Sat, Feb 21, 2026
[Archive]
Volume 1, Issue 3 (Spring 2023)
CPR 2023, 1(3): 360-371 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Layali I, Abedini E, Ghajar M, Joulaei M. Relationship Between Occupational Stress and Sleep Disorders of Nurses in a Hospital in Sari, Iran. CPR 2023; 1 (3) :360-371
URL: http://cpr.mazums.ac.ir/article-1-57-en.html
URL: http://cpr.mazums.ac.ir/article-1-57-en.html
Department of Biochemistry, Sari Branch, Islamic Azad University, Sari, Iran.
Full-Text [PDF 1504 kb]
(705 Downloads)
| Abstract (HTML) (1608 Views)
Full-Text: (607 Views)
Introduction
Nurses are the largest part of the health care system such that 40% of employees in a hospital are nurses. They need to have a good quality of life to provide quality care to patients [1]. Nursing is a high-risk occupation associated with fatigue and illness [2]. Nurses suffer from significant stress due to their job requirements (workload، physical needs، time pressure، work shifs) [3]. On the other hand، based on the job demands-control pattern of Karasek (1979)، occupations that are associated with high stress and low control can cause psychological and physical distress and lead to sleep disorders and reduced quality of life [4]. Sleep disorders can damage the job and its quality and quantity، lead to a decline in nurses’ performance [5]. When the sleeping cycle is disrupted، other physiological functions of the body may also be disrupted [6]. To achieve maximum efficiency in nurses، they need to have adequate sleep [7]. The decrease in the quality of life and sleep in nurses caused by occupational stress can indirectly affect the quality and accuracy of services provided by them to patients [8]. Sleep facilitates the recovery of fatigue and is considered as an important criterion for the physical، social، and mental health [9, 10, 11, 12]. Poor sleep quality is associated with increased stress، irritability، and depression [13], and can cause medical and non-medical errors [14]. Considering the importance of nursing profession and the prevalence of sleep problems among nurses، and given the lack of sufficient study in this field، this study aims to answer to the question whether occupational stress can predict sleep disorders of nurses in Sari، Iran.
Materials and Method
This is a descriptive-analytical study. Th study population consists of 394 nurses working in Imam Khomeini Hospital in Sari city. Of these، 196 were selected as the sample using a stratified random sampling method. The sample size was determined using Krejcie & Morgan’s table. Inclusion criteria were informed consent to participate in the study and not having a mental illness. Exclusion criteria were the experience of a traumatic event and unwillingness to continue participation. For data collection، in addition to a demographic form (surveying age، sex, marital status, and educational level), two standard questionnaires including Expanded Nursing Stress Scale (ENSS) and sleep quality questionnaire were used.
Questionnaires Including Expanded Nursing Stress Scale (ENSS)
The ENSS is a revised version of the Nursing Stress Scale developed by Gray-Toft and Anderson. It was revised by French et al. to identify stressful situations not mentioned in the Nursing Stress Scale and to increase its scope [15]. This tool has 57 items and 9 subscales of death، conflict with physicians، inadequate emotional preparation، problem with peer support، problems with supervisors، workload، uncertainty about treatment، patients and families، and discrimination [16].The internal consistency is 0.96 for the overall scale, and ranges from 0.65 to 0.88 for its subscales [17]. For its Persian version, Ghiasi et al. reported a Cronbach’s alpha of 0.95 for its internal consistency [18].
The Pittsburgh sleep quality index (PSQI) was designed by Buysse et al. in 1989 to evaluate sleep quality. Its scoring is based on a four-point Likert scale from 0 to 3. The total score ranges from 0 to 21, where higher scores indicate lower sleep quality [19]. The validity and reliability of this questionnaire were confirmed in the studies by Ghaljae et al. [20] and Mahdizade et al. [21].
Data were analyzed in SPSS software, version 20. Frequency, percentage، mean، and standard deviation (SD) were used for descriptive analysis. T test (To compare sleep disorders among nurses with different work shifts)، ANOVA including Pearson correlation coefficient (To assess the effect of independent variable and its dimensions on the dependent variable) test were used for inferential analysis.
Results
Out of 196 participants, 41 (20.9%) were male and 155 (79.1%) were female. Three (1.5%) aged 21-30 years, 59 (30.0%) aged 31-40 years, 77 (39.3%) aged 41-50 years,and 57 (29.1%) aged more than 51 years. In terms of the educational level, 6 (3.1%) had diploma, 165 (84.2%) had bachelor’s degree and 25 (12.8%) had master’s degree and higher. Furthermore, 96 (49.0%) were working the morning shift, 60 (30.6%) on the evening shift، and 40 (20. 4%) on the night shift. The most of participants (42.3%) had 11-20 years of work experience (Table 1).

In examining the assumptions, the Kolmogorov-Smirnov test results showed that the distribution of data was normal, and Durbin-Watson statistic was in the range of 1.5-2.5. Therefore, the conditions for regression analysis were confirmed. As can be seen in Table 2, R value was 0.43 shows the degree of relationship between sleep quality and occupational stress.

R squared value indicated that 19% of the variation in the dependent variable was explained by the independent variable. ANOVA results showed that the regression results were significant. The beta coefficient value indicated that a one unit change in occupational stress could cause a change by 0.43 in the quality of sleep (Table 2).
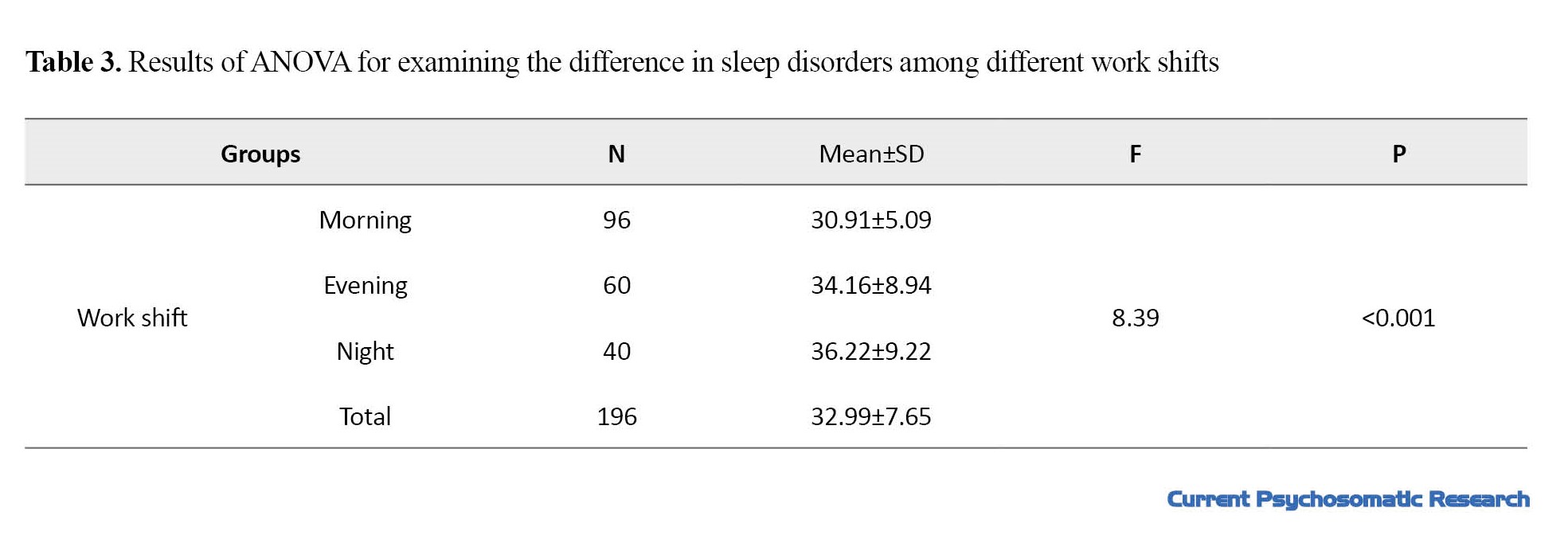
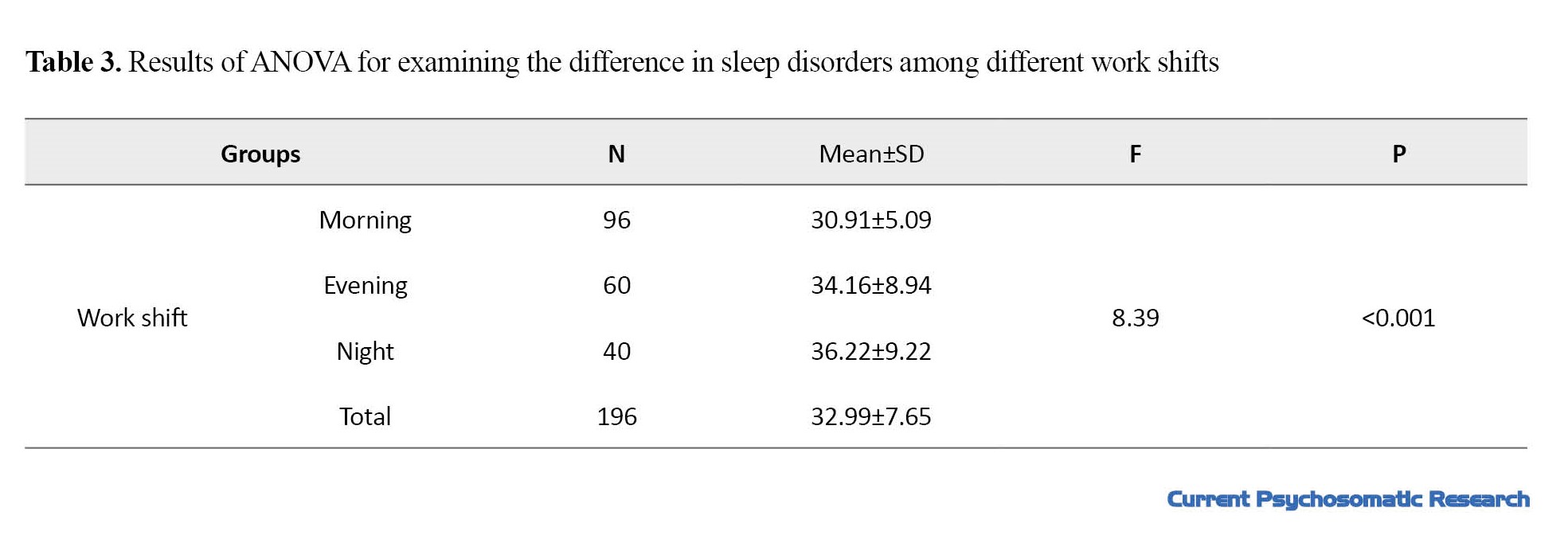
The results of ANOVA showed that sleep disorders were significantly different among nurses with different work shifts (P<0.05). The sleep disorders in those working on the night shift (Mean=36.22) were higher than in those with other two work shifts (Table 3).
The beta coefficients for the domains of ENSS showed that the “conflict with physicians” with a beta value of 0. 99 was the most effective factor and the “problems with peer support” with a beta value of 0.19 was the least effective factor in predicting the sleep disorders of nurses (Table 4).

Discussion
This study showed a significant relationship between occupational stress and sleep disorders in nurses working in Imam Khomeini Hospital in Sari. In a study, Shah reported that the relationship between occupational stress and sleep quality in nurses was significant and negative [1]. Moradi showed a significant correlation between occupational stress and nurses’ fatigue in selected hospitals in Tehran [19]. Today, one of the most important types of stress in people is occupational stress, which is higher among nurses who are in contact with patients. This stress can weaken the immune system, and cause the body to be susceptible to many physical and mental illnesses [20]. In addition، occupational stress disrupts social and family interactions، and creates job dissatisfaction، increased medical errors، decreased decision-making power، and slow response time [21]. Some studies have indicated a high level of occupational stress and physical and psychological problems in nurses [22, 23]. Hospital staff، especially nurses can develop occupational stress due to the large amount of workload، lack of proper equipment in the hospital، inadequate planning، lack of time for providing adequate care for the patients، lack of information، patients’ death، lack of improvement in patient conditions، the atmosphere in the hospital، etc. This can lead to sleep disorders which have negative consequences such as fatigue and aggression [24].
Among the occupational stress domains، conflict with physicians was the strongest predictor of sleep disorders while the problems with peer support was the least strong factor in predicting sleep disorders in nurses. This is consistent with the findings of Yazdi et al. [25]. Salehi et al. investigated the quality of sleep in 176 nurses using the Pittsburgh Sleep Quality Index، and found that only 14% of nurses had a good quality of sleep؛ most of them (86%) had poor sleep quality. They showed that the quality of sleep was significantly higher in the nurses working in intensive care units than those in the internal and surgical departments [26]. Sleep disorder is one of the most important factors in reducing the nurses’ performance، leading to mistakes in the treatment of patients and causing irreversible damage [27]. Daytime sleepiness، which is related to shift work، has an impact on critical care quality، concentration، and even occupational accidents [28]. In our study، sleep disorders of nurses working on the night shift was more than that of nurses on other shifts. One of the reasons for this result may be the working hours؛ working at nighttime can cause sleep disturbances. The exposure to various types of individual and organizational stressors can affect the nurses’ mood and sleep quality [29]. Occupational stresses, by affecting the basal ganglia level, can cause sleep disturbance and significantly affect the mental and physical health of nurses، reducing the quality of care for patients and putting them at risk. Therefore، it is necessary to take necessary measures in this field and reduce the nurses’ workload.
Conclusions
There is a significant relationship between occupational stress and sleep disorders in nurses working in the study hospital in Sari. Sleep disorders of nurses are significantly different in in terms of work shifts. Conflict with physicians is the strongest predictor of sleep disorders، while the problem with peer support is the least strong factor in predicting sleep disorders of nurses.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of Islamic Azad University, Sari branch (Code: IR.IAU.SARI.REC.1396.75).
Funding
This research received no specific grant from any funding agency in the public، commercial، or not-for-profit sectors.
Authors' contributions
Conceptualization, design, data collection: Manizhe Joulaei; Data analysis: Maryam Ghajar; Editing & review: Ehsan Abedini; Preparing initial draft: Issa Layali.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank all participants in this study for their cooperation.
References
Nurses are the largest part of the health care system such that 40% of employees in a hospital are nurses. They need to have a good quality of life to provide quality care to patients [1]. Nursing is a high-risk occupation associated with fatigue and illness [2]. Nurses suffer from significant stress due to their job requirements (workload، physical needs، time pressure، work shifs) [3]. On the other hand، based on the job demands-control pattern of Karasek (1979)، occupations that are associated with high stress and low control can cause psychological and physical distress and lead to sleep disorders and reduced quality of life [4]. Sleep disorders can damage the job and its quality and quantity، lead to a decline in nurses’ performance [5]. When the sleeping cycle is disrupted، other physiological functions of the body may also be disrupted [6]. To achieve maximum efficiency in nurses، they need to have adequate sleep [7]. The decrease in the quality of life and sleep in nurses caused by occupational stress can indirectly affect the quality and accuracy of services provided by them to patients [8]. Sleep facilitates the recovery of fatigue and is considered as an important criterion for the physical، social، and mental health [9, 10, 11, 12]. Poor sleep quality is associated with increased stress، irritability، and depression [13], and can cause medical and non-medical errors [14]. Considering the importance of nursing profession and the prevalence of sleep problems among nurses، and given the lack of sufficient study in this field، this study aims to answer to the question whether occupational stress can predict sleep disorders of nurses in Sari، Iran.
Materials and Method
This is a descriptive-analytical study. Th study population consists of 394 nurses working in Imam Khomeini Hospital in Sari city. Of these، 196 were selected as the sample using a stratified random sampling method. The sample size was determined using Krejcie & Morgan’s table. Inclusion criteria were informed consent to participate in the study and not having a mental illness. Exclusion criteria were the experience of a traumatic event and unwillingness to continue participation. For data collection، in addition to a demographic form (surveying age، sex, marital status, and educational level), two standard questionnaires including Expanded Nursing Stress Scale (ENSS) and sleep quality questionnaire were used.
Questionnaires Including Expanded Nursing Stress Scale (ENSS)
The ENSS is a revised version of the Nursing Stress Scale developed by Gray-Toft and Anderson. It was revised by French et al. to identify stressful situations not mentioned in the Nursing Stress Scale and to increase its scope [15]. This tool has 57 items and 9 subscales of death، conflict with physicians، inadequate emotional preparation، problem with peer support، problems with supervisors، workload، uncertainty about treatment، patients and families، and discrimination [16].The internal consistency is 0.96 for the overall scale, and ranges from 0.65 to 0.88 for its subscales [17]. For its Persian version, Ghiasi et al. reported a Cronbach’s alpha of 0.95 for its internal consistency [18].
The Pittsburgh sleep quality index (PSQI) was designed by Buysse et al. in 1989 to evaluate sleep quality. Its scoring is based on a four-point Likert scale from 0 to 3. The total score ranges from 0 to 21, where higher scores indicate lower sleep quality [19]. The validity and reliability of this questionnaire were confirmed in the studies by Ghaljae et al. [20] and Mahdizade et al. [21].
Data were analyzed in SPSS software, version 20. Frequency, percentage، mean، and standard deviation (SD) were used for descriptive analysis. T test (To compare sleep disorders among nurses with different work shifts)، ANOVA including Pearson correlation coefficient (To assess the effect of independent variable and its dimensions on the dependent variable) test were used for inferential analysis.
Results
Out of 196 participants, 41 (20.9%) were male and 155 (79.1%) were female. Three (1.5%) aged 21-30 years, 59 (30.0%) aged 31-40 years, 77 (39.3%) aged 41-50 years,and 57 (29.1%) aged more than 51 years. In terms of the educational level, 6 (3.1%) had diploma, 165 (84.2%) had bachelor’s degree and 25 (12.8%) had master’s degree and higher. Furthermore, 96 (49.0%) were working the morning shift, 60 (30.6%) on the evening shift، and 40 (20. 4%) on the night shift. The most of participants (42.3%) had 11-20 years of work experience (Table 1).

In examining the assumptions, the Kolmogorov-Smirnov test results showed that the distribution of data was normal, and Durbin-Watson statistic was in the range of 1.5-2.5. Therefore, the conditions for regression analysis were confirmed. As can be seen in Table 2, R value was 0.43 shows the degree of relationship between sleep quality and occupational stress.

R squared value indicated that 19% of the variation in the dependent variable was explained by the independent variable. ANOVA results showed that the regression results were significant. The beta coefficient value indicated that a one unit change in occupational stress could cause a change by 0.43 in the quality of sleep (Table 2).
The results of ANOVA showed that sleep disorders were significantly different among nurses with different work shifts (P<0.05). The sleep disorders in those working on the night shift (Mean=36.22) were higher than in those with other two work shifts (Table 3).
The beta coefficients for the domains of ENSS showed that the “conflict with physicians” with a beta value of 0. 99 was the most effective factor and the “problems with peer support” with a beta value of 0.19 was the least effective factor in predicting the sleep disorders of nurses (Table 4).

Discussion
This study showed a significant relationship between occupational stress and sleep disorders in nurses working in Imam Khomeini Hospital in Sari. In a study, Shah reported that the relationship between occupational stress and sleep quality in nurses was significant and negative [1]. Moradi showed a significant correlation between occupational stress and nurses’ fatigue in selected hospitals in Tehran [19]. Today, one of the most important types of stress in people is occupational stress, which is higher among nurses who are in contact with patients. This stress can weaken the immune system, and cause the body to be susceptible to many physical and mental illnesses [20]. In addition، occupational stress disrupts social and family interactions، and creates job dissatisfaction، increased medical errors، decreased decision-making power، and slow response time [21]. Some studies have indicated a high level of occupational stress and physical and psychological problems in nurses [22, 23]. Hospital staff، especially nurses can develop occupational stress due to the large amount of workload، lack of proper equipment in the hospital، inadequate planning، lack of time for providing adequate care for the patients، lack of information، patients’ death، lack of improvement in patient conditions، the atmosphere in the hospital، etc. This can lead to sleep disorders which have negative consequences such as fatigue and aggression [24].
Among the occupational stress domains، conflict with physicians was the strongest predictor of sleep disorders while the problems with peer support was the least strong factor in predicting sleep disorders in nurses. This is consistent with the findings of Yazdi et al. [25]. Salehi et al. investigated the quality of sleep in 176 nurses using the Pittsburgh Sleep Quality Index، and found that only 14% of nurses had a good quality of sleep؛ most of them (86%) had poor sleep quality. They showed that the quality of sleep was significantly higher in the nurses working in intensive care units than those in the internal and surgical departments [26]. Sleep disorder is one of the most important factors in reducing the nurses’ performance، leading to mistakes in the treatment of patients and causing irreversible damage [27]. Daytime sleepiness، which is related to shift work، has an impact on critical care quality، concentration، and even occupational accidents [28]. In our study، sleep disorders of nurses working on the night shift was more than that of nurses on other shifts. One of the reasons for this result may be the working hours؛ working at nighttime can cause sleep disturbances. The exposure to various types of individual and organizational stressors can affect the nurses’ mood and sleep quality [29]. Occupational stresses, by affecting the basal ganglia level, can cause sleep disturbance and significantly affect the mental and physical health of nurses، reducing the quality of care for patients and putting them at risk. Therefore، it is necessary to take necessary measures in this field and reduce the nurses’ workload.
Conclusions
There is a significant relationship between occupational stress and sleep disorders in nurses working in the study hospital in Sari. Sleep disorders of nurses are significantly different in in terms of work shifts. Conflict with physicians is the strongest predictor of sleep disorders، while the problem with peer support is the least strong factor in predicting sleep disorders of nurses.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of Islamic Azad University, Sari branch (Code: IR.IAU.SARI.REC.1396.75).
Funding
This research received no specific grant from any funding agency in the public، commercial، or not-for-profit sectors.
Authors' contributions
Conceptualization, design, data collection: Manizhe Joulaei; Data analysis: Maryam Ghajar; Editing & review: Ehsan Abedini; Preparing initial draft: Issa Layali.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank all participants in this study for their cooperation.
References
- Shah MK, Gandrakota N, Cimiotti JP, Ghose N, Moore M, Ali MK. Prevalence of and factors associated with nurse burnout in the US. JAMA Netw Open. 2021; 4(2): e2036469. [DOI: 10. 1001/jamanetworkopen. 2020. 36469] [PMID]
- Barzideh M, Choobineh A, Tabatabaei H. [Job stress dimensions and their relationship to job change intention among nurses (Persian)]. Iran J Ergon. 2013; 1(1): 33-42. [Link]
- Hojjati H, Jalal Manesh S, Fesharaki M. [Sleeplessness effect on the general health of hospitals nightshift nurses in Gorgan, Iran (Persian)]. J Gorgan Univ Med Sci. 2009; 11(3): 70-5. [Link]
- Nourian K. [The relationship between job stressors and general health of nursing staff working in educational hospitals affiliated to Isfahan University of medical sciences (Persian)]. J Fac Nurs Midwifery Paramed Sci Rafsanjan. 2010; 5(2-1). [Link]
- Bozorg Sohrabi F, Soleymani A, Habibi M, Emami Zeydi A, Nejad Gorji H, Hasanzade Kiab F. [Sleep Quality and its Related Factors in Nurses, Work in Open Heart Intensive Care Units in Mazandaran Providence: A Cross-sectional Study (Persian)]. Q J Health Breeze, 2014; 2(1):18-23. [Link]
- Caruso CC. Negative impacts of shiftwork and long work hours. Rehabil Nurs. 2014; 39(1): 16-25. [DOI: 10. 1002/rnj. 107] [PMID]
- Soleimani MA, Masoudi R, Sadeghi T, Bahrami N, Ghorbani M, Hasanpour A. [General health and its association with sleep quality in two groups of nurses with and without shift working in educational centers of Iran University of Medical Sciences (IUMS) (Persian)]. J Shahrekord Univ Med Sci. 2008; 10(3):70-5. [Link]
- Nasiry Zarrin Ghabaee D, Talebpour Amiri F, Hosseini Velshkolaei MR, Rajabzadeh R. [Quality of life and its relationship with job stress among nursing staff in hospitals of Sari (Persian)]. J Nurs Educ. 2016; 5(2):40-8. [Link]
- Hojjati H, Taheri N, Sharif Nia H. [Mental health and physical health in nurses working at night in hospitals affiliated to Golestan University of Medical Sciences (Persian)]. Nurs Midwifery J. 2010; 8(3). [Link]
- Zakerimoghadam M, Shaban M, Kazemnejad A, Ghadyani L. [Comparison of effective factors on sleeping the nurses and hospitalized patients’ viewpoints (Persian)]. J Hayat. 2006; 2(12): 5-12. [Link]
- Farhadi Nasab A, Azimi H. Study of patterns and subjective quality of sleep and their correlation with personality traits among medical students of Hamadan university of medical sciences. Avicenna J Clin Med. 2008; 15(1):11-5. [Link]
- Kara N. Effect of sleep quality on psychiatric symptoms and life quality in newspaper couriers. Noro Psikiyatr Ars. 2016; 53(2): 102-7. [PMID]
- Silva M, Chaves C, Duarte J, Amaral O, Ferreira M. Sleep quality determinants among nursing students. Procedia-Social and Behavioral Sciences. 2017; 217: 999-1007. [DOI: 10. 1016/j. sbspro. 2016. 02. 090]
- Namdar P, Etezadi T, Pourasghar M, Ghadami H, Molania T. [Evaluation of anxiety, stress, and sleep disorders in professors and students of Sari Dental School during the COVID-19 pandemic in 2021 (Persian)]. J Mash Dent Sch. 2023; 47(1): 80-9. [Link]
- French SE, Lenton R, Walters V, Eyles J. An empirical evaluation of an expanded Nursing Stress Scale. J Nurs Meas. 2000; 8(2): 161-78. [DOI: 10. 1891/1061-3749. 8. 2. 161]
- Andal EM. A Pilot Study Quantifying Filipino Nurses’ Perception of Stress. Californian J Health Promot. 2006; 4(4):88-95.[Link]
- Milutinović D, Golubović B, Brkić N, Prokeš B. Professional stress and health among critical care nurses in Serbia. Arh Hig Rada Toksikol. 2012; 63(2):171-80. [DOI:10.2478/10004-1254-63-2012-2140] [PMID]
- Ghiasi A, ghaffari M, shahabi nejad M, Soltani Poorsheikh S, barkhordar A, davari M. [A study of occupational stressors among the nurses in a military hospital. Ebnesina (Persian)]. 2017; 19(1):4-11. [Link]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
- Ghaljaei F, Naderifar M, Ghaljeh M. Comparison of general health status and sleep quality between nurses with fixed working shifts and nurses with rotating working shifts. Zahedan J Res Med Sci. 2011; 13(1):e94094. [Link]
- Mahdizadeh S, Salari MM, Ebadi A, Aslani J, Naderi Z, Aazeh A. [Relationship between sleep quality and quality of life in chemical warfare victims with bronchiolitis obliteransreferred to Baqiyatallah hospital of Tehran, Iran (Persian)]. Payesh. 2011; 10(2): 265-71. [Link]
- Moradi F. [Evaluation of the relationship between job stress, sleep quality and fatigue of nurses in selected hospitals in Tehran (Persian)] [Msc Thesis]. Tehran: Tehran University of Medical Sciences; 2013.
- Safa A, Adib Haj Bagheri M, Fazel Darbandi A. [The relationship between sleep quality and quality of life in older adults (Persian)]. Iran J Psychiatr Nurs. 2015; 3(3): 53-62. [Link]
- Dhabhar FS. Effects of stress on immune function: The good, the bad, and the beautiful. Immunol Res. 2014; 58(2-3): 193-210. [DOI: 10. 1007/s12026-014-8517-0] [PMID]
- Sarafis P, Rousaki E, Tsounis A, Malliarou M, Lahana L, Bamidis P, etc. The impact of occupational stress on nurses’ caring behaviors and their health related quality of life. BMC Nurs. 2016; 15: 56. [DOI: 10. 1186/s12912-016-0178-y] [PMID]
- Terry D, Lê Q, Nguyen U, Hoang H. Workplace health and safety issues among community nurses: A study regarding the impact on providing care to rural consumers. BMJ Open. 2015; 5(8): e008306. [DOI: 10. 1136/bmjopen-2015-008306] [PMID]
- Kayser MS, Mainwaring B, Yue Z, Sehgal A. Sleep deprivation suppresses aggression in Drosophila. Elife. 2015; 4: e07643. [DOI: 10. 7554/eLife. 07643] [PMID]
- Yazdi Z, Abbasi M, Nabatian M, Zohal MA. [Comparison of sleep disorders in working shift workers and individuals with static Shifts (Persian)]. Iran South Med J. 2013; 16(5):320-30. [Link]
- Salehi H, Amini A, Frizzy-Amiry B, Pakpour V. Evaluating the quality of sleep among nurses working at educational hospitals of Zanjan University of Medical Sciences and its related factors. Nurs Pract Today. 2017; 4(4): 164-9. [Link]
- Sadeghniiat-Haghighi K, Najafi A, Eftekhari S, Tarkhan S. Insomnia and its association with absenteeism: A cross-sectional study among Iranian nursing team. Sleep Sci. 2021; 14(4): 305-10. [DOI: 10. 5935/1984-0063. 20200106]
- Sepehrmanesh Z, Mousavi G, Saberi H, Saei R. Sleep quality and related factors among the nurses of the Hospital of Kashan University of Medical Sciences, Iran. Int Arch Health Sci. 2017; 4(1): 17-21. [Link]
- Cranage K, Foster K. Mental health nurses’ experience of challenging workplace situations: A qualitative descriptive study. Int J Ment Health Nurs. 2022; 31(3): 665-76. [DOI: 10. 1111/inm. 12986] [PMID]
Type of Study: Research |
Subject:
Psychology
Received: 2023/04/7 | Accepted: 2023/07/5 | Published: 2023/07/1
Received: 2023/04/7 | Accepted: 2023/07/5 | Published: 2023/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







