Thu, May 22, 2025
[Archive]
Volume 1, Issue 4 (Summer 2023)
CPR 2023, 1(4): 474-489 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ashabi B, Salari N, Mahmoudi E, Golezar S. The Relationship Between Mindfulness and Sleep Quality of Postmenopausal Women. CPR 2023; 1 (4) :474-489
URL: http://cpr.mazums.ac.ir/article-1-69-en.html
URL: http://cpr.mazums.ac.ir/article-1-69-en.html
Department of Reproductive Health, School of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran.
Full-Text [PDF 2033 kb]
(311 Downloads)
| Abstract (HTML) (1197 Views)
Full-Text: (244 Views)
Introduction
Menopause refers to when the menstrual period in women stops permanently [1]. Due to the increase in life expectancy, many women spend more than a third of their lives after menopause [2]. It is expected that by 2025, the population of postmenopausal women will reach about 1.1 billion people in the world [3]. Common problems during menopause include vasomotor symptoms, vulvovaginal atrophy, urinary incontinence, sexual dysfunction, headache, and sleep disorders [3]. Sleep disorder is a serious problem at the level of public health, which includes problems in the quality, amount, and timing of sleep [4، 5]. The prevalence of sleep disorders is higher in women, and menopause is known as a factor in increasing the incidence of sleep disorders in women [4]. Sleep problems of postmenopausal women include frequent waking up, difficulty falling asleep, and waking up early in the morning [6]. Effective factors in the occurrence of sleep disorders in postmenopausal women include vasomotor symptoms, circadian rhythm disorder, exacerbation of primary insomnia, changes in hormone levels, lifestyle, and physical and mental illnesses [7]. According to the Study of Women's Health Across the Nation (SWAN), sleep disorders increase with age. According to this study, the prevalence of sleep disorders in women is 16-42% before menopause, 39-47% around menopause, and 35-60% after menopause [8]. Low-quality sleep or lack of sleep is associated with harmful consequences for humans, including a decrease in energy levels, fatigue, impaired concentration, irritability, the development or exacerbation of psychological disorders such as depression and anxiety, impaired decision-making ability, and chronic diseases such as diabetes, heart disease, congestive heart failure, arthritis and Parkinson’s [5]. Sleep quality is essential for health and quality of life. Therefore, sleep problems of postmenopausal women should not be neglected [9].
Mindfulness can be mentioned among the important factors related to optimal sleep quality [13]. Kabat-Zinn defined mindfulness as: "The awareness that arises from paying attention, on purpose, in the present moment, and non-judgmentally" [10]. Hence, it can be said that mindfulness is a conscious and purposeful focus on current events without having a judgmental point of view [11]. The benefits of high mindfulness in people include reduced rumination, reduced stress, improved working memory, increased concentration, reduced emotional reaction to distressing events, increased cognitive flexibility, increased ability to express feelings to spouse, followed by marital satisfaction, increased body immune function, reduced psychological distress and increased speed of information processing [12]. Increased amount of mindfulness in people is associated with improved quality of sleep [13-17]. A high level of mindfulness, by increasing awareness of mental and physical states and learning how to change mental processes, can create an adaptive response to insomnia and thus improve the quality of sleep [18].
Due to the increase in life expectancy, the population of postmenopausal women in the world is increasing, whose health problems can put a high burden on societies. Several studies have been conducted on the relationship between mindfulness and sleep quality in different age groups and patients with different physical conditions [13-17], but no study has been conducted in postmenopausal women despite the high prevalence of sleep disorders in them. Therefore, this study aims to determine the relationship between mindfulness and sleep quality in postmenopausal women in Iran.
Materials and Methods
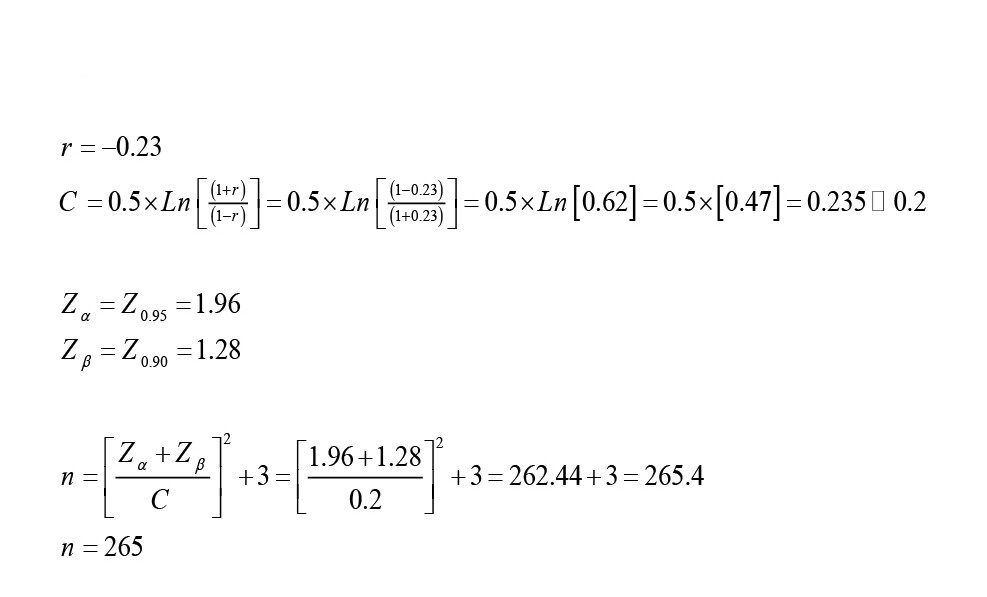
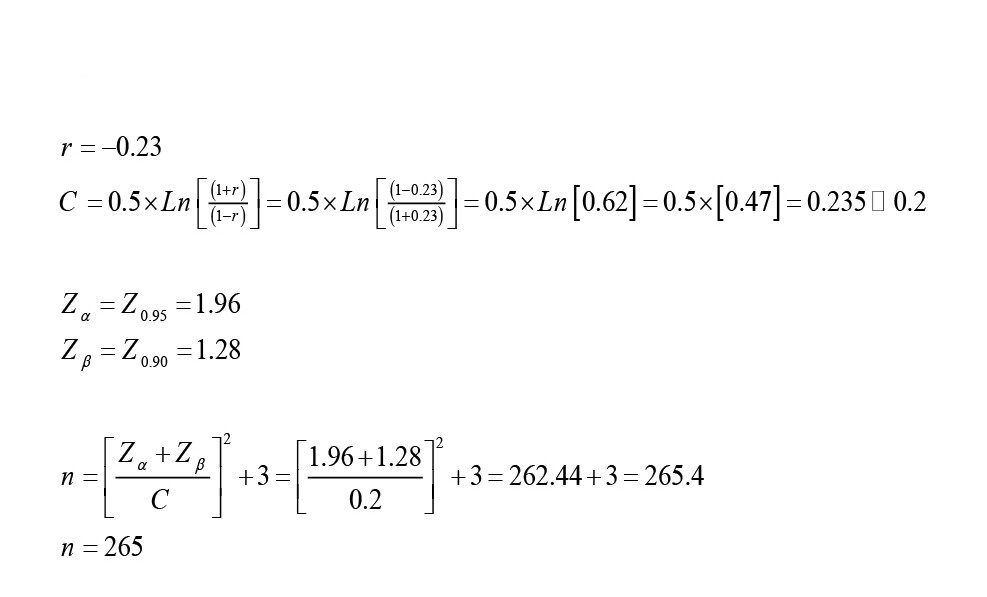
This cross-sectional study was conducted in 2021. The study population included all postmenopausal women who visited health centers in Kermanshah, Iran. The criteria for entering the study were age 50-60 years, absence of menstruation for at least 1 year, no previous history of sleep disorders, no previous history of psychological disorders, and being literate. The criterion for withdrawing from the study was the unwillingness to continue participation in the study. The sample size was determined 265 using the Equation 1 and based on Michelle Park’s study, which examined the correlation between sleep quality score and mindfulness [13].
1.
Therefore, 265 eligible women were selected by a convenience sampling method. Data collection tools included a demographic/obstetric form, the five facet mindfulness questionnaire (FFMQ), and the Pittsburgh sleep quality index (PSQI).
The FFMQ was designed by Baer et al. in 2006. It has 39 items and five subscales of observing, describing, acting with awareness, non-judgmental, and non-reactive. Scoring is based on a Likert scale from never (1 point) to always (5 points). Items 3, 5, 8, 10, 12, 13, 14, 16, 17, 18, 22, 23, 25, 28, 30, 34, 35, 38, and 39 have reversed scoring. The total score ranges from 39 to 195, where a higher score indicates greater mindfulness. Regarding its internal consistency, Cronbach’s α coefficient is 0.91 for the describing subscale and 0.75 for the non-reactivity subscale, observing=0.83, acting with awareness=0.87, describing=0.91, non judging=0.87 [19]. Ahmadvand et al confirmed the validity and reliability of the Persian version of FFMQ [20].
The PSQI was developed by Buysse et al. in 1989. This questionnaire has 9 items, but since item 5 has 10 sub-items, the whole questionnaire has 19 items, which are graded on a 4-point Likert scale from 0 to 3. The total score ranges from 0 to 21, where a lower score indicates better sleep quality. The subscales of this inventory are subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Buysse et al. reported the internal consistency of this questionnaire using Cronbach‘s α as 0.83 [21]. The validity and reliability of the Persian version of PSQI have been confirmed in various studies [22، 23].
After obtaining permission from the university, the researchers visited the health centers. After explaining the study objectives to the participants, their written informed consent was obtained. Then, they completed the questionnaires. The collected data were analyzed in SPSS software, version 25. The significance level was set at 0.05.
Results
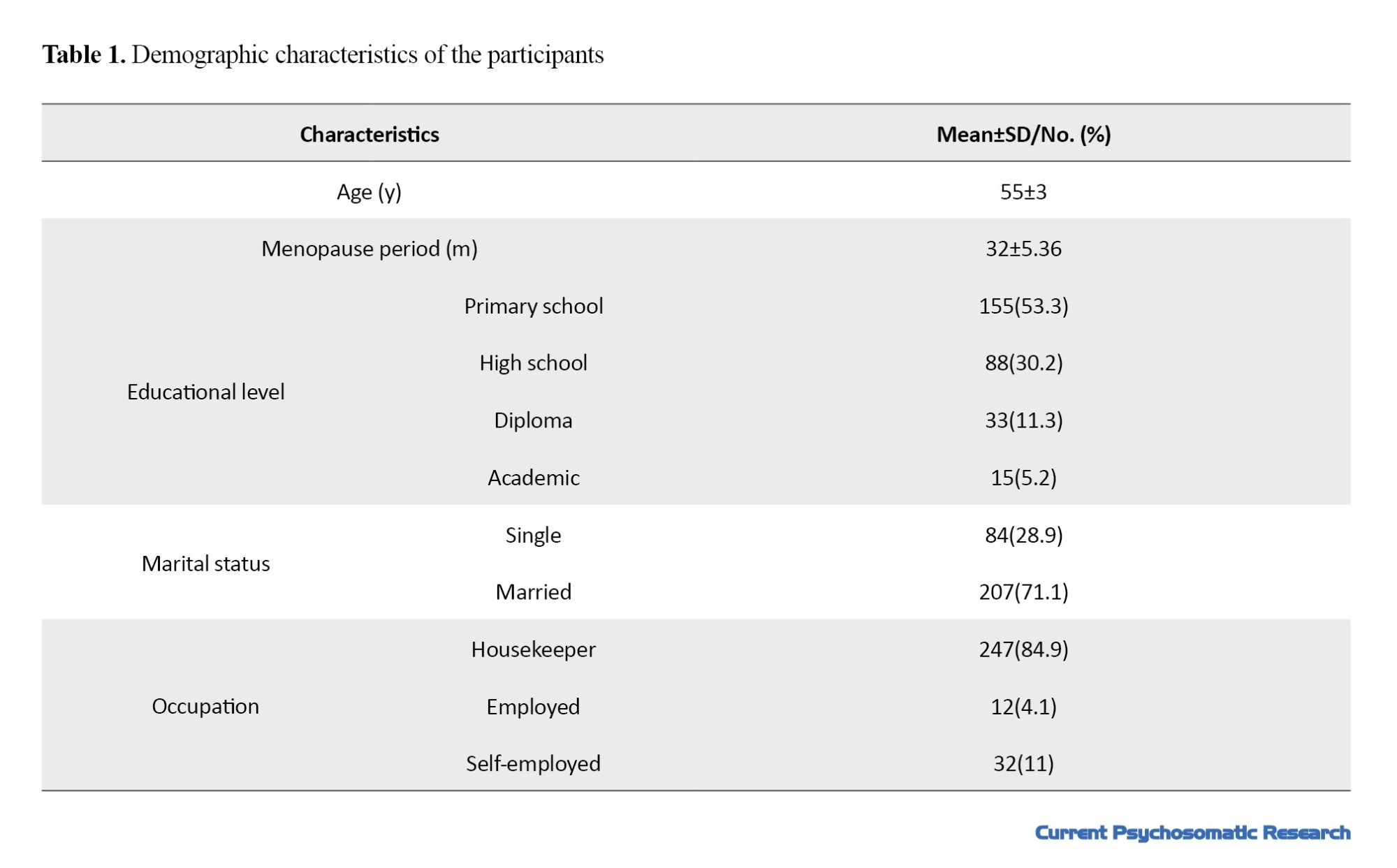
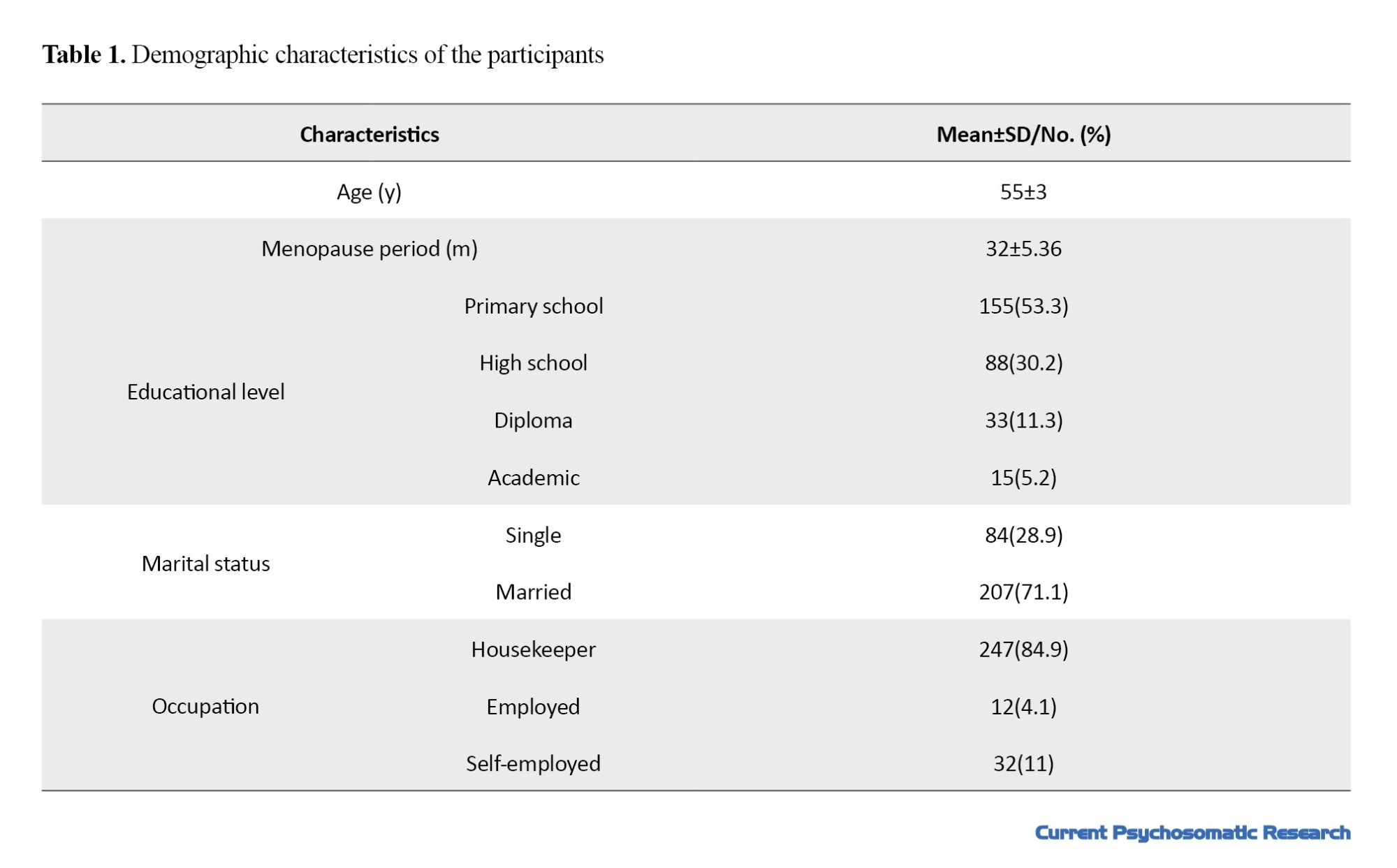
In this study, 291 postmenopausal women with a mean age of 55±3 years (ranged 50-60 years) participated. Most of them had primary school education (53.3%) and were housekeeper (84.9%) and married (71.1%). The were menopause for 32±5.36 (months) (Table 1). The average time since menopause was 32±5.36 months (Table 1).
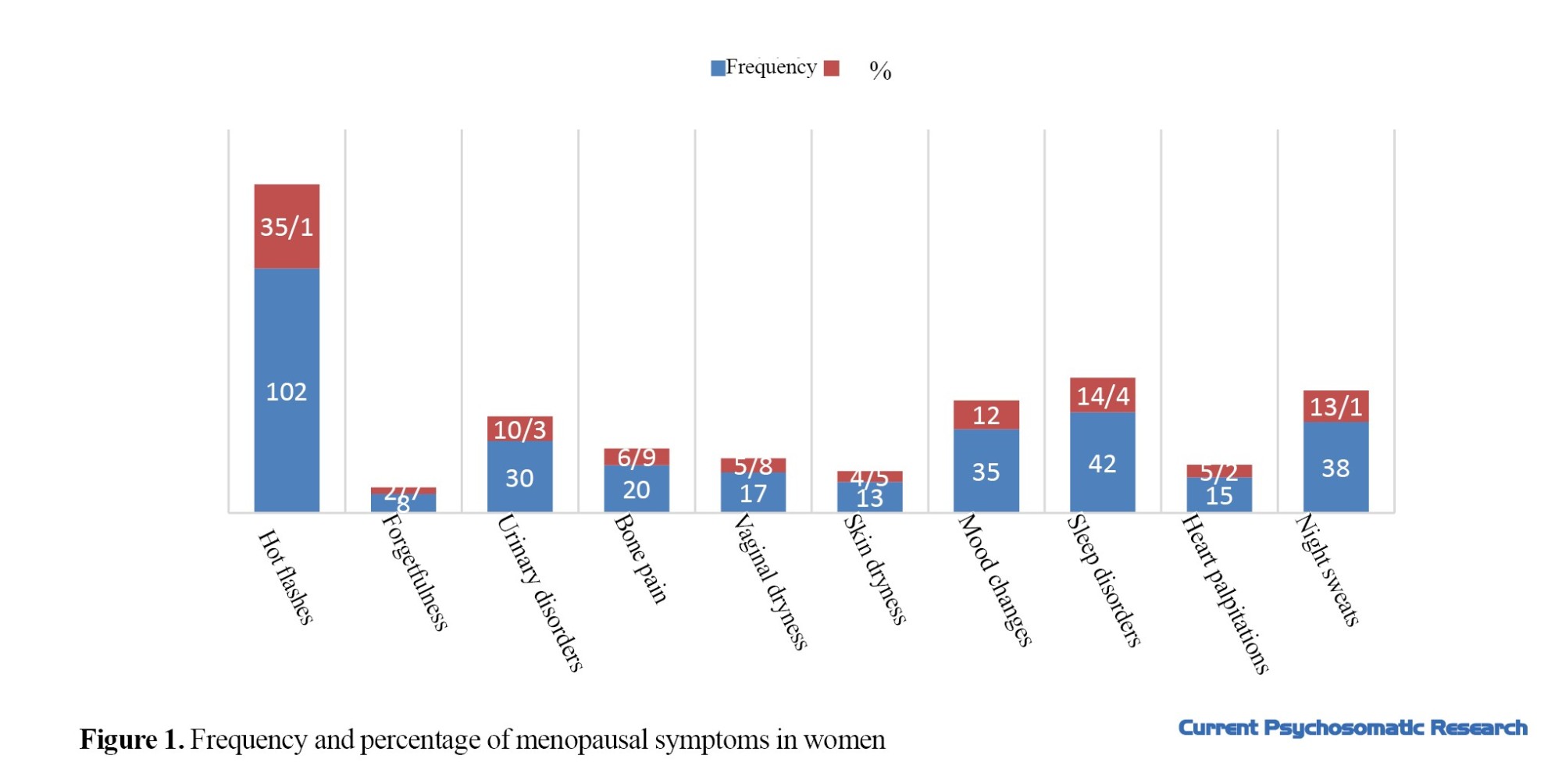
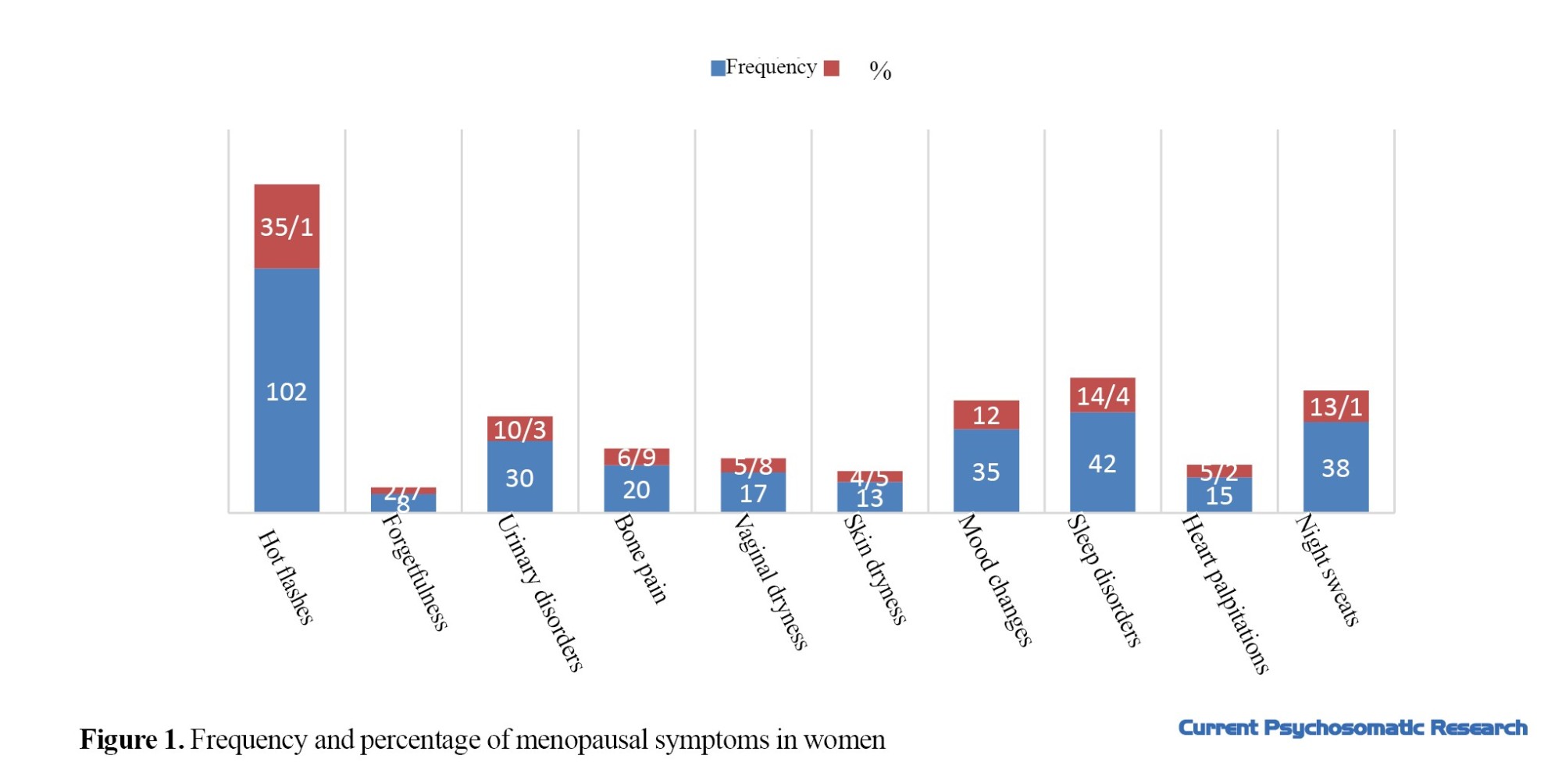
The frequency and percentage of menopausal symptoms in postmenopausal women are shown in Figure 1.
The mean scores of the overall PSQI was 5.8±1.12; for the subjective sleep quality, 1.35±1.03; for sleep latency, 1.13±0.83; for sleep duration, 0.45±0.69; for habitual sleep efficiency, 0.97±1.1; for sleep disturbances, 1.07±0.34; for the use of sleeping medication, 0.13±0.46; and for daytime dysfunction, 0.76±0.65. The mean score of the overall FFMQ was 103.9±41.6; for the components of observing, describing, acting with awareness, non-judgmental and non-reactivity, the mean scores were 21.7±8.9, 19.1±7.9, 21.8±9.1, and 21.9±8.9, 19.3±7.8 respectively.
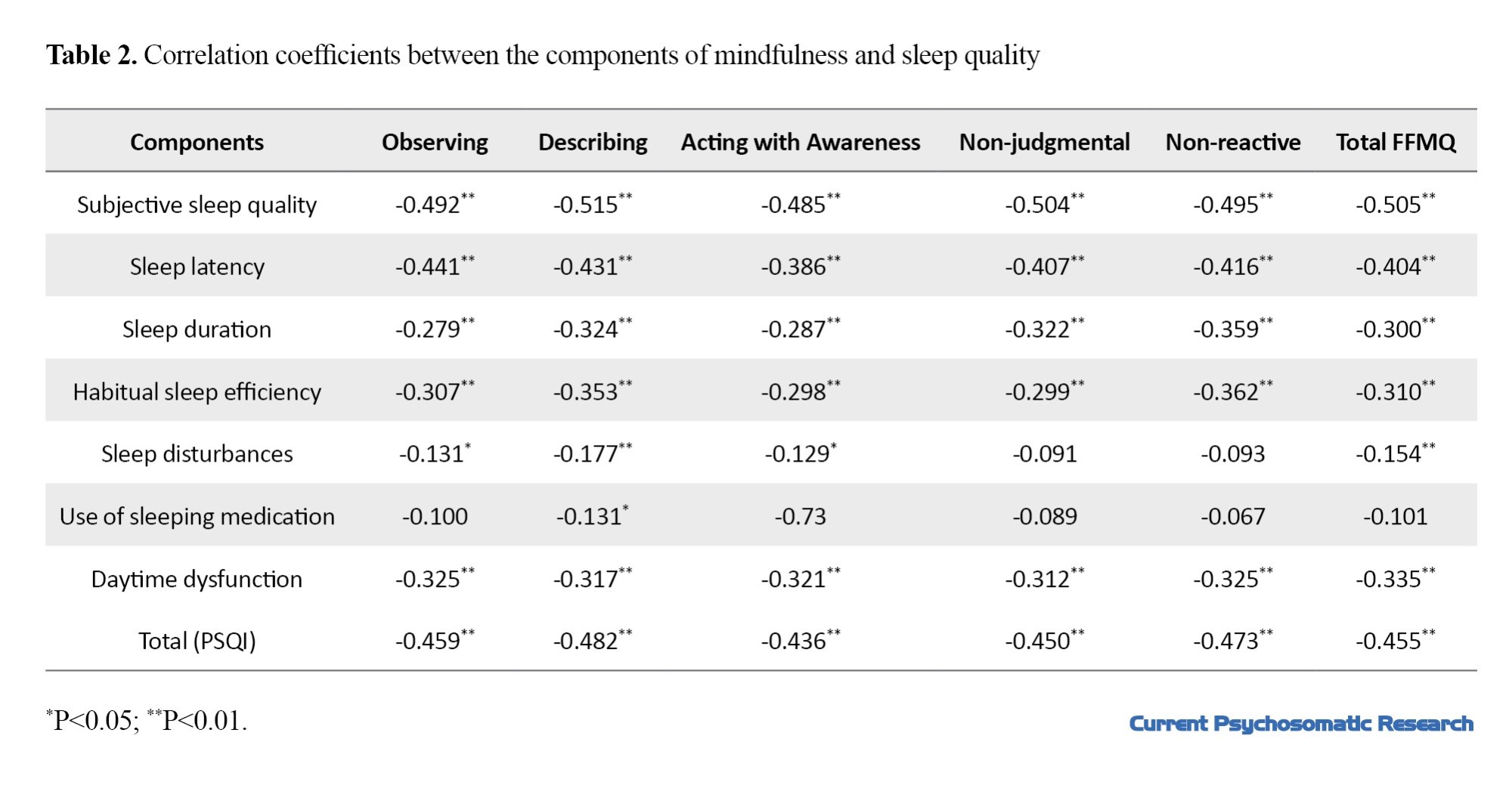
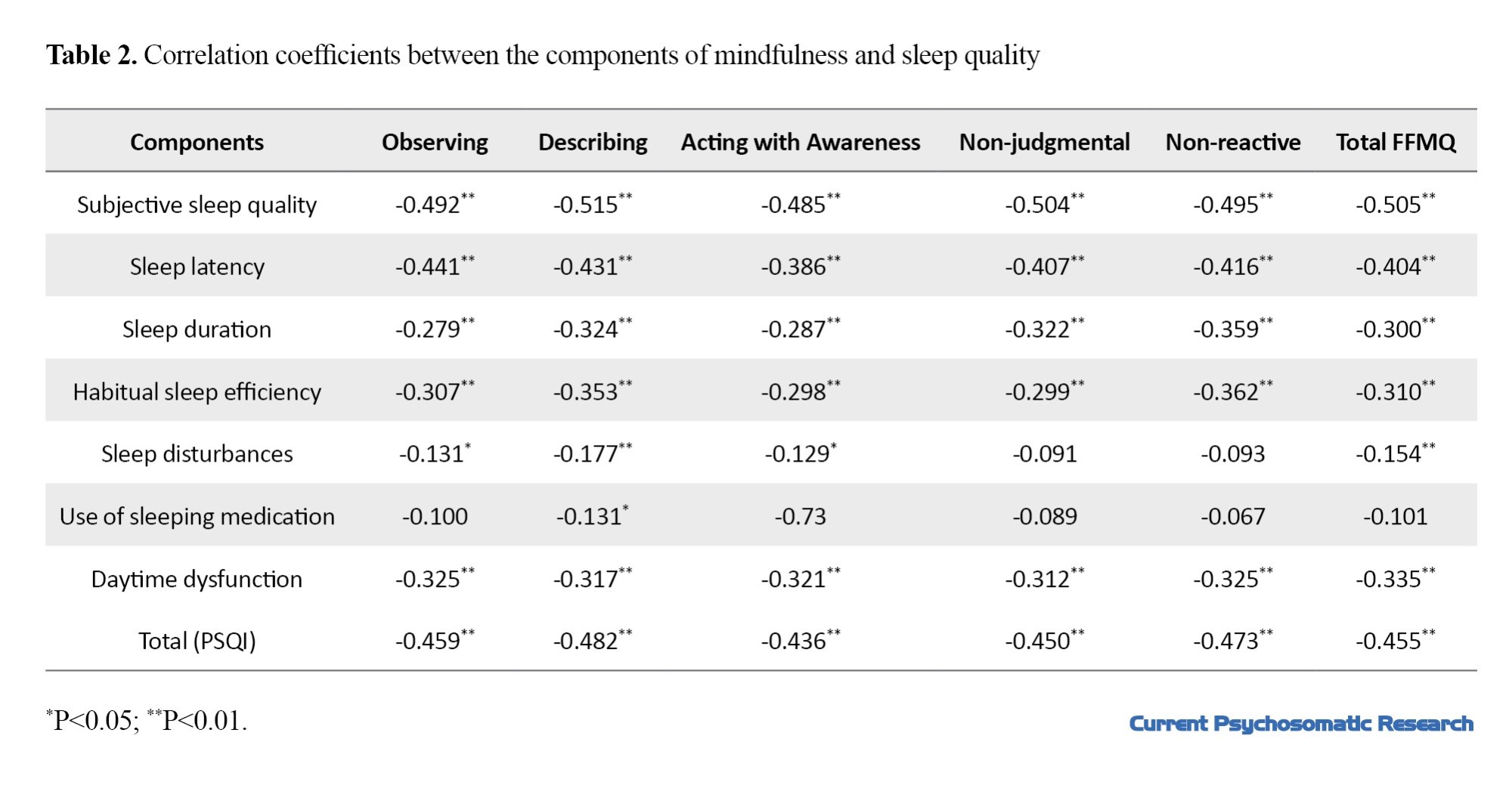
The distribution of the data was non-normal; therefore, Spearman’s correlation test was used to evaluate the relationship between mindfulness and sleep quality. Table 2 shows the correlation coefficients between the components of mindfulness and sleep quality. Since the low scores of PSQI indicate better sleep quality, the results showed that by increasing mindfulness, the sleep quality of postmenopausal women also improves.
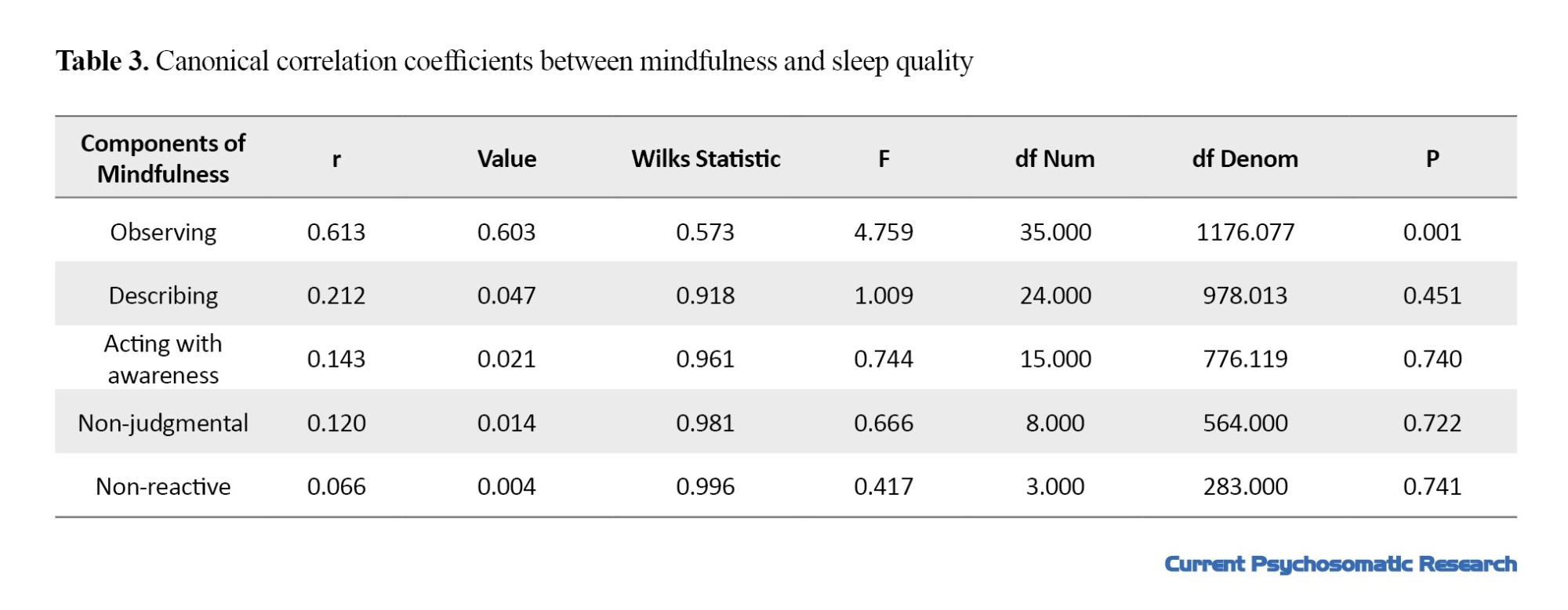
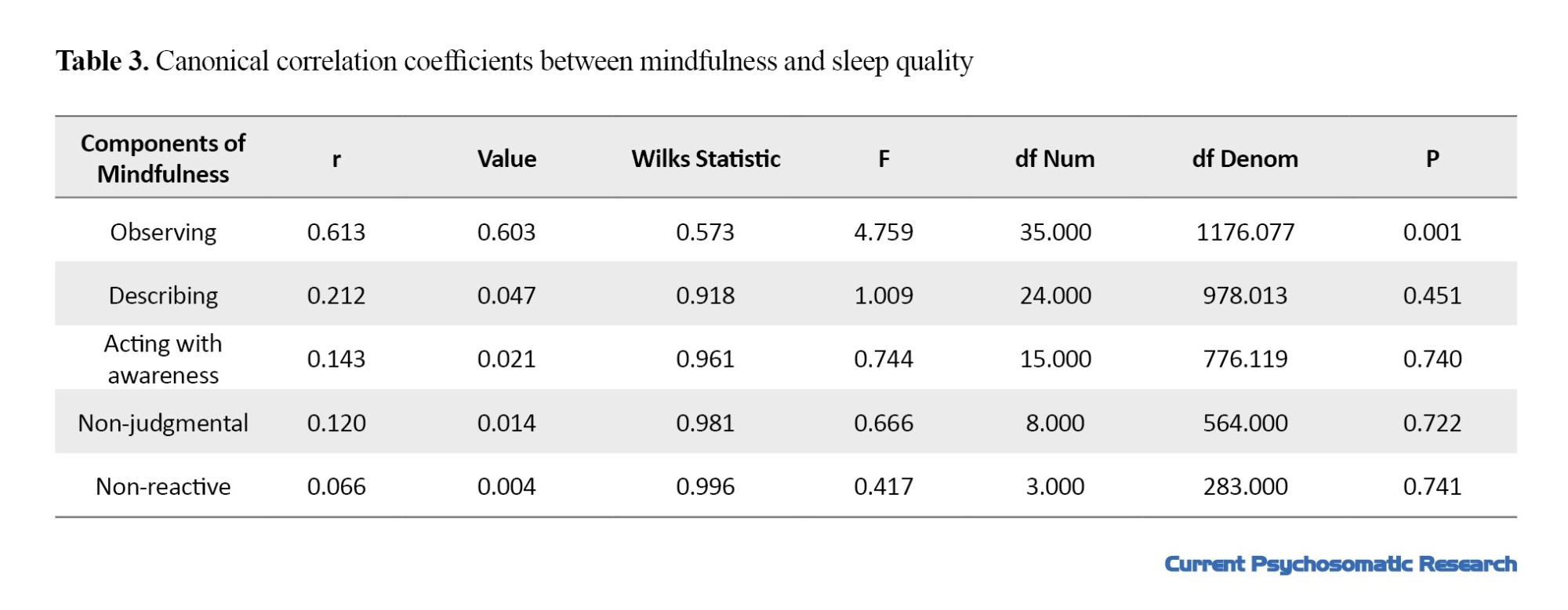
According to Table 3, the canonical correlation coefficient between the two canonical variables of mindfulness and sleep quality was 0.613 and significant (P<0.05). The square of the canonical correlation coefficient (canonical root) was 0.375, indicating that the main variables related to mindfulness predict 37.5% of the changes in the main variables related to sleep quality or vice versa.
According to Table 4 the variables of observing, describing, acting with awareness, non-judgmental, and non-reactive with canonical loads of -0.96, -0.96, -0.95, -0.98, and -0.96 had a significant role in predicting sleep quality. The square of these canonical loads was 0.92, 0.92, 0.90, 0.96, and 0.92, respectively, indicating that, in predicting the sleep quality, the contribution of the observing factor was 92%; the describing factor had a contribution of 92%; acting with awareness had a contribution of 90%; non-judgmental factor, 96%; and non-reactive factor, 92%.
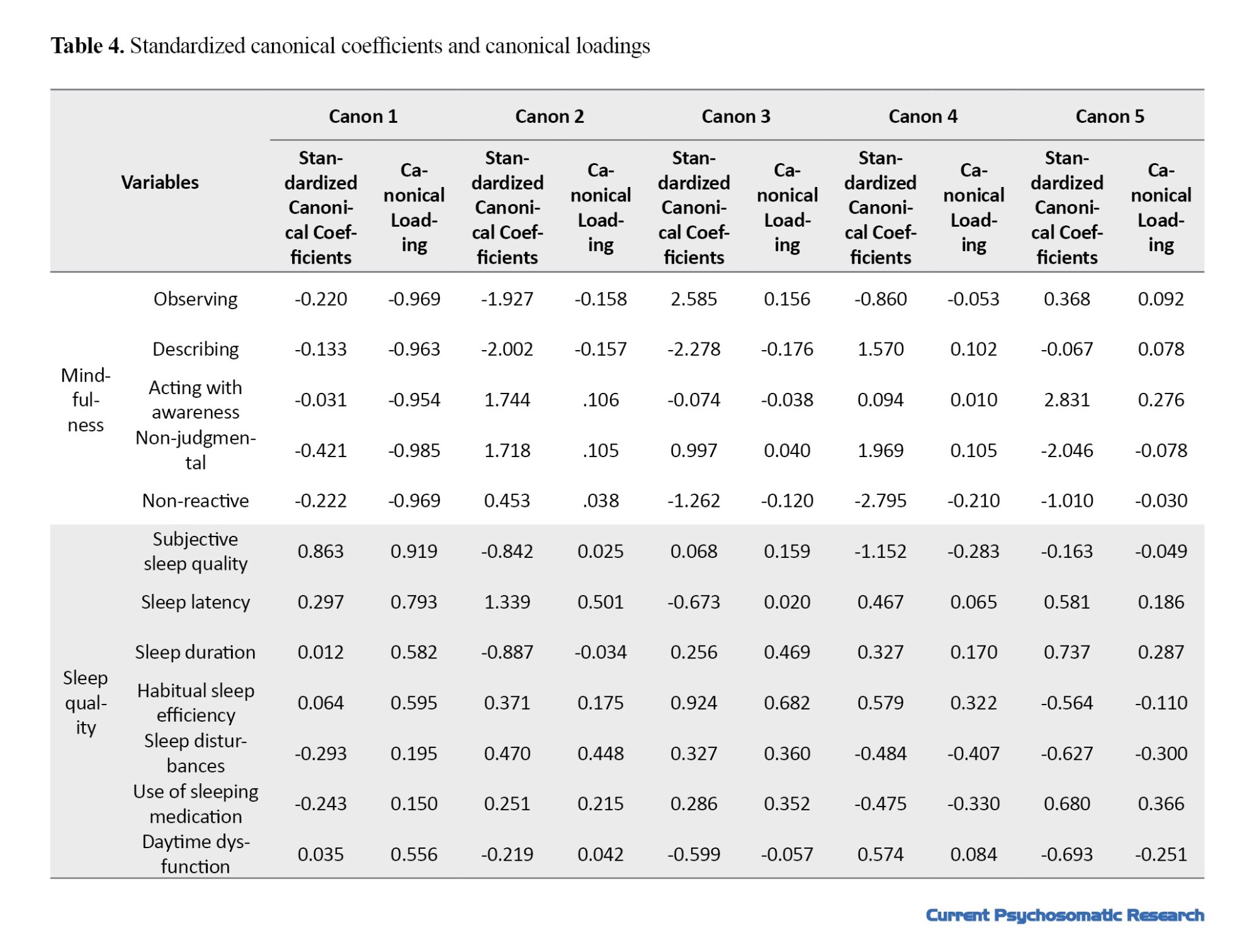
The variables of subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction with canonical loads of 0.91, 0.79, 0.58, 0.59, 0.19, 0.15, and 0.55 had a significant role in predicting mindfulness level. The square of these canonical loads were 0.82, 0.62, 0.33, 0.34, 0.03, 0.02, and 0.30, respectively, indicating that, in predicting mindfulness, the contribution of subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction was 82%, 62%, 33%, 34%, 3%, 2%, and 30%, respectively (Table 4).
Discussion
In the current study, the relationship between mindfulness and sleep quality of postmenopausal women was evaluated. According to the findings, there was a significant association between sleep quality and mindfulness of postmenopausal women; with the increase in mindfulness, the quality of sleep increased. The results are consistent with the results of Liu et al., Ding et al. and Park et al. [13، 15، 24]. In explaining this finding, it can be said that women with sleep problems complain about the inability to control their thoughts while lying in bed. Mindfulness increases psychological well-being and reduces mental rumination, and thus women are less likely to have psychological conflicts before sleep. Mindfulness stimulates the relaxation response, which allows the body to restore itself and reduce stress levels. Many of the benefits of mindfulness come from its impact on the stress response, which effectively improves sleep quality.
In the present study, it was reported that the mindfulness components of observing, describing, acting with awareness, non-judgmental, and non-reactive had a significant role in predicting sleep quality. This finding is consistent with the results of Ding et al. who showed that awareness, non-judgment, and non-reactivity are vital for improving sleep quality [24]. Awareness causes the acceptance of life events without exaggeration. Acceptance allows an unpleasant event to occur without appraisal (non-judgment) and without any effort to stand and resist (non-reactivity).
Various studies have shown the indirect effects of stress on poor sleep quality through pre-sleep arousal and high levels of rumination and worry [25]. Mindfulness acts as a protective factor against negative emotions and leads to a reduction in rumination or mood disorders, which ultimately leads to improved sleep quality [24]. Mindfulness reduces rumination and stress by creating an open and receptive attitude towards thoughts, emotional feelings, and physical reactions. Mindfulness causes self-regulation of behaviors, including increasing attention to respond to bodily cues such as sleepiness and separation from everyday worries, and thus causes restful sleep [26]. Mindfulness has a mutual relationship with sleep quality; as mindfulness improves sleep quality, a good sleep quality strengthens mindfulness [26]. Rusch et al. and Chen et al. also showed that mindfulness improves sleep quality [27، 28].
Based on the results, it can be concluded that mindfulness has a significant relationship with the sleep quality of postmenopausal women. Therefore, it is necessary to think about possible solutions for better provision of mental health services, including mindfulness intervention in comprehensive health centers for these women. Future studies are recommended to compare mindfulness intervention with other psychological techniques in improving the sleep quality of postmenopausal women. Moreover, to obtain more comprehensive results, similar studies are recommended on other groups using a larger sample size. One of the limitations of this study was the old age and low educational level of the women, which made it difficult for them to understand the questions in the questionnaires. To solve this problem, we explained the questions to the participants in person.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Kermanshah University of Medical Sciences (Code: IR.KUMS.REC.1400.598).
Funding
This project was funded by the student research committee of Kermanshah University of Medical Sciences Kermanshah University of Medical Sciences.
Authors' contributions
Study design: Bita Ashabi and Smira Golezar; Supervision: Samira Golezar; Data analysis and data interpretation: Nader Salari and Bita Ashabi; Data collection and writing: Bita Ashabi and Ehsan Mahmoudi; review and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the student research committee of Kermanshah University of Medical Sciences, the management of the Health Organization in Kermanshah Province, and all the women participated in this study for their cooperation.
Menopause refers to when the menstrual period in women stops permanently [1]. Due to the increase in life expectancy, many women spend more than a third of their lives after menopause [2]. It is expected that by 2025, the population of postmenopausal women will reach about 1.1 billion people in the world [3]. Common problems during menopause include vasomotor symptoms, vulvovaginal atrophy, urinary incontinence, sexual dysfunction, headache, and sleep disorders [3]. Sleep disorder is a serious problem at the level of public health, which includes problems in the quality, amount, and timing of sleep [4، 5]. The prevalence of sleep disorders is higher in women, and menopause is known as a factor in increasing the incidence of sleep disorders in women [4]. Sleep problems of postmenopausal women include frequent waking up, difficulty falling asleep, and waking up early in the morning [6]. Effective factors in the occurrence of sleep disorders in postmenopausal women include vasomotor symptoms, circadian rhythm disorder, exacerbation of primary insomnia, changes in hormone levels, lifestyle, and physical and mental illnesses [7]. According to the Study of Women's Health Across the Nation (SWAN), sleep disorders increase with age. According to this study, the prevalence of sleep disorders in women is 16-42% before menopause, 39-47% around menopause, and 35-60% after menopause [8]. Low-quality sleep or lack of sleep is associated with harmful consequences for humans, including a decrease in energy levels, fatigue, impaired concentration, irritability, the development or exacerbation of psychological disorders such as depression and anxiety, impaired decision-making ability, and chronic diseases such as diabetes, heart disease, congestive heart failure, arthritis and Parkinson’s [5]. Sleep quality is essential for health and quality of life. Therefore, sleep problems of postmenopausal women should not be neglected [9].
Mindfulness can be mentioned among the important factors related to optimal sleep quality [13]. Kabat-Zinn defined mindfulness as: "The awareness that arises from paying attention, on purpose, in the present moment, and non-judgmentally" [10]. Hence, it can be said that mindfulness is a conscious and purposeful focus on current events without having a judgmental point of view [11]. The benefits of high mindfulness in people include reduced rumination, reduced stress, improved working memory, increased concentration, reduced emotional reaction to distressing events, increased cognitive flexibility, increased ability to express feelings to spouse, followed by marital satisfaction, increased body immune function, reduced psychological distress and increased speed of information processing [12]. Increased amount of mindfulness in people is associated with improved quality of sleep [13-17]. A high level of mindfulness, by increasing awareness of mental and physical states and learning how to change mental processes, can create an adaptive response to insomnia and thus improve the quality of sleep [18].
Due to the increase in life expectancy, the population of postmenopausal women in the world is increasing, whose health problems can put a high burden on societies. Several studies have been conducted on the relationship between mindfulness and sleep quality in different age groups and patients with different physical conditions [13-17], but no study has been conducted in postmenopausal women despite the high prevalence of sleep disorders in them. Therefore, this study aims to determine the relationship between mindfulness and sleep quality in postmenopausal women in Iran.
Materials and Methods
This cross-sectional study was conducted in 2021. The study population included all postmenopausal women who visited health centers in Kermanshah, Iran. The criteria for entering the study were age 50-60 years, absence of menstruation for at least 1 year, no previous history of sleep disorders, no previous history of psychological disorders, and being literate. The criterion for withdrawing from the study was the unwillingness to continue participation in the study. The sample size was determined 265 using the Equation 1 and based on Michelle Park’s study, which examined the correlation between sleep quality score and mindfulness [13].
1.
Therefore, 265 eligible women were selected by a convenience sampling method. Data collection tools included a demographic/obstetric form, the five facet mindfulness questionnaire (FFMQ), and the Pittsburgh sleep quality index (PSQI).
The FFMQ was designed by Baer et al. in 2006. It has 39 items and five subscales of observing, describing, acting with awareness, non-judgmental, and non-reactive. Scoring is based on a Likert scale from never (1 point) to always (5 points). Items 3, 5, 8, 10, 12, 13, 14, 16, 17, 18, 22, 23, 25, 28, 30, 34, 35, 38, and 39 have reversed scoring. The total score ranges from 39 to 195, where a higher score indicates greater mindfulness. Regarding its internal consistency, Cronbach’s α coefficient is 0.91 for the describing subscale and 0.75 for the non-reactivity subscale, observing=0.83, acting with awareness=0.87, describing=0.91, non judging=0.87 [19]. Ahmadvand et al confirmed the validity and reliability of the Persian version of FFMQ [20].
The PSQI was developed by Buysse et al. in 1989. This questionnaire has 9 items, but since item 5 has 10 sub-items, the whole questionnaire has 19 items, which are graded on a 4-point Likert scale from 0 to 3. The total score ranges from 0 to 21, where a lower score indicates better sleep quality. The subscales of this inventory are subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Buysse et al. reported the internal consistency of this questionnaire using Cronbach‘s α as 0.83 [21]. The validity and reliability of the Persian version of PSQI have been confirmed in various studies [22، 23].
After obtaining permission from the university, the researchers visited the health centers. After explaining the study objectives to the participants, their written informed consent was obtained. Then, they completed the questionnaires. The collected data were analyzed in SPSS software, version 25. The significance level was set at 0.05.
Results
In this study, 291 postmenopausal women with a mean age of 55±3 years (ranged 50-60 years) participated. Most of them had primary school education (53.3%) and were housekeeper (84.9%) and married (71.1%). The were menopause for 32±5.36 (months) (Table 1). The average time since menopause was 32±5.36 months (Table 1).
The frequency and percentage of menopausal symptoms in postmenopausal women are shown in Figure 1.
The mean scores of the overall PSQI was 5.8±1.12; for the subjective sleep quality, 1.35±1.03; for sleep latency, 1.13±0.83; for sleep duration, 0.45±0.69; for habitual sleep efficiency, 0.97±1.1; for sleep disturbances, 1.07±0.34; for the use of sleeping medication, 0.13±0.46; and for daytime dysfunction, 0.76±0.65. The mean score of the overall FFMQ was 103.9±41.6; for the components of observing, describing, acting with awareness, non-judgmental and non-reactivity, the mean scores were 21.7±8.9, 19.1±7.9, 21.8±9.1, and 21.9±8.9, 19.3±7.8 respectively.
The distribution of the data was non-normal; therefore, Spearman’s correlation test was used to evaluate the relationship between mindfulness and sleep quality. Table 2 shows the correlation coefficients between the components of mindfulness and sleep quality. Since the low scores of PSQI indicate better sleep quality, the results showed that by increasing mindfulness, the sleep quality of postmenopausal women also improves.
According to Table 3, the canonical correlation coefficient between the two canonical variables of mindfulness and sleep quality was 0.613 and significant (P<0.05). The square of the canonical correlation coefficient (canonical root) was 0.375, indicating that the main variables related to mindfulness predict 37.5% of the changes in the main variables related to sleep quality or vice versa.
According to Table 4 the variables of observing, describing, acting with awareness, non-judgmental, and non-reactive with canonical loads of -0.96, -0.96, -0.95, -0.98, and -0.96 had a significant role in predicting sleep quality. The square of these canonical loads was 0.92, 0.92, 0.90, 0.96, and 0.92, respectively, indicating that, in predicting the sleep quality, the contribution of the observing factor was 92%; the describing factor had a contribution of 92%; acting with awareness had a contribution of 90%; non-judgmental factor, 96%; and non-reactive factor, 92%.
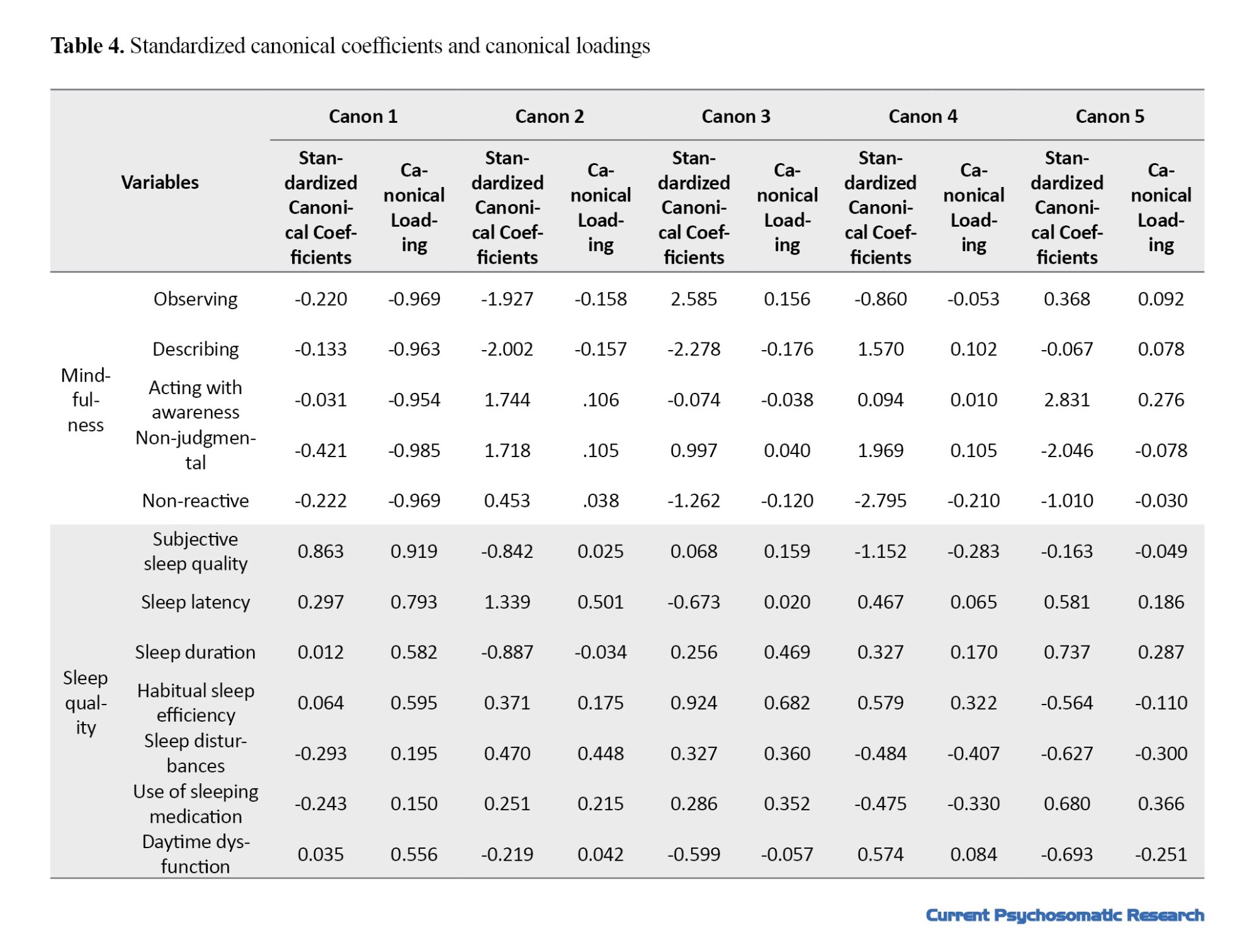
The variables of subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction with canonical loads of 0.91, 0.79, 0.58, 0.59, 0.19, 0.15, and 0.55 had a significant role in predicting mindfulness level. The square of these canonical loads were 0.82, 0.62, 0.33, 0.34, 0.03, 0.02, and 0.30, respectively, indicating that, in predicting mindfulness, the contribution of subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction was 82%, 62%, 33%, 34%, 3%, 2%, and 30%, respectively (Table 4).
Discussion
In the current study, the relationship between mindfulness and sleep quality of postmenopausal women was evaluated. According to the findings, there was a significant association between sleep quality and mindfulness of postmenopausal women; with the increase in mindfulness, the quality of sleep increased. The results are consistent with the results of Liu et al., Ding et al. and Park et al. [13، 15، 24]. In explaining this finding, it can be said that women with sleep problems complain about the inability to control their thoughts while lying in bed. Mindfulness increases psychological well-being and reduces mental rumination, and thus women are less likely to have psychological conflicts before sleep. Mindfulness stimulates the relaxation response, which allows the body to restore itself and reduce stress levels. Many of the benefits of mindfulness come from its impact on the stress response, which effectively improves sleep quality.
In the present study, it was reported that the mindfulness components of observing, describing, acting with awareness, non-judgmental, and non-reactive had a significant role in predicting sleep quality. This finding is consistent with the results of Ding et al. who showed that awareness, non-judgment, and non-reactivity are vital for improving sleep quality [24]. Awareness causes the acceptance of life events without exaggeration. Acceptance allows an unpleasant event to occur without appraisal (non-judgment) and without any effort to stand and resist (non-reactivity).
Various studies have shown the indirect effects of stress on poor sleep quality through pre-sleep arousal and high levels of rumination and worry [25]. Mindfulness acts as a protective factor against negative emotions and leads to a reduction in rumination or mood disorders, which ultimately leads to improved sleep quality [24]. Mindfulness reduces rumination and stress by creating an open and receptive attitude towards thoughts, emotional feelings, and physical reactions. Mindfulness causes self-regulation of behaviors, including increasing attention to respond to bodily cues such as sleepiness and separation from everyday worries, and thus causes restful sleep [26]. Mindfulness has a mutual relationship with sleep quality; as mindfulness improves sleep quality, a good sleep quality strengthens mindfulness [26]. Rusch et al. and Chen et al. also showed that mindfulness improves sleep quality [27، 28].
Based on the results, it can be concluded that mindfulness has a significant relationship with the sleep quality of postmenopausal women. Therefore, it is necessary to think about possible solutions for better provision of mental health services, including mindfulness intervention in comprehensive health centers for these women. Future studies are recommended to compare mindfulness intervention with other psychological techniques in improving the sleep quality of postmenopausal women. Moreover, to obtain more comprehensive results, similar studies are recommended on other groups using a larger sample size. One of the limitations of this study was the old age and low educational level of the women, which made it difficult for them to understand the questions in the questionnaires. To solve this problem, we explained the questions to the participants in person.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Kermanshah University of Medical Sciences (Code: IR.KUMS.REC.1400.598).
Funding
This project was funded by the student research committee of Kermanshah University of Medical Sciences Kermanshah University of Medical Sciences.
Authors' contributions
Study design: Bita Ashabi and Smira Golezar; Supervision: Samira Golezar; Data analysis and data interpretation: Nader Salari and Bita Ashabi; Data collection and writing: Bita Ashabi and Ehsan Mahmoudi; review and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the student research committee of Kermanshah University of Medical Sciences, the management of the Health Organization in Kermanshah Province, and all the women participated in this study for their cooperation.
References
- American College of Obstetricians and Gynecologists. The menopause years. New York: American College of Obstetricians and Gynecologists; 2018. [Link]
- Lobo RA, Davis SR, De Villiers TJ, Gompel A, Henderson VW, Hodis HN, et al. Prevention of diseases after menopause. Climacteric. 2014; 17(5):540-56. [DOI:10.3109/13697137.2014.933411] [PMID]
- Shifren JL, Gass ML; NAMS Recommendations for Clinical Care of Midlife Women Working Group. The North American Menopause Society recommendations for clinical care of midlife women. Menopause. 2014; 21(10):1038-62. [DOI:10.1097/GME.0000000000000319] [PMID]
- Polo-Kantola P. Sleep and menopause. Women’s Health. 2007; 3(1):99-106. [DOI:10.2217/17455057.3.1.99] [PMID]
- American Psychiatric Association. What are sleep disorders?. Washington, DC: American Psychiatric Association; 2020. [Link]
- Han Y, Lee J, Cho HH, Kim MR. Erratum to: Sleep disorders and menopause. J Menopausal Med. 2019; 25(3):172. [DOI:10.6118/jmm.19192.err] [PMID]
- Ameratunga D, Goldin J, Hickey M. Sleep disturbance in menopause. Intern Med J. 2012; 42(7):742-7. [DOI:10.1111/j.1445-5994.2012.02723.x] [PMID]
- Kravitz HM, Joffe H. Sleep during the perimenopause: A SWAN story. Obstet Gynecol Clin North Am. 2011; 38(3):567-86. [DOI:10.1016/j.ogc.2011.06.002] [PMID]
- Caretto M, Giannini A, Simoncini T. An integrated approach to diagnosing and managing sleep disorders in menopausal women. Maturitas. 2019; 128:1-3. [DOI:10.1016/j.maturitas.2019.06.008] [PMID]
- Niemiec RM. Mindfulness and character strengths: A practical guide to flourishing. Göttingen: Hogrefe; 2013. [DOI:10.1027/00376-000]
- Zinn JK. Wherever you go, there you are: Mindfulness meditation in everyday life. New York: Hyperion; 1994. [Link]
- Davis DM, Hayes JA. What are the benefits of mindfulness. Washington, D.C: American Psychological Association; 2012. [Link]
- Park M, Zhang Y, Price LL, Bannuru RR, Wang C. Mindfulness is associated with sleep quality among patients with fibromyalgia. Int J Rheum Dis. 2020; 23(3):294-301. [DOI:10.1111/1756-185X.13756] [PMID]
- Liu K, Yin T, Shen Q. Relationships between sleep quality, mindfulness and work-family conflict in Chinese nurses: A cross-sectional study. Appl Nurs Res. 2020; 55:151250. [DOI:10.1016/j.apnr.2020.151250] [PMID]
- Liu QQ, Zhou ZK, Yang XJ, Kong FC, Sun XJ, Fan CY. Mindfulness and sleep quality in adolescents: Analysis of rumination as a mediator and self-control as a moderator. Pers Individ Dif. 2018; 122:171-6. [DOI:10.1016/j.paid.2017.10.031]
- Sadri Damirchi E, Cheraghian H. [Modeling of mindfulness and quality of sleep by the mediation of psychological well-being in high school students (Persian)]. J Sch Psychol. 2017; 6(2):100-23. [DOI: 10.22098/JSP.2017.570]
- Visser PL, Hirsch JK, Brown KW, Ryan R, Moynihan JA. Components of sleep quality as mediators of the relation between mindfulness and subjective vitality among older adults. Mindfulness. 2015; 6:723-31. [DOI:10.1007/s12671-014-0311-5]
- Ong JC, Ulmer CS, Manber R. Improving sleep with mindfulness and acceptance: A metacognitive model of insomnia. Behav Res Ther. 2012; 50(11):651-60. [DOI:10.1016/j.brat.2012.08.001] [PMID]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006; 13(1):27-45. [DOI:10.1177/1073191105283504] [PMID]
- Ahmadvand Z, Heydarinasab L, Shaeri M. An investigation of the validity and reliability of psychometric characteristics of five facet mindfulness questionnaire in Iranian non-clinical samples. J Behav Sci. 2013; 7(3):229-37. [Link]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
- Farrahi Moghaddam J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P). Sleep Breath. 2012; 16(1): 79-82. [DOI:10.1007/s11325-010-0478-5] [PMID]
- Ebrahimi AA, Ghalehbandi MF, Salehi M, Tafti AR, Vakili Y, Farsi E. Sleep parameters and the factors affecting the quality of sleep in patients attending selected clinics of Rasoul-e-Akram hospital. Razi J Med Sci. 2008; 15:31-8. [Link]
- Ding X, Wang X, Yang Z, Tang R, Tang YY. Relationship between trait mindfulness and sleep quality in college students: A conditional process model. Front Psychol. 2020; 11:576319. [DOI:10.3389/fpsyg.2020.576319] [PMID]
- Li Y, Gu S, Wang Z, Li H, Xu X, Zhu H, et al. Relationship between stressful life events and sleep quality: rumination as a mediator and resilience as a moderator. Front Psychiatry. 2019; 10:348. [DOI:10.3389/fpsyt.2019.00348] [PMID]
- Howell AJ, Digdon NL, Buro K, Sheptycki AR. Relations among mindfulness, well-being, and sleep. Pers Individ Dif. 2008; 45(8):773-7. [DOI:10.1016/j.paid.2008.08.005]
- Rusch HL, Rosario M, Levison LM, Olivera A, Livingston WS, Wu T, et al. The effect of mindfulness meditation on sleep quality: A systematic review and meta-analysis of randomized controlled trials. Ann N Y Acad Sci. 2019; 1445(1):5-16. [DOI:10.1111/nyas.13996] [PMID]
- Chen TL, Chang SC, Hsieh HF, Huang CY, Chuang JH, Wang HH. Effects of mindfulness-based stress reduction on sleep quality and mental health for insomnia patients: A meta-analysis. J Psychosom Res. 2020; 135:110144. [DOI:10.1016/j.jpsychores.2020.110144] [PMID]
Type of Study: Research |
Subject:
Psychology
Received: 2023/03/17 | Accepted: 2023/05/31 | Published: 2023/07/1
Received: 2023/03/17 | Accepted: 2023/05/31 | Published: 2023/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







