Sat, Dec 27, 2025
[Archive]
Volume 1, Issue 4 (Summer 2023)
CPR 2023, 1(4): 372-393 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Haji Mohammadreza M, Khani S, Shahhosseini Z, Pourasghar M. Psychological Interventions for the Quality of Life of Women With Polycystic Ovary Syndrome: A Scoping Review of Clinical Trials. CPR 2023; 1 (4) :372-393
URL: http://cpr.mazums.ac.ir/article-1-76-en.html
URL: http://cpr.mazums.ac.ir/article-1-76-en.html
Department of Midwifery and Reproductive Health, Mazandaran University of Medical Sciences, Sari, Iran.
Full-Text [PDF 3883 kb]
(721 Downloads)
| Abstract (HTML) (1632 Views)
Full-Text: (833 Views)
Introduction
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of reproductive age [1، 2]. Women with PCOS have a wide range of symptoms, including amenorrhea, oligomenorrhea, hirsutism, infertility, anovulation, weight gain or obesity, acne, androgenetic alopecia, and metabolic disorders [3، 4]. According to the Rotterdam criteria set by the European Society of Human Reproduction & Embryology and the American Society For Reproductive Medicine (ESHRE/ASRM), to diagnose PCOS after excluding other medical conditions leading to irregular menstrual cycle and hyperandrogenemia, at least two of the following three criteria should be met in the individual: oligomenorrhea or amenorrhea, hyperandrogenism, and the morphological appearance of polycystic ovaries (the presence of at least 12 or more small antral follicles in the ultrasound of the ovaries with a diameter between 2-9 mm or an increase in the size of the ovaries by more than 10 mm) [4-6].
According to the Rotterdam criteria, the global prevalence of PCOS is 5-10% [7] and its prevalence in Iran is relatively high (11.4%) [8]. The exact cause of PCOS is not clear, but the emergence of this syndrome is probably multifactorial and is caused by the interaction between genetic and environmental factors [8]. In reproductive age, the main complaint of patients is infertility and irregular ovulation [9]. This syndrome is the common cause of approximately 75% of infertility cases [10]. Patients with PCOS face an increased risk of uterine and ovarian cancer [11], late menopause [12], type 2 diabetes, high blood pressure, lipid disorders, cardiovascular disease [13، 14], depressed and anxious mood [15], Social phobia [16], eating disorders [17], suicide attempts [18] and bipolar disorder [19]. Studies show that the effects and complications left by PCOS cause psychological damage and a significant decrease in the quality of life (QOL) and health-related QOL in women with this syndrome compared to healthy women and even compared to those suffering from other diseases [20-24].
Factors affecting the QOL of women with PCOS in physical dimensions include overweight, hairiness, hair loss, acne lesions, menstrual disorders, and general health problems, and the factors in psychological, emotional, cognitive, and social dimensions include depression, despair, fear/anxiety, moodiness, introversion, low self-confidence, embarrassment/shame, impaired problem-solving and planning abilities, seclusion and isolationism, inability to express problems to those around, being blamed by the spouse for infertility, loss of femininity and the appearance of masculinity, disruption in marital relations, etc. [25، 26]. As a result, PCOS is a chronic disease that negatively affects both the physical and mental health of patients and their QOL [27]. This syndrome is not a disease specific to the reproductive age and adolescence. Due to its high prevalence, it can create a great health and economic burden on countries [28].
So far, different interventions have been developed to improve the QOL of women with PCOS [29-33], one of the most important of which is psychological interventions combined with medication therapy [34، 35]. Psychological interventions can change all aspects of life. Since women with PCOS are very prone to psychological disorders, psychological interventions can be useful [36-39]; however, to make a decision about their efficiency, a detailed investigation is needed. A scoping review study is used to critically evaluate and produce a conclusion for a particular question and to provide evidence. Unlike a systematic review, there is no need for complex statistical analyses such as meta-analysis in this type of review study. To our knowledge, a comprehensive review study has not been conducted in this field so far. A scoping review can be effective for systematic and interventional studies [40]. In this regard, and due to the great importance of QOL in women with PCOS, this scoping review study aimed to investigate psychological interventions for improving the QOL of women with PCOS.
Materials and Methods
This is a scoping review study, which was conducted in five stages according to the JBI approach. These steps are: 1- Identifying the research question, 2- Searching the related studies, 3- Selecting relevant studies, 4- Charting and summarizing the data, and 5- Reporting the results [40]. In the first step, the question was determined as: Are psychological interventions effective in improving the QOL of women with PCOS? The inclusion criteria were determined based on the PICO approach: Population (women with PCOS), Intervention (psychological interventions), Comparison (women with no psychological intervention), and Outcome (post-intervention QOL). For searching the related studies, the following keywords were used in Persian and English: “Psychological interventions”, “women”, “Quality of life”, and “polycystic ovary syndrome”. These keywords were used along the Boolean operators (AND, OR). The search was performed in Google Scholar, PubMed, EMBASE, Scopus, Cochrane Library, Science Direct, Web of Science, Scientific Information Database, IranDoc, IranMedex, and Magiran. All online articles published from 2010 to June 3, 2023 were searched. The reference list of identified articles was also manually searched to find more related studies. Searching was done independently by two researchers (first and second authors). The interventional studies (Quasi-experimental, experimental, and clinical trials), studies that investigated the effect of psychological interventions on the QOL of women with PCOS, those that met the PICO criteria, and those whose sample size and their results were clear were included in the study. The studies that did not meet the mentioned criteria and those with unavailable full texts were excluded.
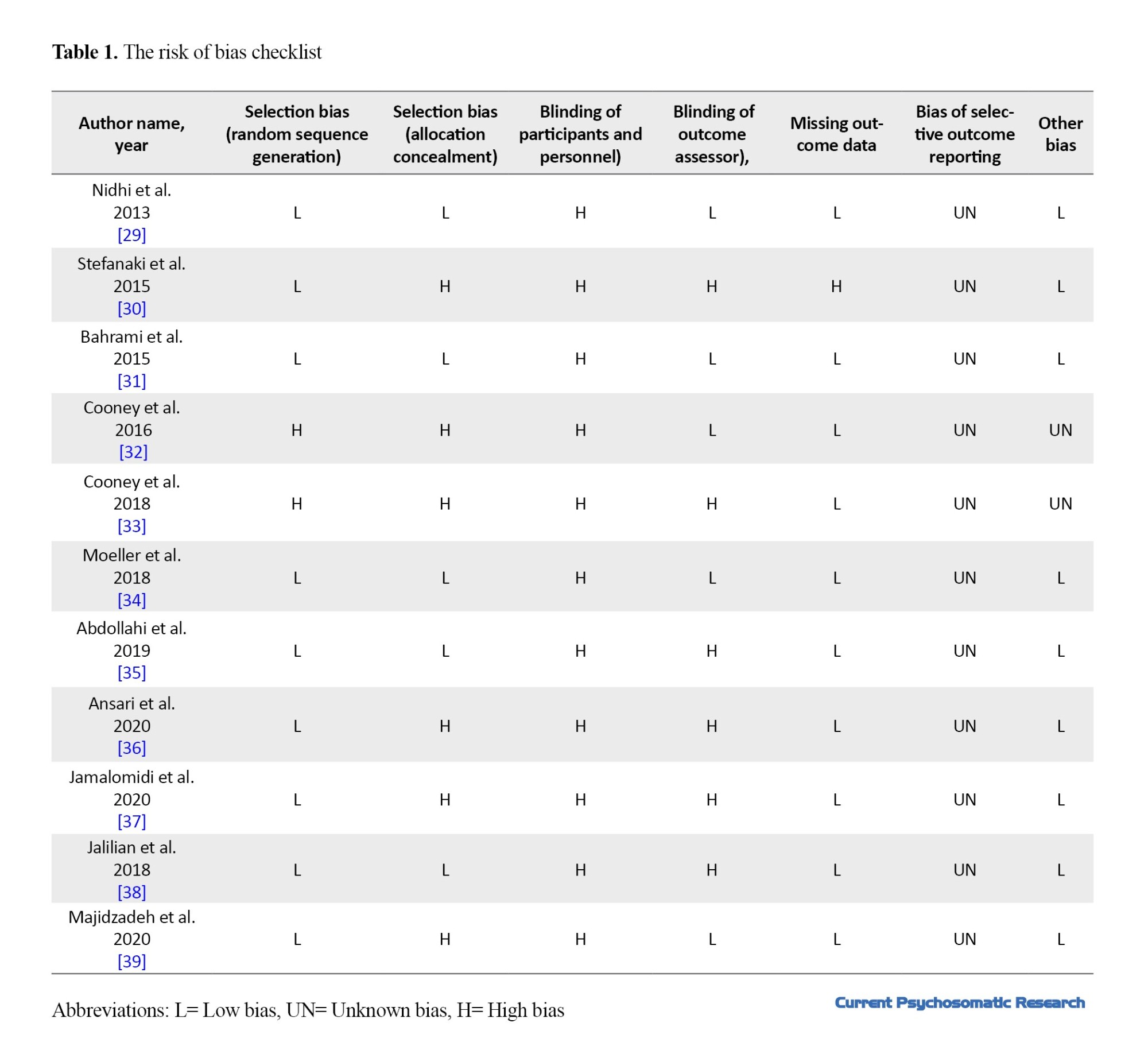
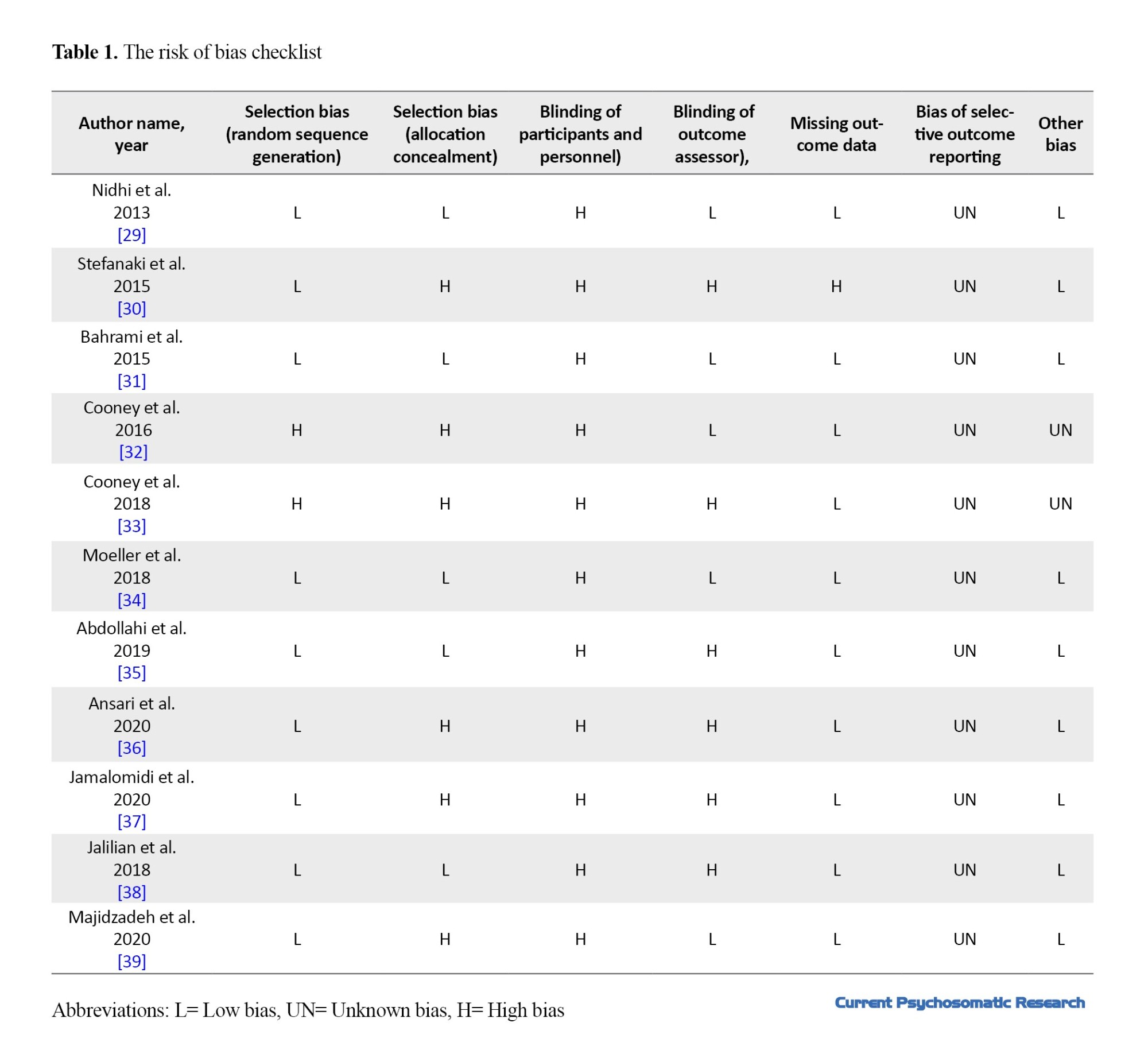
The quality of articles was examined in terms of selection bias (random sequence generation and allocation concealment), implementation bias (blinding of participants and personnel), diagnosis bias (blinding of outcome assessor), sample missing (missing data after randomization), bias of selective outcome reporting, and other bias. In this regard, we used the risk of bias checklist provided by Cochrane Library (Table 1) [17]. Based on this tool, the quality of the articles was classified into three levels: “High”, “Low,” and “Unclear”.
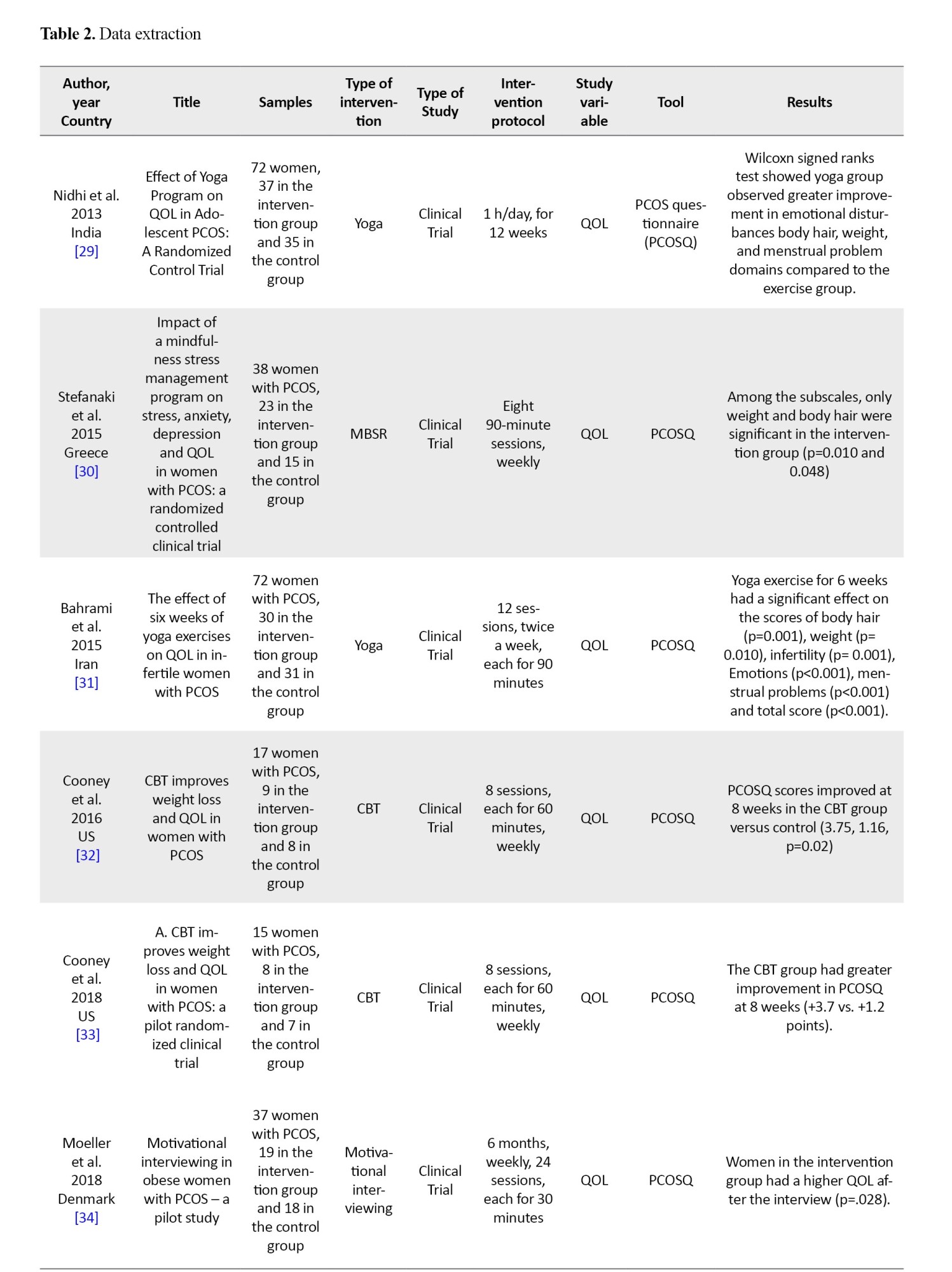
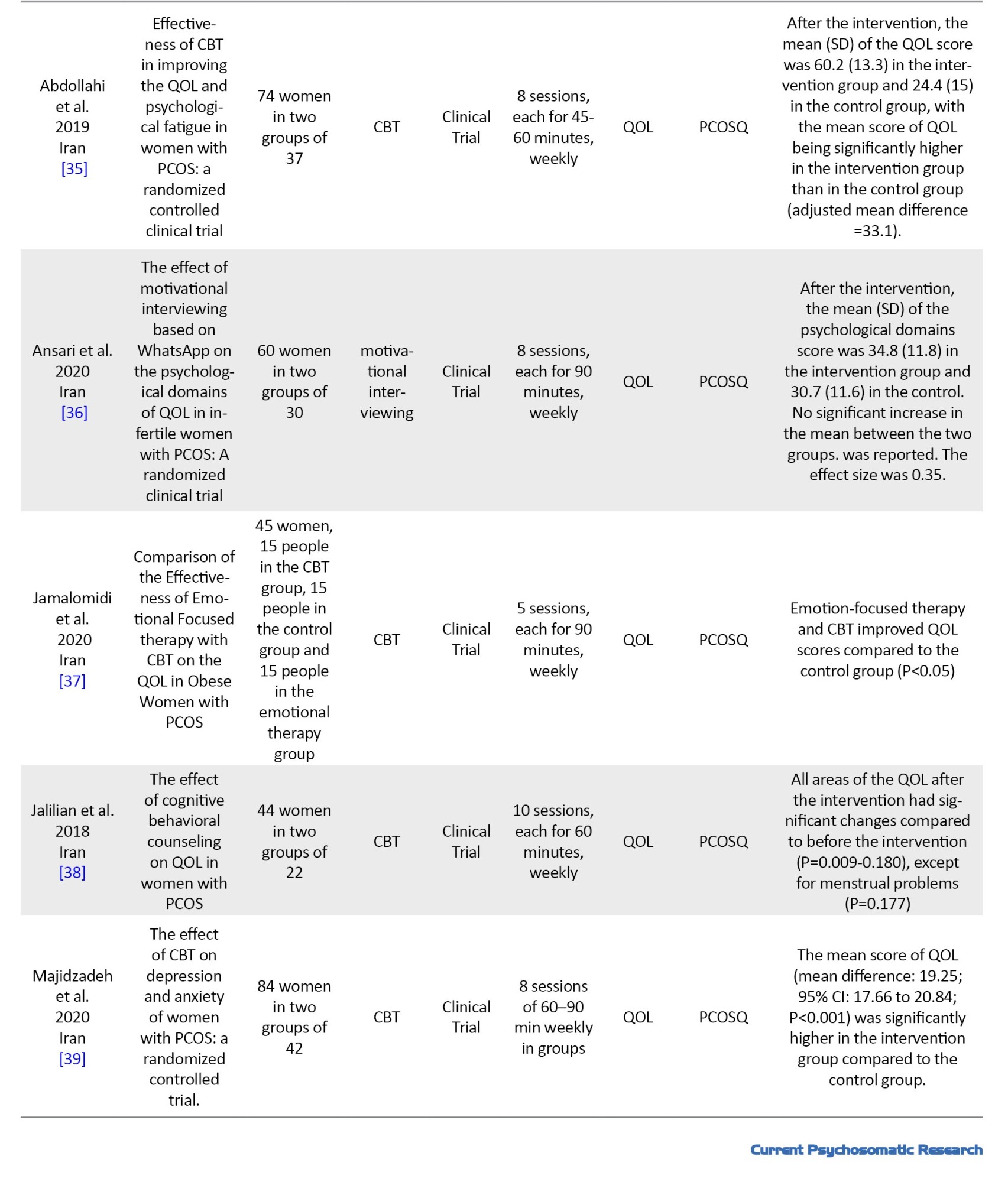
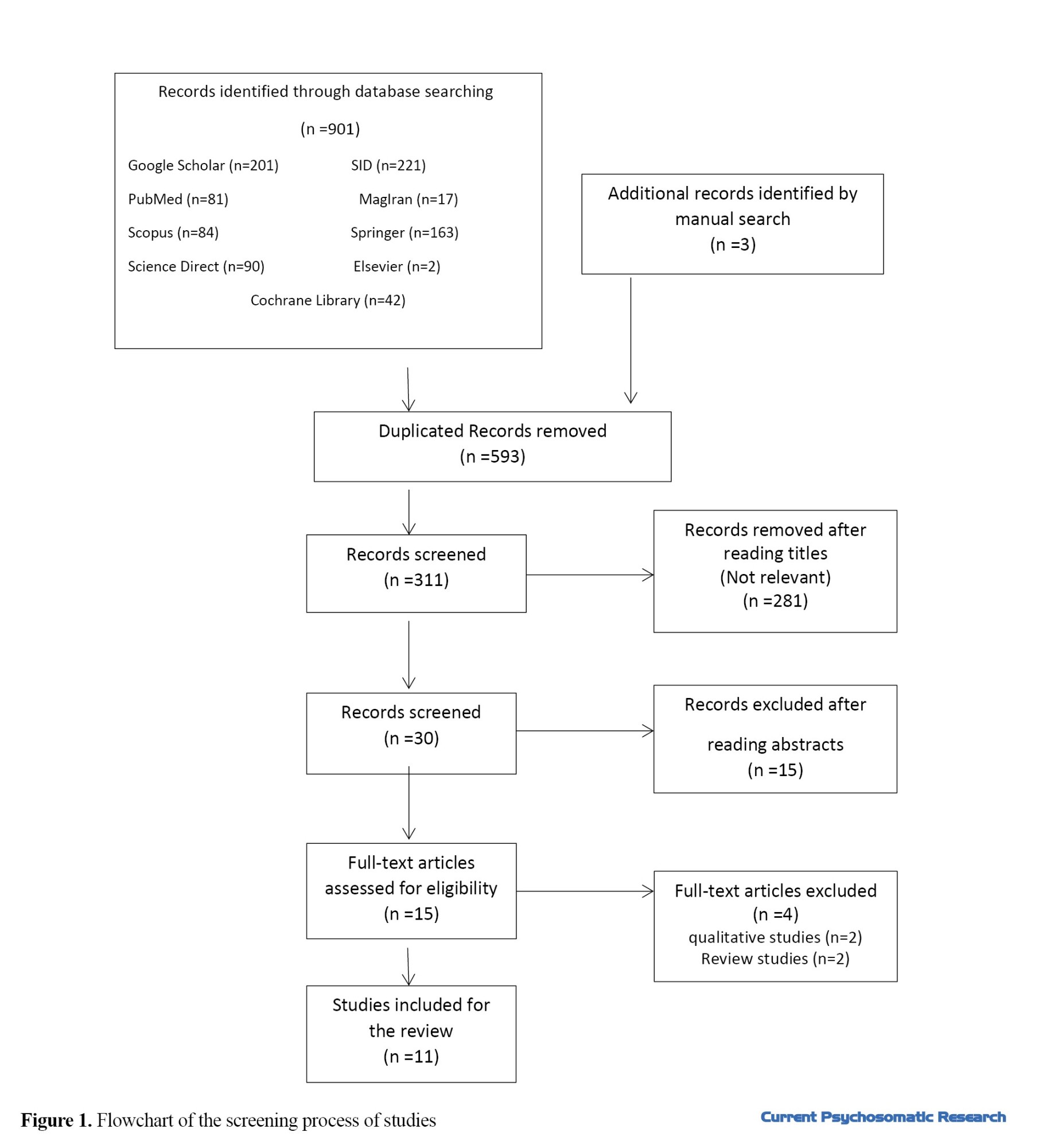
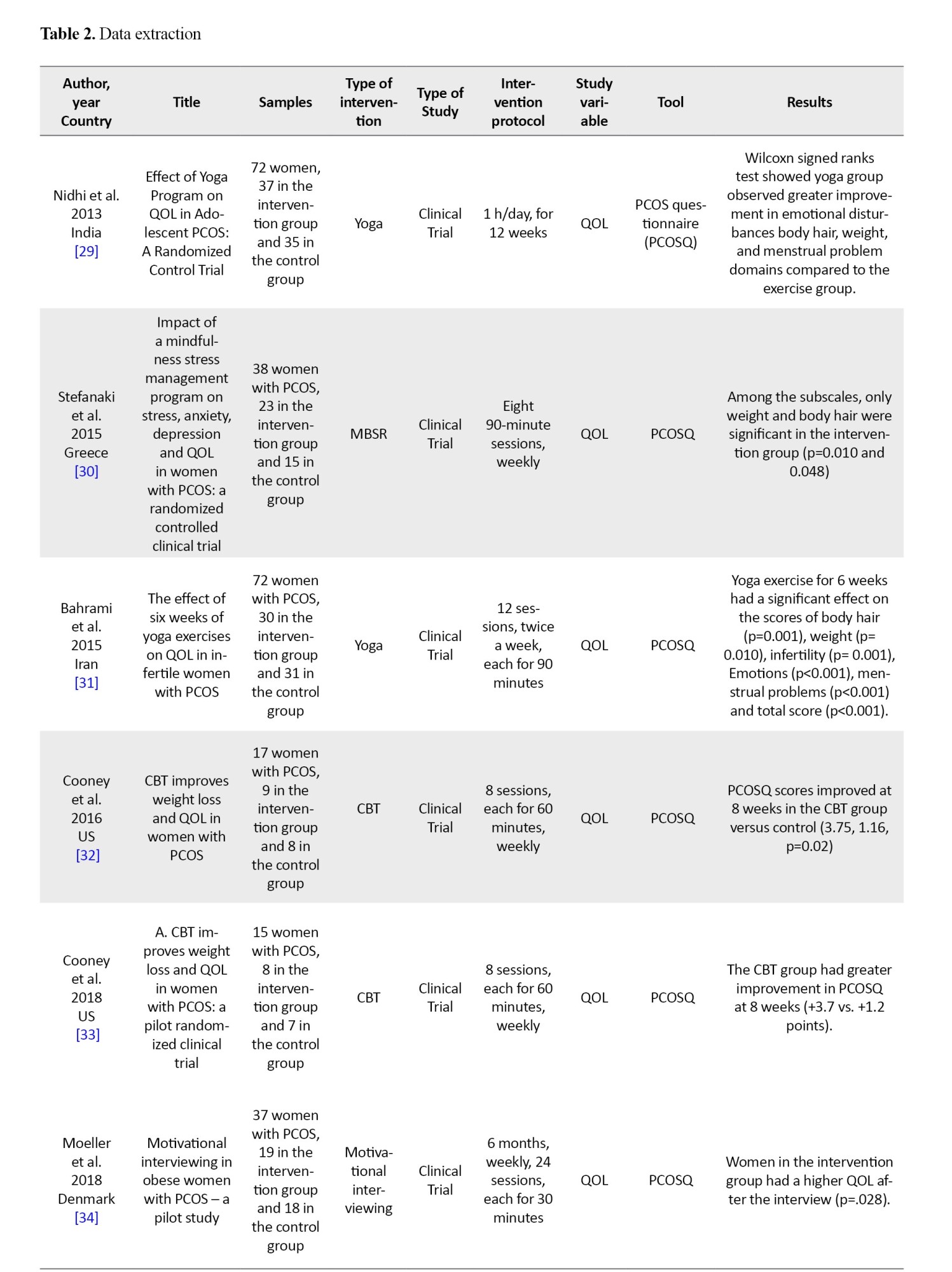
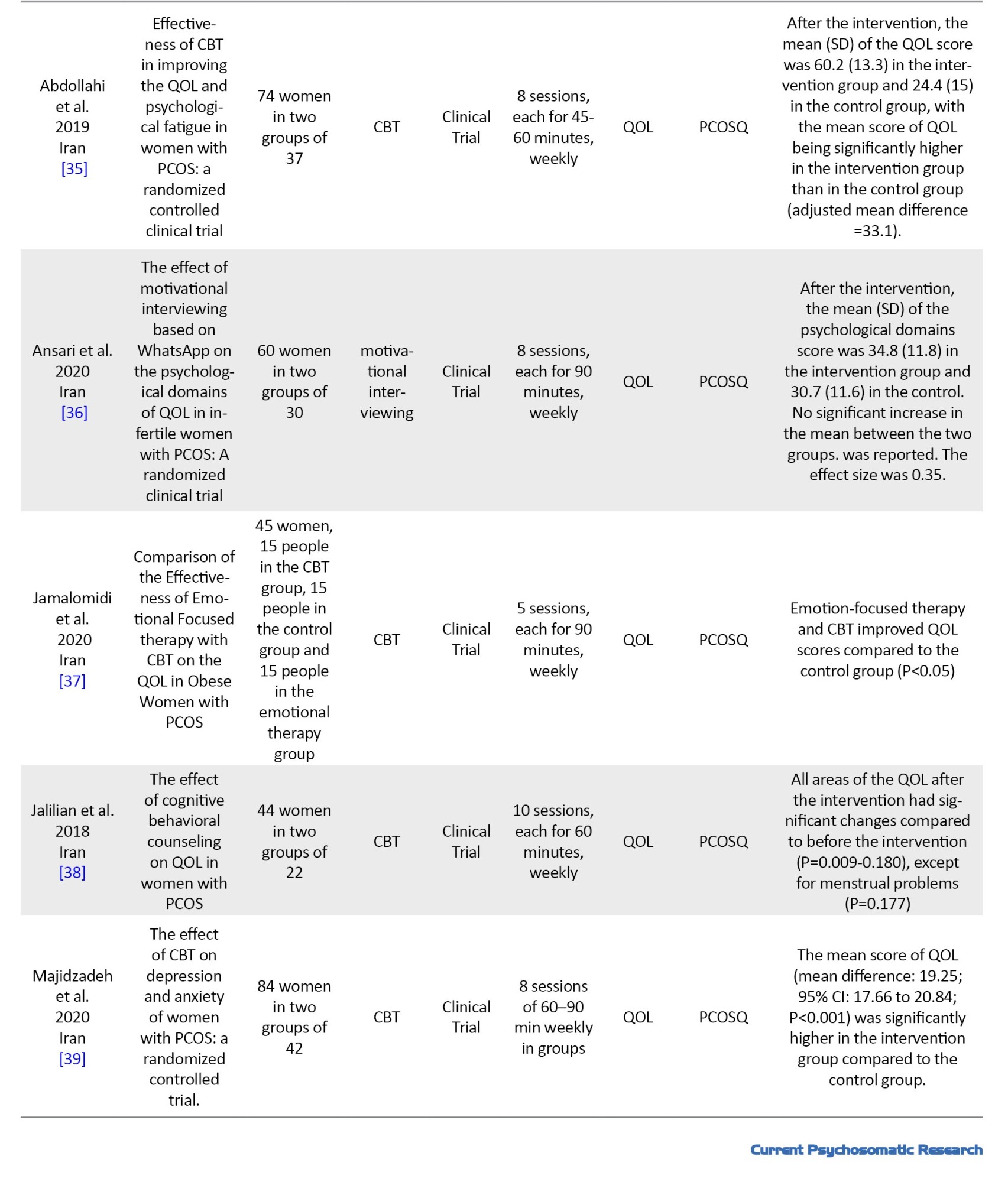
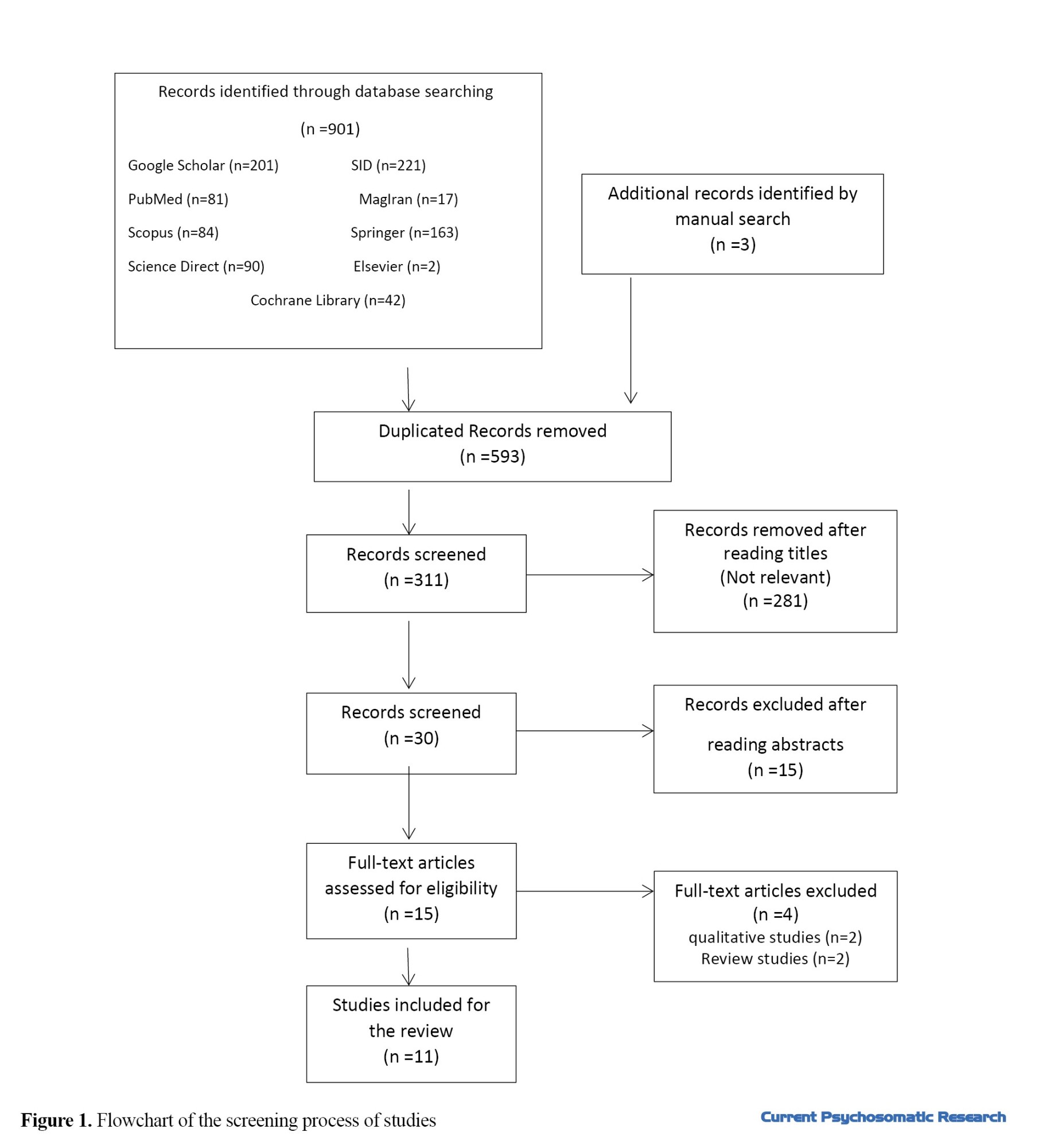
The initial search yielded 901 articles. Three articles were also found by manual search. After removing duplicates, unrelated articles were identified by reading titles and abstracts. After removing unrelated articles, 30 remained. Fifteen studies were removed after reading their abstracts, and 4 were removed after reading their full texts. Finally, 11 articles were selected for the review (Table 2), and their information, including the name of the authors, year of publication, study area, study purpose, sample size, tool, study variables, study design, and results were extracted (Figure.1).
Results
Participants
Participants in all studies were women of reproductive age. There was a total of 477 participants. Their age range was from 15 to 47 years. Participants included women with PCOS having morbid obesity, adolescent women, those in the premenopausal period, and those with infertility [29-37].
Data classification
Reviewing the texts of 11 articles, the findings were divided into four groups based on the intervention used: cognitive behavioral therapy (CBT), motivational interview, mindfulness, and yoga. Six studies used CBT [32، 33، 35، 37-39], two studies used motivational interviewing [34، 36], two studies used yoga [29، 31], and one study used mindfulness [30] to improve the QOL in women with PCOS.
CBT
Of six studies used CBT, two studies applied relaxation, breathing techniques, problem-solving techniques, cognitive restructuring, managing negative thoughts, psycho-education about PCOS and its symptoms, anger control and talking about sexual issues in CBT sessions. CBT sessions were conducted by one expert with PhD in clinical psychology and one expert master in psychology [32، 33]. Their result showed improvement in the intervention group in both studies. Another study by Abdulahi investigated the effect of CBT in patients with PCOS [35]. In the CBT sessions, problem-solving techniques, anger control, and stress management skills were taught. After the intervention, the mean score of QOL in the intervention group significantly increased [35]. Another study by Majidzadeh et al. investigated the effect of CBT on QOL, depression and anxiety of women with PCOS [39]. The contents of the sessions were based on overcoming incompatible thoughts and changing them, reducing the use of painkillers, anti-anxiety and anti-depressants, and increasing daily activity (exercise) as well as anger control and stress management [39].
Mindfulness therapy
One study investigated the effect of mindfulness intervention on the QOL of women with PCOS [30]. In this study, the effectiveness of Mindfulness-Based Stress Reduction (MBSR) therapy was evaluated in changing stress, anxiety, depression and QOL of women with PCOS. In the intervention sessions, mindfulness training, body scanning, breathing techniques, music and biofeedback support, group counseling and psycho-education (Psychological challenges, healthy habits including food and exercise, and mind-body interaction), stress and anxiety reduction, body image, and anger management were taught by a therapist expert in mindfulness therapy [30].
Yoga
In two studies used yoga [29، 31], the protocol included communication and interaction of participants with each other (30 minutes), muscle relaxation (10 minutes), yoga training with 5-10 breathing exercises (60 minutes), muscle relaxation with meditation and breathing techniques (10 minutes) and finally a question & answer session (10 minutes). Intervention sessions were conducted by a yoga instructor in both studies. The results of both studies showed satisfactory and effective role of yoga in improving the QOL of women with PCOS [29، 31].
Motivational interviewing
Two studies investigated the effect of motivational interviewing in improving the QOL of women with PCOS [34، 36]; one study conducted face-to-face [34] and one conducted virtually on WhatsApp [36]. Practicing and accurately identifying emotions, completing the impact of emotional dimensions, practicing brainstorming, the benefits of any short-term and long-term thinking, practicing completing the table of positive and negative dimensions, describing and practicing corrective and replacement options, defining values, defining the priority and importance of each person's values, defining a short-term and long-term plan, and discussing the prospects of these plans and their benefits were among the contents of motivational interviewing sessions. Both studies declared effective and satisfactory results.
Discussion
The current scoping review study evaluated 11 interventional studies that were conducted to investigate the effect of psychological interventions in improving the QOL of women with PCOS [29-37]. Six studies used CBT [32، 33، 35، 37-39], two studies used motivational interviewing [34، 36], two studies used yoga [29، 31], and one study used mindfulness [30] to improve the QOL of women with PCOS. All the studies reported the positive impact of psychological treatments in improving the QOL of women with PCOS and recommended their use along with another therapy (medication therapy, if necessary). The tool used in all 11 studies was PCOS questionnaire, which examines 5 domains (emotions, body hair, weight, infertility and menstrual problems).
In explaining the effectiveness of mindfulness therapy, it can be said that this therapy includes practicing the moment-by-moment awareness of thoughts, feelings and emotions in a non-judgmental manner [30]. This approach encourages women to consider distracting factors (such as negative and disturbing thoughts) as mental events, which are not necessarily accurate and true, and it is not necessary to believe in or pay attention to them [37]. There is evidence that the ability to include feelings in nonjudgmental words, which increases with mindfulness practice, is positively related to gray matter volume in the right anterior insula and right amygdala, indicating that the increase in this volume may reflect a person's greater awareness of the stressful situation and greater ability to cognitively manage emotions [42]. In the study that investigated the effect of mindfulness [30], two subscales of weight and body hair were significantly different after MBSR, but the other three subscales were not significant. To examine the impact on other dimensions, more use of mindfulness with a greater scope are needed, because the issues related to menstrual problems and infertility and emotions seem a little deeper [30].
In explaining the effectiveness of yoga on improving the QOL of women with PCOS, it can be said that this treatment has caused significant changes in all QOL aspects of women with PCOS (except infertility) by releasing negative thoughts and letting them go. In Nidhi et al.’s study, all areas were significant after yoga [29], but in Bahrami et al.'s study, all areas except infertility were declared significant [31]. This discrepancy can be attributed to the target population. In the first study, the samples were teenage women with PCOS [29], but in the second study, the samples were infertile women with PCOS [31]). The average scores after the intervention were also higher in Nidhi et al.’s study than in Bahrami et al.’s, which can also be due to the difference in the study samples. It seems that it is easier to intervene in adolescents without infertility. In cases with infertility, drug therapy is also needed. In other words, we cannot expect a statistically significant improvement in fertility simply by performing psychological methods.
In 2016 and 2018, Cooney et al. used CBT to improve the QOL of women with PCOS and reported its efficacy in all areas [32، 33]. They showed that CBT improved awareness, self-management, and mental state in women. In CBT, the therapist teaches the patient to answer stressful questions by using logical and current reasons [43]. Jalilian et al. showed significant changes in all areas of QOL after CBT compared to before the intervention, except for menstrual problems [38]. They recommended that CBT, along with drug therapy, can be very effective. Majidzadeh et al also confirmed the effectiveness of CBT in improving the QOL of women with PCOS [39]. Abdulahi et al. also reported that 8 sessions of CBT were effective in increasing the QOL score [35]. In Abdulahi et al.'s study, which was conducted on the age group of 18-35 years, CBT was more effective.
Another psychological treatment that was reported to have an impact on the QOL of women with PCOS was motivational interviewing. In two studies in Iran and Denmark in 2020 and 2018, motivational interviewing improved the QOL of women with PCOS [34، 36]. Ansari et al.'s study was conducted in Iran on infertile women with PCOS. Considering that infertility is one of the complications of PCOS, it may not necessarily occur in patients, but if occurs, it will certainly increase the psychological complications and effects on different aspects of life [44]. Thus, psychological interventions may be less effective for infertile women. However, Ansari et al. reported that the QOL of infertile women improved significantly after motivational interviewing [36]. In the study by Moeller et al., improvement in QOL after motivational interviewing was also reported [34]. However, in Moeller et al.’s [34] study, the effectiveness rate was higher, because the intervention was conducted face-to-face and weekly for 6 months, while in Ansari et al.'s study, the intervention was online at 5 sessions. Motivational interviewing provides a vision of the benefit of psychological changes in the long term by motivating patients, which can cause changes for recovery [45].
Conclusion
CBT, mindfulness therapy, motivational interviewing, and yoga training can be effective in improving the QOL of women with PCOS. However, there is scant research in this field. To access stronger evidence for the efficacy of psychological interventions in improving the QOL in PCOS women, more studies with less bias are needed.
Ethical Considerations
Compliance with ethical guidelines
This article is the result of a review study and did not have any human or animal samples. Ethical issues such as avoiding plagiarism, ensuring robustness in collecting relevant data, and publishing rights were considered.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Initial draft preparation, data collection, search and investigation: Mahtab Haji Mohammadreza and Soghra Khani; Writing original draft: Mahtab Haji Mohammadreza , Soghra Khani and Zohre Shahhosseini; Editing and final approval: All authors.
Conflict of interest
The authors contributed equally to preparing this paper.
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of reproductive age [1، 2]. Women with PCOS have a wide range of symptoms, including amenorrhea, oligomenorrhea, hirsutism, infertility, anovulation, weight gain or obesity, acne, androgenetic alopecia, and metabolic disorders [3، 4]. According to the Rotterdam criteria set by the European Society of Human Reproduction & Embryology and the American Society For Reproductive Medicine (ESHRE/ASRM), to diagnose PCOS after excluding other medical conditions leading to irregular menstrual cycle and hyperandrogenemia, at least two of the following three criteria should be met in the individual: oligomenorrhea or amenorrhea, hyperandrogenism, and the morphological appearance of polycystic ovaries (the presence of at least 12 or more small antral follicles in the ultrasound of the ovaries with a diameter between 2-9 mm or an increase in the size of the ovaries by more than 10 mm) [4-6].
According to the Rotterdam criteria, the global prevalence of PCOS is 5-10% [7] and its prevalence in Iran is relatively high (11.4%) [8]. The exact cause of PCOS is not clear, but the emergence of this syndrome is probably multifactorial and is caused by the interaction between genetic and environmental factors [8]. In reproductive age, the main complaint of patients is infertility and irregular ovulation [9]. This syndrome is the common cause of approximately 75% of infertility cases [10]. Patients with PCOS face an increased risk of uterine and ovarian cancer [11], late menopause [12], type 2 diabetes, high blood pressure, lipid disorders, cardiovascular disease [13، 14], depressed and anxious mood [15], Social phobia [16], eating disorders [17], suicide attempts [18] and bipolar disorder [19]. Studies show that the effects and complications left by PCOS cause psychological damage and a significant decrease in the quality of life (QOL) and health-related QOL in women with this syndrome compared to healthy women and even compared to those suffering from other diseases [20-24].
Factors affecting the QOL of women with PCOS in physical dimensions include overweight, hairiness, hair loss, acne lesions, menstrual disorders, and general health problems, and the factors in psychological, emotional, cognitive, and social dimensions include depression, despair, fear/anxiety, moodiness, introversion, low self-confidence, embarrassment/shame, impaired problem-solving and planning abilities, seclusion and isolationism, inability to express problems to those around, being blamed by the spouse for infertility, loss of femininity and the appearance of masculinity, disruption in marital relations, etc. [25، 26]. As a result, PCOS is a chronic disease that negatively affects both the physical and mental health of patients and their QOL [27]. This syndrome is not a disease specific to the reproductive age and adolescence. Due to its high prevalence, it can create a great health and economic burden on countries [28].
So far, different interventions have been developed to improve the QOL of women with PCOS [29-33], one of the most important of which is psychological interventions combined with medication therapy [34، 35]. Psychological interventions can change all aspects of life. Since women with PCOS are very prone to psychological disorders, psychological interventions can be useful [36-39]; however, to make a decision about their efficiency, a detailed investigation is needed. A scoping review study is used to critically evaluate and produce a conclusion for a particular question and to provide evidence. Unlike a systematic review, there is no need for complex statistical analyses such as meta-analysis in this type of review study. To our knowledge, a comprehensive review study has not been conducted in this field so far. A scoping review can be effective for systematic and interventional studies [40]. In this regard, and due to the great importance of QOL in women with PCOS, this scoping review study aimed to investigate psychological interventions for improving the QOL of women with PCOS.
Materials and Methods
This is a scoping review study, which was conducted in five stages according to the JBI approach. These steps are: 1- Identifying the research question, 2- Searching the related studies, 3- Selecting relevant studies, 4- Charting and summarizing the data, and 5- Reporting the results [40]. In the first step, the question was determined as: Are psychological interventions effective in improving the QOL of women with PCOS? The inclusion criteria were determined based on the PICO approach: Population (women with PCOS), Intervention (psychological interventions), Comparison (women with no psychological intervention), and Outcome (post-intervention QOL). For searching the related studies, the following keywords were used in Persian and English: “Psychological interventions”, “women”, “Quality of life”, and “polycystic ovary syndrome”. These keywords were used along the Boolean operators (AND, OR). The search was performed in Google Scholar, PubMed, EMBASE, Scopus, Cochrane Library, Science Direct, Web of Science, Scientific Information Database, IranDoc, IranMedex, and Magiran. All online articles published from 2010 to June 3, 2023 were searched. The reference list of identified articles was also manually searched to find more related studies. Searching was done independently by two researchers (first and second authors). The interventional studies (Quasi-experimental, experimental, and clinical trials), studies that investigated the effect of psychological interventions on the QOL of women with PCOS, those that met the PICO criteria, and those whose sample size and their results were clear were included in the study. The studies that did not meet the mentioned criteria and those with unavailable full texts were excluded.
The quality of articles was examined in terms of selection bias (random sequence generation and allocation concealment), implementation bias (blinding of participants and personnel), diagnosis bias (blinding of outcome assessor), sample missing (missing data after randomization), bias of selective outcome reporting, and other bias. In this regard, we used the risk of bias checklist provided by Cochrane Library (Table 1) [17]. Based on this tool, the quality of the articles was classified into three levels: “High”, “Low,” and “Unclear”.
The initial search yielded 901 articles. Three articles were also found by manual search. After removing duplicates, unrelated articles were identified by reading titles and abstracts. After removing unrelated articles, 30 remained. Fifteen studies were removed after reading their abstracts, and 4 were removed after reading their full texts. Finally, 11 articles were selected for the review (Table 2), and their information, including the name of the authors, year of publication, study area, study purpose, sample size, tool, study variables, study design, and results were extracted (Figure.1).
Results
Participants
Participants in all studies were women of reproductive age. There was a total of 477 participants. Their age range was from 15 to 47 years. Participants included women with PCOS having morbid obesity, adolescent women, those in the premenopausal period, and those with infertility [29-37].
Data classification
Reviewing the texts of 11 articles, the findings were divided into four groups based on the intervention used: cognitive behavioral therapy (CBT), motivational interview, mindfulness, and yoga. Six studies used CBT [32، 33، 35، 37-39], two studies used motivational interviewing [34، 36], two studies used yoga [29، 31], and one study used mindfulness [30] to improve the QOL in women with PCOS.
CBT
Of six studies used CBT, two studies applied relaxation, breathing techniques, problem-solving techniques, cognitive restructuring, managing negative thoughts, psycho-education about PCOS and its symptoms, anger control and talking about sexual issues in CBT sessions. CBT sessions were conducted by one expert with PhD in clinical psychology and one expert master in psychology [32، 33]. Their result showed improvement in the intervention group in both studies. Another study by Abdulahi investigated the effect of CBT in patients with PCOS [35]. In the CBT sessions, problem-solving techniques, anger control, and stress management skills were taught. After the intervention, the mean score of QOL in the intervention group significantly increased [35]. Another study by Majidzadeh et al. investigated the effect of CBT on QOL, depression and anxiety of women with PCOS [39]. The contents of the sessions were based on overcoming incompatible thoughts and changing them, reducing the use of painkillers, anti-anxiety and anti-depressants, and increasing daily activity (exercise) as well as anger control and stress management [39].
Mindfulness therapy
One study investigated the effect of mindfulness intervention on the QOL of women with PCOS [30]. In this study, the effectiveness of Mindfulness-Based Stress Reduction (MBSR) therapy was evaluated in changing stress, anxiety, depression and QOL of women with PCOS. In the intervention sessions, mindfulness training, body scanning, breathing techniques, music and biofeedback support, group counseling and psycho-education (Psychological challenges, healthy habits including food and exercise, and mind-body interaction), stress and anxiety reduction, body image, and anger management were taught by a therapist expert in mindfulness therapy [30].
Yoga
In two studies used yoga [29، 31], the protocol included communication and interaction of participants with each other (30 minutes), muscle relaxation (10 minutes), yoga training with 5-10 breathing exercises (60 minutes), muscle relaxation with meditation and breathing techniques (10 minutes) and finally a question & answer session (10 minutes). Intervention sessions were conducted by a yoga instructor in both studies. The results of both studies showed satisfactory and effective role of yoga in improving the QOL of women with PCOS [29، 31].
Motivational interviewing
Two studies investigated the effect of motivational interviewing in improving the QOL of women with PCOS [34، 36]; one study conducted face-to-face [34] and one conducted virtually on WhatsApp [36]. Practicing and accurately identifying emotions, completing the impact of emotional dimensions, practicing brainstorming, the benefits of any short-term and long-term thinking, practicing completing the table of positive and negative dimensions, describing and practicing corrective and replacement options, defining values, defining the priority and importance of each person's values, defining a short-term and long-term plan, and discussing the prospects of these plans and their benefits were among the contents of motivational interviewing sessions. Both studies declared effective and satisfactory results.
Discussion
The current scoping review study evaluated 11 interventional studies that were conducted to investigate the effect of psychological interventions in improving the QOL of women with PCOS [29-37]. Six studies used CBT [32، 33، 35، 37-39], two studies used motivational interviewing [34، 36], two studies used yoga [29، 31], and one study used mindfulness [30] to improve the QOL of women with PCOS. All the studies reported the positive impact of psychological treatments in improving the QOL of women with PCOS and recommended their use along with another therapy (medication therapy, if necessary). The tool used in all 11 studies was PCOS questionnaire, which examines 5 domains (emotions, body hair, weight, infertility and menstrual problems).
In explaining the effectiveness of mindfulness therapy, it can be said that this therapy includes practicing the moment-by-moment awareness of thoughts, feelings and emotions in a non-judgmental manner [30]. This approach encourages women to consider distracting factors (such as negative and disturbing thoughts) as mental events, which are not necessarily accurate and true, and it is not necessary to believe in or pay attention to them [37]. There is evidence that the ability to include feelings in nonjudgmental words, which increases with mindfulness practice, is positively related to gray matter volume in the right anterior insula and right amygdala, indicating that the increase in this volume may reflect a person's greater awareness of the stressful situation and greater ability to cognitively manage emotions [42]. In the study that investigated the effect of mindfulness [30], two subscales of weight and body hair were significantly different after MBSR, but the other three subscales were not significant. To examine the impact on other dimensions, more use of mindfulness with a greater scope are needed, because the issues related to menstrual problems and infertility and emotions seem a little deeper [30].
In explaining the effectiveness of yoga on improving the QOL of women with PCOS, it can be said that this treatment has caused significant changes in all QOL aspects of women with PCOS (except infertility) by releasing negative thoughts and letting them go. In Nidhi et al.’s study, all areas were significant after yoga [29], but in Bahrami et al.'s study, all areas except infertility were declared significant [31]. This discrepancy can be attributed to the target population. In the first study, the samples were teenage women with PCOS [29], but in the second study, the samples were infertile women with PCOS [31]). The average scores after the intervention were also higher in Nidhi et al.’s study than in Bahrami et al.’s, which can also be due to the difference in the study samples. It seems that it is easier to intervene in adolescents without infertility. In cases with infertility, drug therapy is also needed. In other words, we cannot expect a statistically significant improvement in fertility simply by performing psychological methods.
In 2016 and 2018, Cooney et al. used CBT to improve the QOL of women with PCOS and reported its efficacy in all areas [32، 33]. They showed that CBT improved awareness, self-management, and mental state in women. In CBT, the therapist teaches the patient to answer stressful questions by using logical and current reasons [43]. Jalilian et al. showed significant changes in all areas of QOL after CBT compared to before the intervention, except for menstrual problems [38]. They recommended that CBT, along with drug therapy, can be very effective. Majidzadeh et al also confirmed the effectiveness of CBT in improving the QOL of women with PCOS [39]. Abdulahi et al. also reported that 8 sessions of CBT were effective in increasing the QOL score [35]. In Abdulahi et al.'s study, which was conducted on the age group of 18-35 years, CBT was more effective.
Another psychological treatment that was reported to have an impact on the QOL of women with PCOS was motivational interviewing. In two studies in Iran and Denmark in 2020 and 2018, motivational interviewing improved the QOL of women with PCOS [34، 36]. Ansari et al.'s study was conducted in Iran on infertile women with PCOS. Considering that infertility is one of the complications of PCOS, it may not necessarily occur in patients, but if occurs, it will certainly increase the psychological complications and effects on different aspects of life [44]. Thus, psychological interventions may be less effective for infertile women. However, Ansari et al. reported that the QOL of infertile women improved significantly after motivational interviewing [36]. In the study by Moeller et al., improvement in QOL after motivational interviewing was also reported [34]. However, in Moeller et al.’s [34] study, the effectiveness rate was higher, because the intervention was conducted face-to-face and weekly for 6 months, while in Ansari et al.'s study, the intervention was online at 5 sessions. Motivational interviewing provides a vision of the benefit of psychological changes in the long term by motivating patients, which can cause changes for recovery [45].
Conclusion
CBT, mindfulness therapy, motivational interviewing, and yoga training can be effective in improving the QOL of women with PCOS. However, there is scant research in this field. To access stronger evidence for the efficacy of psychological interventions in improving the QOL in PCOS women, more studies with less bias are needed.
Ethical Considerations
Compliance with ethical guidelines
This article is the result of a review study and did not have any human or animal samples. Ethical issues such as avoiding plagiarism, ensuring robustness in collecting relevant data, and publishing rights were considered.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Initial draft preparation, data collection, search and investigation: Mahtab Haji Mohammadreza and Soghra Khani; Writing original draft: Mahtab Haji Mohammadreza , Soghra Khani and Zohre Shahhosseini; Editing and final approval: All authors.
Conflict of interest
The authors contributed equally to preparing this paper.
References
- Kaczmarek C, Haller DM, Yaron M. Health-related quality of life in adolescents and young adults with polycystic ovary syndrome: A systematic review. J Pediatr Adolesc Gynecol. 2016; 29(6):551-7. [DOI:10.1016/j.jpag.2016.05.006] [PMID]
- Tsikouras P, Spyros L, Manav B, Zervoudis S, Poiana C, Nikolaos T, et al. Features of polycystic ovary syndrome in adolescence. J Med Life. 2015; 8(3):291-6. [PMID] [PMCID]
- Malik-Aslam A, Reaney MD, Speight J. The suitability of polycystic ovary syndrome-specific questionnaires for measuring the impact of PCOS on quality of life in clinical trials. Value Health. 2010; 13(4):440-6. [DOI:10.1111/j.1524-4733.2010.00696.x] [PMID]
- Daniilidis A, Dinas K. Long term health consequences of polycystic ovarian syndrome: A review analysis. Hippokratia. 2009; 13(2):90-2. [PMID] [PMCID]
- Haoula Z, Salman M, Atiomo W. Evaluating the association between endometrial cancer and polycystic ovary syndrome. Hum Reprod. 2012; 27(5):1327-31. [DOI:10.1093/humrep/des042] [PMID]
- Dunaif A,Chang RJ, Franks S, Legro RS. Polycystic ovary syndrome: Current controversies, from the ovary to the pancreas. Berlin: Springer Science & Business Media; 2008. [DOI:10.1007/978-1-59745-108-6]
- Tehrani FR, Simbar M, Tohidi M, Hosseinpanah F, Azizi F. The prevalence of polycystic ovary syndrome in a community sample of Iranian population: Iranian PCOS prevalence study. Reprod Biol Endocrinol. 2011; 9:39. [DOI:10.1186/1477-7827-9-39] [PMID] [PMCID]
- Lizneva D, Suturina L, Walker W, Brakta S, Gavrilova-Jordan L, Azziz R. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil Steril. 2016; 106(1):6-15. [DOI:10.1016/j.fertnstert.2016.05.003] [PMID]
- Jalilian A, Kiani F, Sayehmiri F, Sayehmiri K, Khodaee Z, Akbari M. Prevalence of polycystic ovary syndrome and its associated complications in Iranian women: A meta-analysis. Iran J Reprod Med. 2015; 13(10):591-604. [PMID] [PMCID]
- Toscani MK, Mario FM, Radavelli-Bagatini S, Spritzer PM. Insulin resistance is not strictly associated with energy intake or dietary macronutrient composition in women with polycystic ovary syndrome. Nutr Res. 2011; 31(2):97-103. [DOI:10.1016/j.nutres.2011.01.009] [PMID]
- Harris HR, Terry KL. Polycystic ovary syndrome and risk of endometrial, ovarian, and breast cancer: A systematic review. Fertil Res Pract. 2016; 2:14. [DOI:10.1186/s40738-016-0029-2] [PMID] [PMCID]
- Forslund M, Landin-Wilhelmsen K, Schmidt J, Brännström M, Trimpou P, Dahlgren E. Higher menopausal age but no differences in parity in women with polycystic ovary syndrome compared with controls. Acta Obstet Gynecol Scand. 2019; 98(3):320-6. [DOI:10.1111/aogs.13489] [PMID] [PMCID]
- Brehm A, Pfeiler G, Pacini G, Vierhapper H, Roden M. Relationship between serum lipoprotein ratios and insulin resistance in obesity. Clin Chem. 2004; 50(12):2316-22. [DOI:10.1373/clinchem.2004.037556] [PMID]
- Xiang SK, Hua F, Tang Y, Jiang XH, Zhuang Q, Qian FJ. Relationship between serum lipoprotein ratios and insulin resistance in polycystic ovary syndrome. Int J Endocrinol. 2012; 2012:173281. [DOI:10.1155/2012/173281] [PMID] [PMCID]
- Mehrabadi S, Jahanian Sadatmahalleh S, Kazemnejad A. [Association of depression and anxiety with cognitive function in patients with polycystic ovary syndrome (Persian)]. J Mazandaran Univ Med Sci. 2017; 27(147):159-70. [Link]
- Benson S, Hahn S, Tan S, Mann K, Janssen OE, Schedlowski M, et al. Prevalence and implications of anxiety in polycystic ovary syndrome: Results of an internet-based survey in Germany. Hum Reprod. 2009; 24(6):1446-51. [DOI:10.1093/humrep/dep031] [PMID]
- Kerchner A, Lester W, Stuart SP, Dokras A. Risk of depression and other mental health disorders in women with polycystic ovary syndrome: A longitudinal study. Fertil Steril. 2009; 91(1):207-12. [DOI:10.1016/j.fertnstert.2007.11.022] [PMID]
- Månsson M, Holte J, Landin-Wilhelmsen K, Dahlgren E, Johansson A, Landén M. Women with polycystic ovary syndrome are often depressed or anxious--A case control study. Psychoneuroendocrinology. 2008; 33(8):1132-8. [DOI:10.1016/j.psyneuen.2008.06.003] [PMID]
- Chen SF, Yang YC, Hsu CY, Shen YC. Risk of bipolar disorder in patients with polycystic ovary syndrome: A nationwide population-based cohort study. J Affect Disord. 2020 263:458-62. [DOI:10.1016/j.jad.2019.12.007] [PMID]
- Hasan M, Sultana S, Sohan M, Parvin S, Rahman MA, Hossain MJ, et al. Prevalence and associated risk factors for mental health problems among patients with polycystic ovary syndrome in Bangladesh: A nationwide cross-Sectional study. Plos One. 2022; 17(6):e0270102. [DOI:10.1371/journal.pone.0270102] [PMID] [PMCID]
- Barberis N, Calaresi D, Cannavò M, Verrastro V. Trait emotional intelligence and quality of life in women with polycystic ovary syndrome: Dysmorphic concerns and general distress as mediators. Compr Psychiatry. 2023; 122:152373. [DOI:10.1016/j.comppsych.2023.152373] [PMID]
- Van Niekerk LM, Bromfield H, Matthewson M. Physical and psychological correlates of self and body compassion in women with polycystic ovary syndrome. J Health Psychol. 2022; 27(11):2566-80. [DOI:10.1177/13591053211059390] [PMID]
- Pokora K, Kowalczyk K, Wikarek A, Rodak M, Pędrys K, Wójtowicz M, et al. Depressive symptoms and control of emotions among polish women with polycystic ovary syndrome. Int J Environ Res Public Health. 2022; 19(24):16871. [DOI:10.3390/ijerph192416871] [PMID] [PMCID]
- Douglas KM, Fenton AJ, Eggleston K, Porter RJ. Rate of polycystic ovary syndrome in mental health disorders: A systematic review. Arch Womens Ment Health. 2022; 25(1):9-19. [DOI:10.1007/s00737-021-01179-4] [PMID]
- Jegargoosheh S, Mostafazadeh F, Fathibitaraf S, Akhavanakbari P. [Evaluation of quality of life of women with polycystic ovary syndrome referred to Ardabil Alavi Educational and Medical Center, 2021 (Persian)]. J Health Care. 2021; 23(3):271-9. [DOI:10.52547/jhc.23.3.271]
- Pakari N, Chananeh M. Investigating the quality of life of women with polycystic ovary syndrome: A review study. Paper presented at: 8th Congress of Reproductive Health and Infertility Research Center. 16 December 2015; Tehran, Iran. [Link]
- Chaudhari AP, Mazumdar K, Mehta PD. Anxiety, depression, and quality of life in women with polycystic ovarian syndrome. Indian J Psychol Med. 2018; 40(3):239-46. [PMID]
- Dema H, Videtič Paska A, Kouter K, Katrašnik M, Jensterle M, Janež A, et al. Effects of mindfulness-based therapy on clinical symptoms and DNA methylation in patients with polycystic ovary syndrome and high metabolic risk. Curr Issues Mol Biol. 2023; 45(4):2717-37. [DOI:10.3390/cimb45040178] [PMID] [PMCID]
- Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. Effect of yoga program on quality of life in adolescent polycystic ovarian syndrome: A randomized control trial. Appl Res Life. 2013; 8:373-83. [DOI:10.1007/s11482-012-9191-9]
- Stefanaki C, Bacopoulou F, Livadas S, Kandaraki A, Karachalios A, Chrousos GP, et al. Impact of a mindfulness stress management program on stress, anxiety, depression and quality of life in women with polycystic ovary syndrome: A randomized controlled trial. Stress. 2015; 18(1):57-66. [DOI:10.3109/10253890.2014.974030] [PMID]
- Bahrami H, Mohseni M, Amini L, Karimian Z. [The effect of six weeks yoga exercises on quality of life in infertile women with polycystic ovary syndrome (PCOS) (Persian)]. Iran J Obstet Gynecol Infertil. 2019; 22(5):18-26. [DOI:10.22038/ijogi.2019.13578]
- Cooney L, Milman LW, Sammel M, Allison K, Epperson C, Dokras A. Cognitive behavioral therapy improves weight loss and quality of life in women with polycystic ovary syndrome (PCOS). Fertil Steril. 2016; 106(3):E252-3. [DOI:10.1016/j.fertnstert.2016.07.729]
- Cooney LG, Milman LW, Hantsoo L, Kornfield S, Sammel MD, Allison KC, et al. Cognitive-behavioral therapy improves weight loss and quality of life in women with polycystic ovary syndrome: A pilot randomized clinical trial. Fertil Steril. 2018; 110(1):161-71.e1. [DOI:10.1016/j.fertnstert.2018.03.028] [PMID] [PMCID]
- Moeller LV, Lindhardt CL, Andersen MS, Glintborg D, Ravn P. Motivational interviewing in obese women with polycystic ovary syndrome - A pilot study. Gynecol Endocrinol. 2019; 35(1):76-80. [DOI:10.1080/09513590.2018.1498832] [PMID]
- Abdollahi L, Mirghafourvand M, Babapour JK, Mohammadi M. Effectiveness of cognitive-behavioral therapy (CBT) in improving the quality of life and psychological fatigue in women with polycystic ovarian syndrome: A randomized controlled clinical trial. J Psychosom Obstet Gynaecol. 2019; 40(4):283-93. [DOI:10.1080/0167482X.2018.1502265] [PMID]
- Ansari F, Hamzehgardeshi Z, Elyasi F, Moosazadeh M, Ahmadi I. The effect of motivational interview based on WhatsApp on the psychological domains of quality of life in infertile women with pcos: A randomized clinical trial. Eur Psychiatry. 2021; 64(S1):S789. [DOI:10.1192/j.eurpsy.2021.2086]
- Jamalomidi N, Hassani F, Kochakentezar R. [Comparison of the effectiveness of emotional focused therapy with cognitive behavioral therapy on the quality of life in obese women with polycystic ovary syndrome (Persian)]. Med J Mashhad Univ Med Sci. 2021; 64(4):3356-68. [DOI:10.22038/mjms.2021.19462]
- Jalilian F, Kaboudi M, TehraniZadeh M, Naghizadeh Moghari F, Montazer A. [The effect of cognitive behavioral counseling on quality of life in women with polycystic ovarian syndrome (Persian)]. Payesh 2018; 17(6):667-76. [Link]
- Majidzadeh S, Mirghafourvand M, Farvareshi M, Yavarikia P. The effect of cognitive behavioral therapy on depression and anxiety of women with polycystic ovary syndrome: A randomized controlled trial. BMC Psychiatry. 2023; 23(1):332. [DOI:10.1186/s12888-023-04814-9] [PMID] [PMCID]
- Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil, H. Chapter 11: Scoping reviews (2020 version). In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. Miami: JBI; 2020. [Link]
- Sarbandi M, Mohamadkhani S, Moradi A. [The effect of childbirth and parenting program training based on mindfulness on pregnancy anxiety and marital satisfaction of pregnant women (Persian)]. J Behav Sci. 2013; 8(4):17-8. [Link]
- Brand S, Holsboer-Trachsler E, Naranjo JR, Schmidt S. Influence of mindfulness practice on cortisol and sleep in long-term and short-term meditators. Neuropsychobiology. 2012; 65(3):109-18. [DOI:10.1159/000330362] [PMID]
- Tang R, Yang J, Yu Y, Fang Y. The effects of cognitive behavioral therapy in women with polycystic ovary syndrome: A meta-analysis. Front Psychol. 2022; 13:796594. [DOI:10.3389/fpsyg.2022.796594] [PMID] [PMCID]
- Lindhardt CL, Glintborg D, Skovsager Andersen M, Ravn P, Møller L. Motivational interviewing used in a an randomised trial for obese women with polycystic ovarian syndrome (PCOs). Paper presented at: Åben Forskerdag, 28 April 2016; Fredericia, Denmark. [Link]
- Arkowitz H, Rollnick S, Miller WR. Motivational interviewing in the treatment of psychological problems. New York: Guilford Publications; 2017. [Link]
Type of Study: review |
Subject:
Psychology
Received: 2023/01/10 | Accepted: 2023/05/20 | Published: 2023/07/1
Received: 2023/01/10 | Accepted: 2023/05/20 | Published: 2023/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







