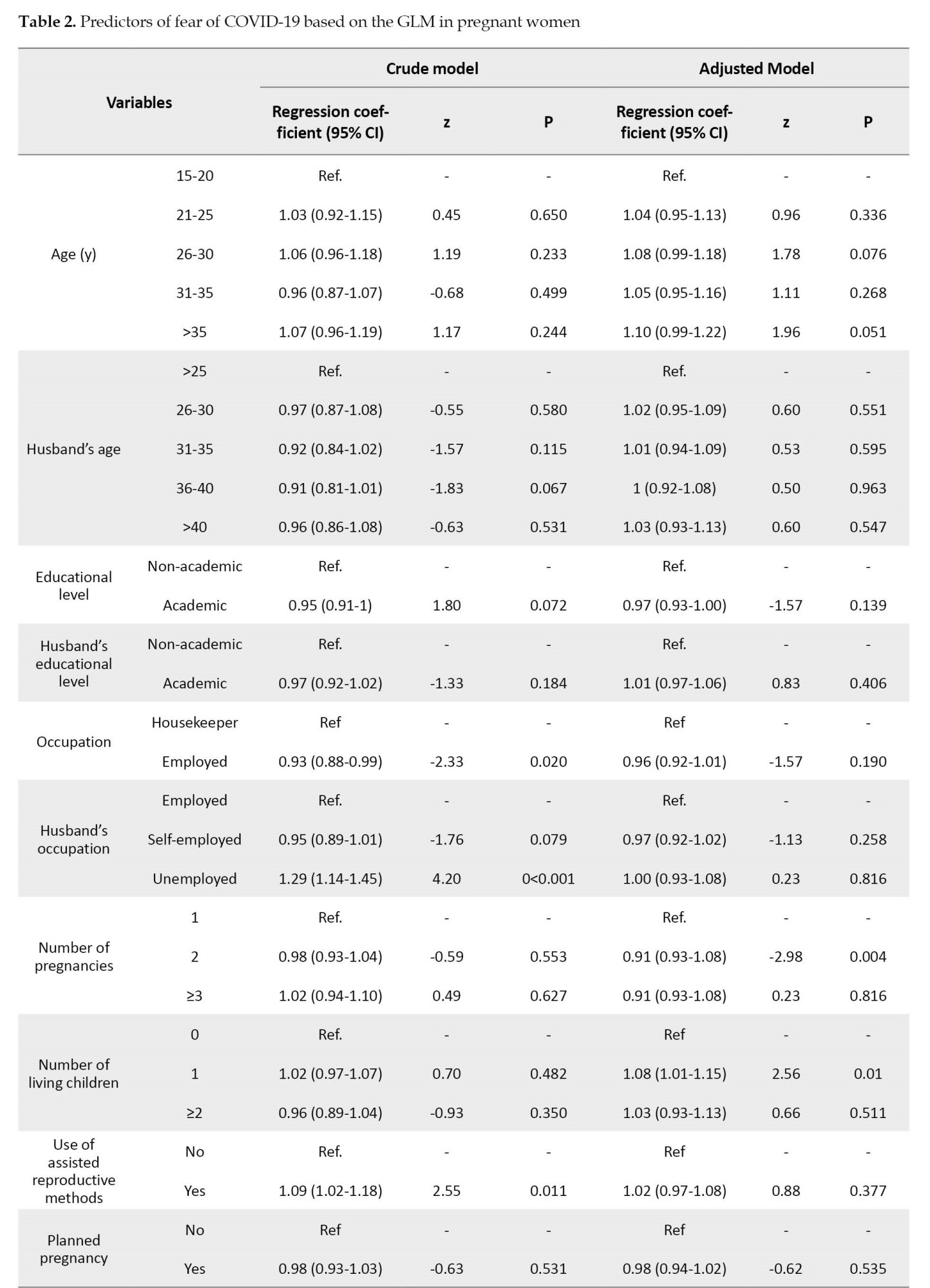
The estimated coefficient value for pregnant women aged >35 years was 1.11, indicating an increase in fear by 0.11 compared to those aged 15-20 years. The estimated coefficient values for women with two pregnancies and those with three or more pregnancies were 0.90 and 0.91, respectively, suggesting a decrease in fear of COVID-19 by 0.10 and 0.09 in them compared to the first-time pregnant women. Moreover, the fear of COVID-19 for women with one child, compared to those without children, increased by 0.09. Moreover, for every one unit increase in COVID-19-related anxiety, the fear of COVID-19 increased by 0.02.
Based on the unadjusted (crude) model, there was a significant relationship between COVID-19-related anxiety and husband’s age, husband’s occupation, use of assisted reproductive methods, contracting COVID-19 during pregnancy, geographic region, and fear of COVID-19 (P<0.05). After adjusting the model, the number of pregnancies, contracting COVID-19 during pregnancy and fear of COVID-19 were significantly related to COVID-19-related anxiety (P<0.05) (Table 3).
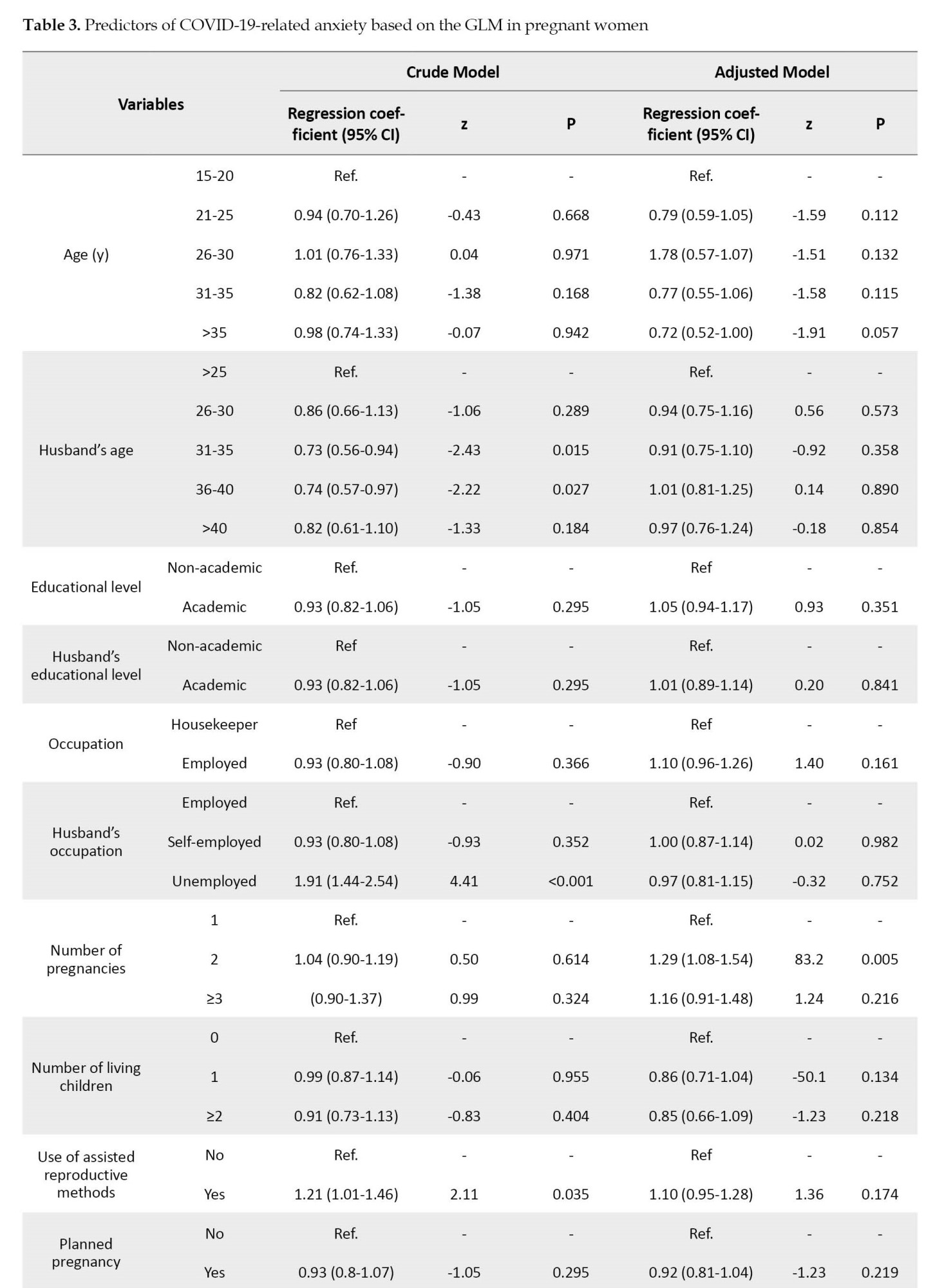
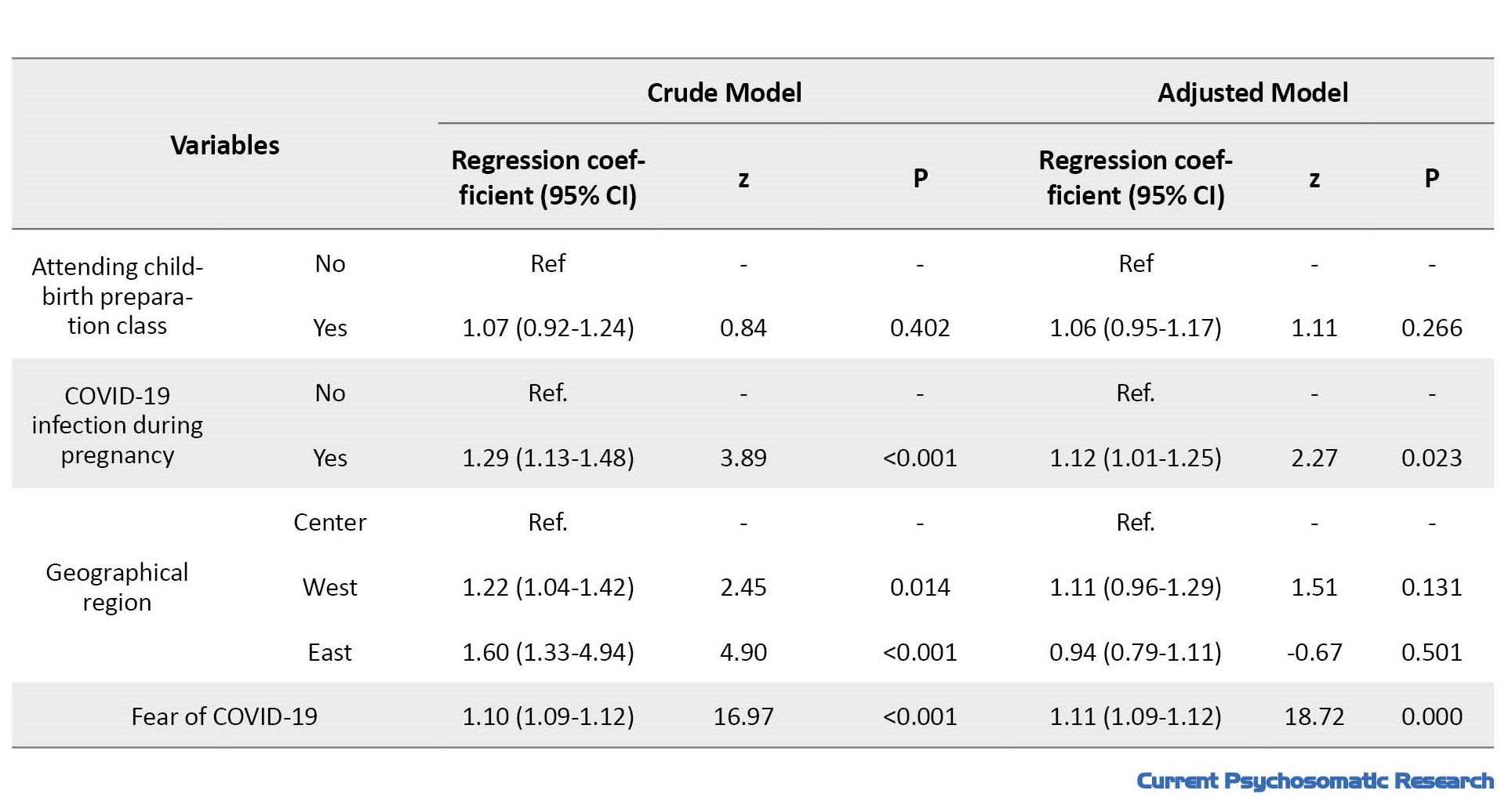
The estimated coefficient value for women with two pregnancies was 1.29, indicating that the COVID-19-related anxiety increased by 0.29 in this group.
Discussion
In this study, using the GLM, the factors of age, number of pregnancies, number of living children, and COVID-19-related anxiety were found to be the predictors of the fear of COVID-19 in pregnant women living in northern Iran. On the other hand, the number of pregnancies, COVID-19 infection in close contacts, and fear of COVID-19 were found to be the predictors of COVID-19-related anxiety in these women. The mean score of FCV-19S in pregnant women in our study was about 22%, which is consistent with the findings of Salehi et al. and Naghizadeh et al. [14, 17]. A meta-analysis reported a mean score of 18.57 for the fear of COVID-19, where women had higher fear than men (20.67 vs. 18.21) [18]. A study in Japan found that pregnant women’s fear of COVID-19 was higher than that of general population, students, and nurses [19]. In our study, the mean score of CDAS was 17. In a study in Alborz province, the mean anxiety score of pregnant women was 15.45 [14]. Lack of knowledge about the virus, lack of sufficient support from significant others such as health providers and spouses, applied restrictions, isolation [2], lack of proper prenatal care, lack of social support, and physical inactivity have been reported to have an effective role in the anxiety of pregnant women during the COVID-19 pandemic [3].
In this study, age was found to be associated with the fear of COVID-19, where the highest level of fear was observed in women aged >35 years. This is against the results of Fan et al., who reported that younger pregnant women experienced higher levels of mental disorders, such as fear and anxiety [6]. One possible explanation for the greater fear among older pregnant women can be that adaptability decreases with aging [20]. A study in Pakistan reported no correlation between COVID-19 fear and age [20]. This discrepancy can be due to differences in sample size and gestational age women.
We found that the fear of COVID-19 level was higher among multiparous women compared to nulliparous women. In a study, no association between the number of pregnancies and fear of COVID-19 was found [20]. A study in Canada revealed that women experiencing their first pregnancy had more fear of COVID-19 than those with second pregnancy [21]. The higher fear in multiparous women during the pandemic can be due to their worry about the health of other children, which can increase their fear. The number of pregnancies was also found to predict the COVID-19-related anxiety, where multiparous women exhibited higher anxiety compared to primiparous women. These findings are consistent with the results of Effati-Daryani et al. [13]. However, there are studies with opposite results. For example, Duncan et al. observed higher anxiety levels in primiparous women [21], while Rezaei et al. found no significant difference in anxiety between primiparous and multiparous women [22]. One possible reason for the lower anxiety level in pregnant women with low number of pregnancies can be their increased interaction with healthcare providers, and receiving more comprehensive and accurate information.
Furthermore, we found a significant relationship between the fear of COVID-19 and COVID-19-related anxiety in pregnant women. A Canadian study reported that women who had fear of COVID-19 were 1.2 times more anxious [21]. The infection with COVID-19 in close contacts during pregnancy was also significantly associated with increased COVID-19-related anxiety. The source of fear is often known or external factors, while the source of anxiety may be unknown threat or internal conflict. Although anxiety is a natural and adaptive response, it can become pathological and impair the ability to successfully cope with various challenges and/or stressful events [23]. Given that pregnant women have high levels of COVID-19-related anxiety during the pandemic, they should receive more attention and emotional support during such critical situations.
Conclusion
Age, number of pregnancies, number of living children, COVID-19-related anxiety are the predictors of the fear of COVID-19, while the number of pregnancies, infection with COVID-19 among close contacts, and fear of COVID-19 are the predictors of COVID-19-related anxiety in pregnant women. The low levels of fear of COVID-19 and COVID-19-related anxiety among pregnant women in this study can indicate successful efforts by health centers and mass media to control negative emotions during the pandemic. The health professionals can significantly contribute to reducing pregnant women’s fear and anxiety by using group and collective training methods
Limitations
One limitation of this study was its cross-sectional design. In this regard, the observed associations between demographic variables and the symptoms of fear and anxiety may not accurately reflect causal relationships due to temporality bias. The fear and anxiety variables were measured using self-report tools, which can lead to information bias. To mitigate this bias, participants were reassured about the confidentiality of their data.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles such as obtaining written informed consent, providing a clear explanation of the research objectives to the participants, ensuring the confidentiality of the collected information, were considered in this study. The ethical approval was obtained from Mazandaran University of Medical Sciences (Code: IR.MAZUMS.REC.1400.174).
Funding
This study was extracted from a research project (number: 9065), funded by Mazandaran University of Medical Sciences.
Authors' contributions
Conceptualization and Supervision: Zohreh Shahhosseini and Monirolsadate Hosseini Tabaghdehi; Methodology: Zohreh Shahhosseini, Monirolsadate Hosseini Tabaghdehi and Roya Nikbakht; Investigation, Writing – original draft, and Writing – review & editing: All authors; Data collection: Leila Hajipour and Seyedeh Zeinab Khoshroo Ghalesari; Data analysis: Roya Nikbakht, Zohreh Shahhosseini and Monirolsadate Hosseini Tabaghdehi; Funding acquisition and Resources: Zohreh Shahhosseini and Monirolsadate Hosseini Tabaghdehi.
Conflict of interest
The authors declared no conflict of interest
Acknowledgments
The authors would like to thank the Deputy for Research of Mazandaran University of Medical Sciences for financial support.
References
- Bayrampour H, McDonald S, Tough S. Risk factors of transient and persistent anxiety during pregnancy. Midwifery. 2015; 31(6):582-9. [DOI:10.1016/j.midw.2015.02.009] [PMID]
- WHO. Maternal Mental Health. Geneva: WHO; 2019. [Link]
- Feduniw S, Modzelewski J, Kajdy A, Sys D, Kwiatkowski S, Makomaska-Szaroszyk E, et al. Anxiety of pregnant women in time of catastrophic events, including COVID-19 pandemic: A systematic review and meta-analysis. J Psychosom Obstet Gynaecol. 2022; 43(4):400-10. [PMID]
- Hussein J. COVID-19: What implications for sexual and reproductive health and rights globally? Sex Reprod Health Matters. 2020; 28(1):1746065. [DOI:10.1080/26410397.2020.1746065] [PMID]
- Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration, UK. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet. 2020; 395(10229):1033-4. [DOI:10.1016/S0140-6736(20)30628-0] [PMID]
- Fan S, Guan J, Cao L, Wang M, Zhao H, Chen L, et al. Psychological effects caused by COVID-19 pandemic on pregnant women: A systematic review with meta-analysis. Asian J Psychiatr. 2021; 56:102533. [DOI:10.1016/j.ajp.2020.102533] [PMID]
- Coussons-Read ME. Effects of prenatal stress on pregnancy and human development: mechanisms and pathways. Obstet Med. 2013; 6(2):52-7. [DOI:10.1177/1753495x12473751] [PMID]
- Accortt EE, Cheadle AC, Dunkel Schetter C. Prenatal depression and adverse birth outcomes: An updated systematic review. Matern Child Health J. 2015; 19(6):1306-37. [DOI:10.1007/s10995-014-1637-2] [PMID]
- Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. 2014; 28(1):25-35. [DOI:10.1016/j.bpobgyn.2013.08.017] [PMID]
- Adamson B, Letourneau N, Lebel C. Prenatal maternal anxiety and children's brain structure and function: A systematic review of neuroimaging studies. J Affect Disord. 2018; 241:117-26. [DOI:10.1016/j.jad.2018.08.029] [PMID]
- Huynh T, Boise C, Kihntopf ME, Schaefer AA, Schafer M. “Fear and anxiety is what I recall the best.”: A phenomenological examination of mothers’ pregnancy experiences during COVID-19 in the United States. Midwifery. 2023; 122:103700. [DOI:10.1016/j.midw.2023.103700] [PMID]
- Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2020; 277:5-13. [DOI:10.1016/j.jad.2020.07.126] [PMID]
- Effati-Daryani F, Zarei S, Mohammadi A, Hemmati E, Ghasemi Yngyknd S, Mirghafourvand M. Depression, stress, anxiety and their predictors in Iranian pregnant women during the outbreak of COVID-19. BMC Psychol. 2020; 8(1):99.[DOI:10.1186/s40359-020-00464-8] [PMID]
- Salehi L, Rahimzadeh M, Molaei E, Zaheri H, Esmaelzadeh-Saeieh S. The relationship among fear and anxiety of COVID-19, pregnancy experience, and mental health disorder in pregnant women: A structural equation model. Brain Behav. 2020; 10(11):e01835. [DOI:10.1002/brb3.1835] [PMID]
- Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 Scale: Development and initial validation. Int J Ment Health Addict. 2020; 1-9. [DOI:10.1037/t78404-000]
- Alipour A, Ghadami A, Farsham A, Dorri N. A new self-reported assessment measure for COVID-19 Anxiety Scale (CDAS) in Iran: A web-based study. Iran J Public Health. 2020; 49(7):1316-23. [DOI:10.18502/ijph.v49i7.3585] [PMID]
- Naghizadeh S, Mirghafourvand M. Relationship of fear of COVID-19 and pregnancy-related quality of life during the COVID-19 pandemic. Arch Psychiatr Nurs. 2021; 35(4):364-8. [DOI:10.1016/j.apnu.2021.05.006] [PMID]
- Luo F, Ghanei Gheshlagh R, Dalvand S, Saedmoucheshi S, Li Q. Systematic review and meta-analysis of fear of COVID-19. Front Psychol. 2021; 12:661078. [DOI:10.3389/fpsyg.2021.661078] [PMID]
- Koiwa K, Wakashima K, Ikuta M, Asai K, Takagi G. Fear of COVID-19 infection and related factors in Japan: A comparison of college students, pregnant women, hospital nurses and the general public. PloS One. 2022; 17(7):e0271176. [DOI:10.1371/journal.pone.0271176] [PMID]
- Nausheen S, Bhamani S, Makhdoom A, Sheikh L. Fear of COVID-19 among pregnant women in Pakistan: A cross-sectional study. Int J Community Med Public Health. 2020; 7(12):4749. [DOI:10.18203/2394-6040.ijcmph20205145]
- Dunkel Schetter C, Niles AN, Guardino CM, Khaled M, Kramer MS. Demographic, medical, and psychosocial predictors of pregnancy anxiety. Paediatr Perinat Epidemiol. 2016; 30(5):421-9. [DOI:10.1111/ppe.12300] [PMID]
- Rezaee R, Framarzi M. Predictors of mental health during pregnancy. Iran J Nurs Midwifery Res. 2014; 19(7 Suppl 1):S45-50. [PMID]
- Steimer T. The biology of fear-and anxiety-related behaviors. Dialogues Clin Neurosci. 2002 ; 4(3):231-49. [PMID]
Type of Study: Research |
Subject:
Midwifery
Received: 2022/12/11 | Accepted: 2023/03/2 | Published: 2023/08/1
Received: 2022/12/11 | Accepted: 2023/03/2 | Published: 2023/08/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




