Tue, Jul 29, 2025
[Archive]
Volume 1, Issue 3 (Spring 2023)
CPR 2023, 1(3): 332-345 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Akbarfahimi N, Pouramiri M, Azimian M, Pishyareh E, Hossienzadeh S. Investigating the Relationship Between Verbal Fluency and Some Clinical Characteristics in Patients With Multiple Sclerosis. CPR 2023; 1 (3) :332-345
URL: http://cpr.mazums.ac.ir/article-1-52-en.html
URL: http://cpr.mazums.ac.ir/article-1-52-en.html
Department of Occupational Therapy, Faculty of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Full-Text [PDF 1675 kb]
(324 Downloads)
| Abstract (HTML) (1186 Views)
Full-Text: (370 Views)
Introduction
Multiple sclerosis (MS) is a chronic progressive disease of the central nervous system with lesions in the brain and spinal cord. The prevalence of this disease in Iran is 100 per 100000 [1]. MS disease includes primary progressive, secondary progressive, and relapsing-remitting [2]. This disease is associated with various disorders including sensory, movement, vision, and cognitive disorders [3, 4]. One of the cognitive disorders in patients with MS is verbal fluency disorder. Verbal fluency disorder is one of the common complaints of patients with MS, which can be seen in the form of losing a string of words in daily conversations [5]. Fluency disorder in patients with MS reduces social participation and as a result communication, emotional, and mental health problems [6]. This disorder occurs at the beginning of the disease and can be a predictor of cognitive impairment in patients with MS [7]. Some studies have shown that verbal fluency disorder is associated with the level of physical disability of people with MS, and more severe physical disability leads to weaker verbal fluency performance [7]. While in other studies, the opposite of this relationship has been reported [8]. In some studies, the type of disease has also been associated with the verbal fluency of these people, and it has been stated that patients whose type of disease is chronic-progressive have a weaker performance in verbal fluency than relapsing-remitting individuals [6, 9]. There are controversies in the studies conducted in the field of clinical factors related to verbal fluency disorders in patients with MS, which refer to factors, such as defects in the evaluation of patients based on clinical characteristics (severity of the disease, type of disease, etc.) [9]. Investigating the clinical factors affecting this cognitive field will be an effective step in increasing social participation and improving people’s quality of life. This research was conducted to examine the relationship of some clinical characteristics (type of disease, the first symptom of disease, sleep status, depression, expanded disability status score (EDSS), fatigue, and duration of disease) with verbal fluency of patients with MS using the controlled oral word association test (COWAT).
Materials and Methods
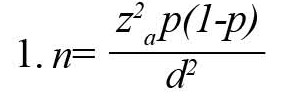
This descriptive-cross-sectional study was conducted on patients with MS referred to Rofideh Rehabilitation Hospital. According to previous studies, the prevalence of executive disfunction in patients with MS is 19%. Considering the confidence level of 0.95 and the error d=0.01 and the 10% probability of dropping, the sample size was determined 71 people by the following formula 1.
The inclusion criteria included persian native, suffering from MS according to McDonald’s criteria with the approval of a neurologist, not suffering from memory-impairing diseases, such as Alzheimer, not suffering from congenital syndromes, such as Down syndrome, not suffering from thyroid disorders, not taking drugs affecting cognition and memory such as benzodiazepine, not suffering from severe visual and movement disorders not allowing the samples to cooperate. Background information questionnaire, Pittsburgh sleep quality questionnaire (PSQI), fatigue severity scale (FSS), EDSS scale, Beck depression inventory-fast screen, and COWAT were used as data collection tools.
The questionnaire of background information included people’s specifications including age, gender, marital status, level of education, type of MS disease, duration of the disease, and the first symptom of the disease, which was designed and completed by the researcher to obtain general information from the subjects.
Pittsburgh Sleep Quality Questionnaire (PSQI) had 9 items, each of which had a score from zero to three. It included the components of sleep duration, mental quality of sleep, delay in falling asleep, sleep efficiency, sleep disorders, use of sleeping pills, and daily dysfunction, and the total score of this test was the sum of these components. A total score of 5 or more indicated poor sleep quality. The validity and reliability of this questionnaire have been confirmed by the Tehran Institute of Psychiatry. Its Cronbach alpha coefficient is reported 0.78 to 0.82 [10].
The fatigue severity scale (FSS) included 9 questions that assess only the concept of fatigue. It was scored on a Likert scale from completely disagree (1) to completely agree (7). The validity and reliability of its Persian version have been done and the value of its Cronbach alpha coefficient has been reported as 0.96 [11].
The expanded disability status score (EDSS) is a quantitative method to measure disability in MS. It ranges from 0 (normal neurological status) to 10 (death due to MS). Necessary information was extracted from patients’ files. A score of 1 to 4.5 included patients who were fully moving, and a score of 5 to 9.5 indicated impaired movement, and this classification was used in this study [12].
The Beck depression inventory-fast screen (BDI-FS) was introduced by Beck et al. in 1961. It consists of 7 questions that are graded on a Likert scale from 0 to 3. Its Cronbach alpha coefficient is 0.87 and its reliability is reported as 0.90 [13].
The verbal fluency test was evaluated by the COWAT test. In this test, the patient was asked to say several words that start with letters (m, b, and t) and with certain restrictions (no place name, no number, etc.). Its scoring was the sum of the number of words spoken in the time limit of 60 s for each letter. Arman Eshaghi et al performed its validity and reliability in Iran [14].
To investigate the simultaneous effect of independent variables (clinical characteristics) on the dependent variable (verbal fluency test), a generalized linear regression model was fitted. The result of fitting the regression model in quantitative variables is reported as the model coefficient and in qualitative variables as the result of Bonferroni’s post hoc test.
Results
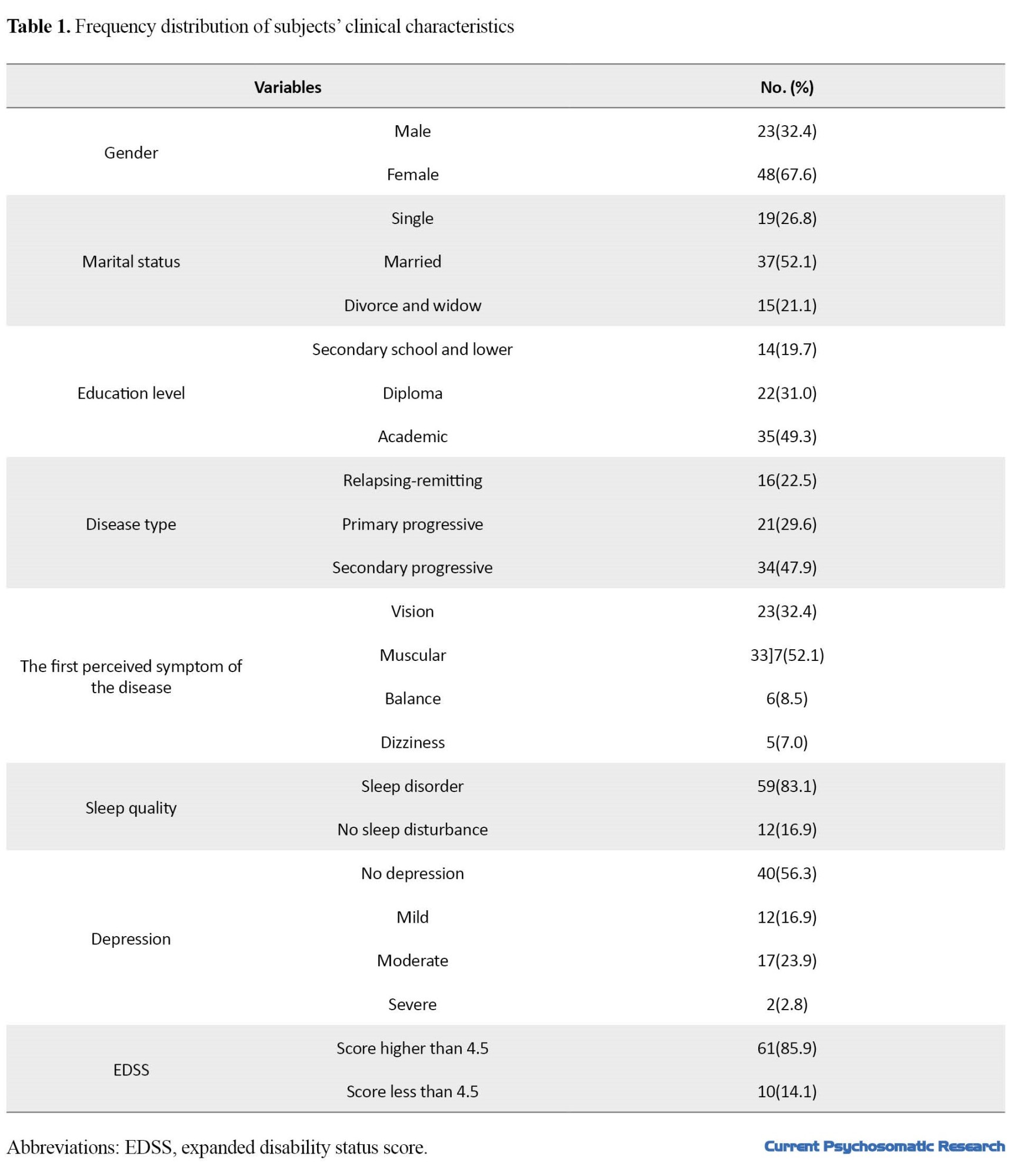
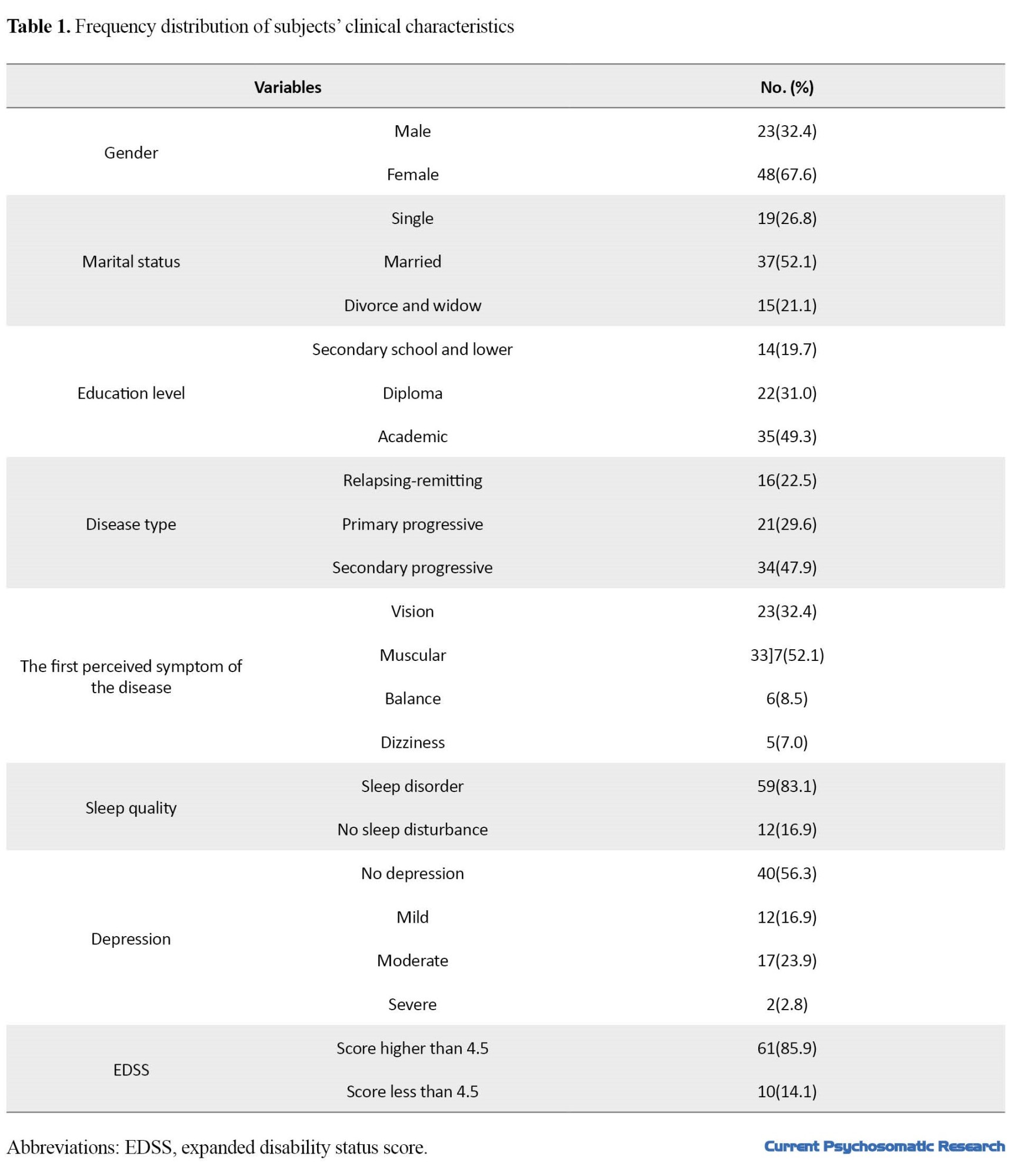
The participants of this research were 71 patients with MS (67.6% women and 32.4% men). A total of 52.1% of subjects were married and 26.8% were single. The average age of subjects in this study was 43.9±35.54 years, the average disease duration was 13.83±5.62 years, and the average fatigue score was 53.7±10.88. Table 1 presents the frequency distribution of the subjects’ clinical characteristics.
Verbal fluency was measured with the verbal fluency questionnaire among the participants, and its mean and standard deviation are 23.68 and 11.76, respectively.
Effective factors on verbal fluency were examined in Table 2.
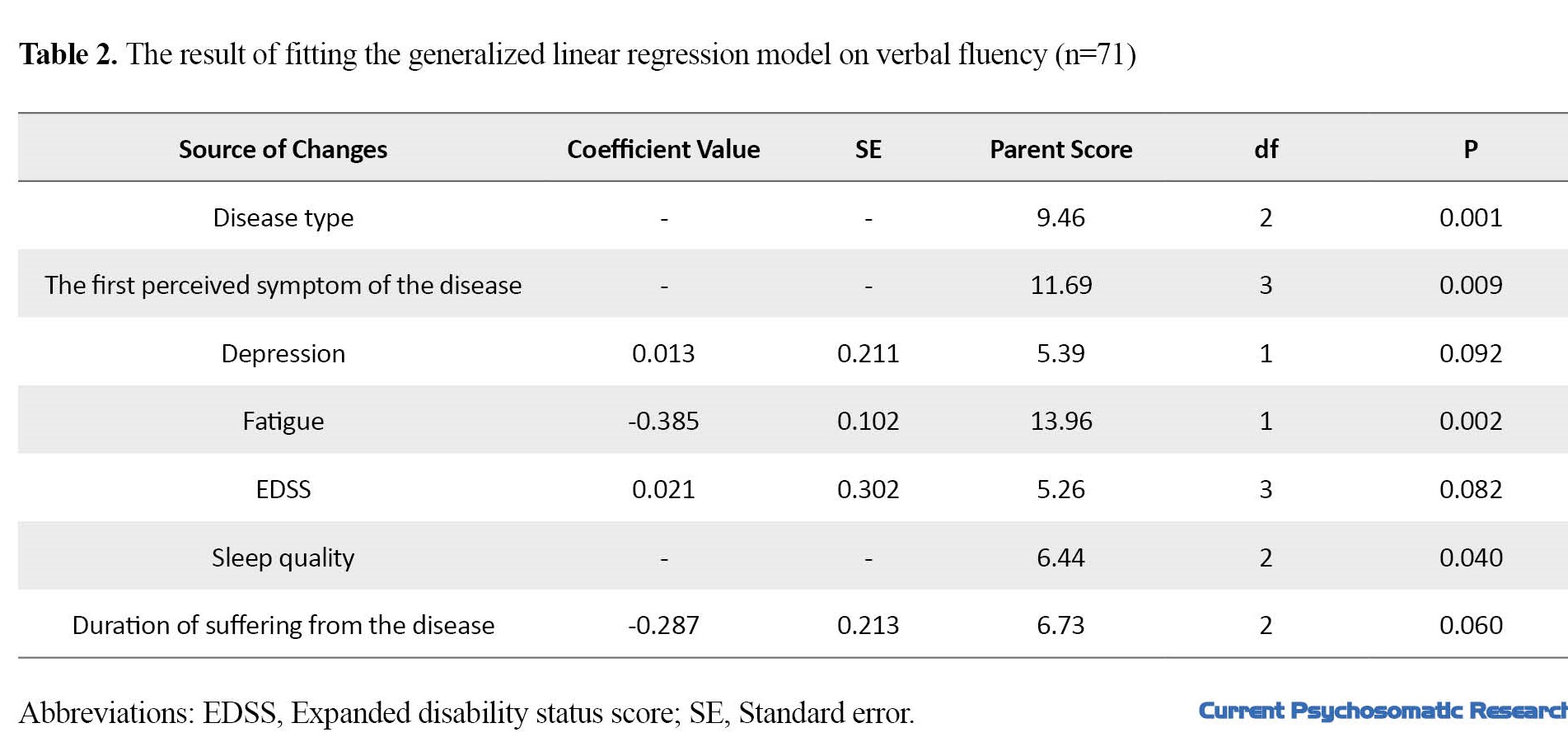
The result of the generalized linear regression model showed that the factors of disease type, the first symptom of the disease, sleep status, and fatigue have a significant relationship with the verbal fluency test (Table 2).
According to the fitted model, the probability value of the variables of depression, physical disability, and the duration of the disease was approximately 0.05, that’s why they were kept in the model. In future studies with a larger sample size, it may be possible to examine the significant relationship status of these variables with more verbal fluency. The fatigue variable shows a significant relationship (P<0.05); with an increase of one score in people’s fatigue, the average verbal fluency decreases by about 0.04. Qualitative variables of the disease type, the first symptom of the disease, and sleep status also showed a significant relationship with verbal fluency. To compare the average verbal fluency in these variables, which have more than two levels, Bonferroni’s test was used, which is generalized in linear regression (EM means comparing). The results of Bonferroni’s test showed a significant difference in the average verbal fluency score in people whose disease perception symptoms were dizziness, visual, and muscular. A significant difference was observed in the average verbal fluency score of people with moderate sleep disorders and people with severe and very severe disorders. Also, a significant difference was observed in the mean verbal fluency score in people who had a progressive type of disease (primary and secondary progressive) (Table 3).

Discussion
Verbal fluency disorder is one of the cognitive disorders in patients with MS, in which the person complains of loss of speech in daily conversations. This disorder reduces social participation and as a result, communication, emotional, and mental health problems for MS patients [6]. This study was conducted to examine the relationship between verbal fluency and some clinical characteristics of patients with MS (physical disability, type of MS disease, duration of disease, first symptom of the disease, fatigue, sleep disorders, depression) using COWAT.
In the present study, no significant relationship was found between the verbal fluency score of patients with MS with their physical disability. Among the inconsistent studies in this field, we can refer to the study of Viterbo et al., who stated that verbal fluency disorder is associated with a level of physical disability, and more severe physical disability results in poor performance in verbal fluency [7]. Talebi et al.’s study was consistent with the present study [8]. In justifying the lack of a significant relationship between physical and mental disability, we can point to the different natures of physical and cognitive scales. In the physical disability scale, not many cognitive items are considered but most physical and movement items are considered. It is also possible to point out the difference between physical and cognitive information processing in the brain. Motor brain skills are mostly processed in primary motor, premotor, and supplementary motor areas, while cognitive skills are mostly processed in the frontal and prefrontal areas.
According to the findings of this study, no significant relationship was observed between the verbal fluency score of patients with MS and the duration of the disease. The results were inconsistent with some studies conducted in this field. In these studies, it has been stated that verbal fluency disorder is associated with the duration of the disease [7, 15]. The average duration of the disease in the present study was 13 years old; this difference in the average duration of the disease in different studies can affect the significance. Also, the sample size in the present study was less than the mentioned studies; this issue can affect the significance.
In the present study, no significant relationship was found between depression and verbal fluency of patients with MS. Among the inconsistent studies in this field, we can refer to the study conducted by Bruce et al. and Julien et al. who stated that depression is effective in verbal fluency cognition of patients with MS [16, 17]. One of the factors affecting the inconsistency of the results is the use of different tools to assess depression. The Beck depression inventory-fast screen (BDI-FS) was used in the present study, which is not necessary for some studies conducted on patients with MS [18]. On the other hand, it is possible to mention the severity of depression, the previous background of depression in patients, as well as the amount of support received from the support groups of the depressed person in MS while examining the determining factors of the above-mentioned conditions.
Fatigue had a significant inverse relationship with the verbal fluency score of the subjects. This study was consistent with other studies conducted in this field, including the study conducted by Martin et al. and Krapp et al. [19, 20]. Fatigue in people with MS includes physical, cognitive, and social fatigue. Cognitive (mental) fatigue in people with MS can have a great impact on cognitive functions [19]. Fatigue is associated with changes in metabolic processes and cognitive activity may be affected by these metabolic changes. For example, fluctuation in the supply and metabolism of glucose (as the primary fuel of the brain) leads to decreased cognitive levels. On the other hand, the person’s concentration becomes difficult, when tired, and the ability to learn and remember is reduced, as a result of which people’s motivation also decreases. Decreasing motivation causes isolation of people and less use of cognitive skills and further reduction of cognition [20].
A significant difference was observed between the verbal fluency score and the sleep status of the subjects. People with moderate levels of sleep disorder had a higher mean and better performance than severe and very severe disorders in the verbal fluency test. The results of the present study were consistent with other studies conducted in this field, including the study conducted by Gurti et al., Bareilly et al., and Abi et al., who investigated the relationship between cognitive disorders and sleep in MS patients. Low quality of sleep can reduce the cognitive and psychological performance of people’s verbal fluency [21-23]. During sleep, more cholinergic projections occur between the hippocampus and the cortex, which have a direct effect on memory, verbal fluency, and other cognitive functions [24]. People with poor sleep quality can have problems in terms of memory and speed of information processing. This can be a justification for the significance of sleep and verbal fluency in this research.
In the present study, the mean of the verbal fluency test had a significant relationship with the first symptom of the disease. The first symptoms of MS, based on the patients’ self-reports, included muscle symptoms, dizziness, and balance and vision. The results showed that people whose onset of the disease was reported with visual symptoms showed poorer performance in the verbal fluency test. This issue can be due to the importance of the vision sense in people’s cognitive skills. In the studies conducted in this field, it has been stated that the vision status of MS people can affect the performance of neuropsychological tests [25, 26]. This issue can be due to occurring both cognitive and vision problems with cortex and subcortex disorders [27].
In the present study, the score of the verbal fluency test had a significant relationship with the type of disease, and people who had the progressive type of the disease (secondary and primary) gained a lower verbal fluency score than other participants in the research. The results were consistent with other studies in this field, including the study conducted by Amy et al., which stated that verbal fluency disorders are more common in the progressive type of disease [15]. In the progressive type, the disease is constantly progressing and the nervous system does not get a chance to recover; however, in the relapsing-remitting type, the possibility of plasticity of the nervous system exists among attacks. On the other hand, in many relapsing-remitting people, the disease becomes a secondary progressive type after a period, the duration of the disease is vital in the cognitive level of people.
Conclusion
The results of this study showed a significant relationship between verbal fluency and some clinical characteristics of patients with MS (fatigue, sleep status, type of disease, and the first symptom of the disease). This relationship shows that in the first diagnoses of MS, considering clinical characteristics and taking early measures such as cognitive rehabilitation and lifestyle modification are taken based on the probability of these disorders which will be an effective step in improving the quality of life of these people. One of the limitations of this research is the lack of replication with healthy people. It is suggested to examine the clinical characteristics of patients with MS who do not have verbal fluency disorder.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of the University of Rehabilitation Sciences and Social Health with code IR.USWR.REC.1396.106.
Funding
This research is derived from the secondary findings of the master’s thesis of Maryam Pouramiri in the Department of Occupational Therapy, University of Rehabilitation Sciences and Social Health.
Authors' contributions
Conceptualization and Supervision: Methodology: Nazila Akbarfahimi and Mojtaba Azimian and Ebrahim Pishyareh; Investigation, Writing–original draf and Data collection: Maryam Pouramiri; Data analysis: Samaneh Hossienzadeh; Writing– review & editing, Funding acquisition and Resource: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Hence, we thank the Clinical Research Development Unit of Rofideh Rehabilitation Hospital in Tehran City, Iran, and all those who helped us in conducting this research.
References
Multiple sclerosis (MS) is a chronic progressive disease of the central nervous system with lesions in the brain and spinal cord. The prevalence of this disease in Iran is 100 per 100000 [1]. MS disease includes primary progressive, secondary progressive, and relapsing-remitting [2]. This disease is associated with various disorders including sensory, movement, vision, and cognitive disorders [3, 4]. One of the cognitive disorders in patients with MS is verbal fluency disorder. Verbal fluency disorder is one of the common complaints of patients with MS, which can be seen in the form of losing a string of words in daily conversations [5]. Fluency disorder in patients with MS reduces social participation and as a result communication, emotional, and mental health problems [6]. This disorder occurs at the beginning of the disease and can be a predictor of cognitive impairment in patients with MS [7]. Some studies have shown that verbal fluency disorder is associated with the level of physical disability of people with MS, and more severe physical disability leads to weaker verbal fluency performance [7]. While in other studies, the opposite of this relationship has been reported [8]. In some studies, the type of disease has also been associated with the verbal fluency of these people, and it has been stated that patients whose type of disease is chronic-progressive have a weaker performance in verbal fluency than relapsing-remitting individuals [6, 9]. There are controversies in the studies conducted in the field of clinical factors related to verbal fluency disorders in patients with MS, which refer to factors, such as defects in the evaluation of patients based on clinical characteristics (severity of the disease, type of disease, etc.) [9]. Investigating the clinical factors affecting this cognitive field will be an effective step in increasing social participation and improving people’s quality of life. This research was conducted to examine the relationship of some clinical characteristics (type of disease, the first symptom of disease, sleep status, depression, expanded disability status score (EDSS), fatigue, and duration of disease) with verbal fluency of patients with MS using the controlled oral word association test (COWAT).
Materials and Methods
This descriptive-cross-sectional study was conducted on patients with MS referred to Rofideh Rehabilitation Hospital. According to previous studies, the prevalence of executive disfunction in patients with MS is 19%. Considering the confidence level of 0.95 and the error d=0.01 and the 10% probability of dropping, the sample size was determined 71 people by the following formula 1.
The inclusion criteria included persian native, suffering from MS according to McDonald’s criteria with the approval of a neurologist, not suffering from memory-impairing diseases, such as Alzheimer, not suffering from congenital syndromes, such as Down syndrome, not suffering from thyroid disorders, not taking drugs affecting cognition and memory such as benzodiazepine, not suffering from severe visual and movement disorders not allowing the samples to cooperate. Background information questionnaire, Pittsburgh sleep quality questionnaire (PSQI), fatigue severity scale (FSS), EDSS scale, Beck depression inventory-fast screen, and COWAT were used as data collection tools.
The questionnaire of background information included people’s specifications including age, gender, marital status, level of education, type of MS disease, duration of the disease, and the first symptom of the disease, which was designed and completed by the researcher to obtain general information from the subjects.
Pittsburgh Sleep Quality Questionnaire (PSQI) had 9 items, each of which had a score from zero to three. It included the components of sleep duration, mental quality of sleep, delay in falling asleep, sleep efficiency, sleep disorders, use of sleeping pills, and daily dysfunction, and the total score of this test was the sum of these components. A total score of 5 or more indicated poor sleep quality. The validity and reliability of this questionnaire have been confirmed by the Tehran Institute of Psychiatry. Its Cronbach alpha coefficient is reported 0.78 to 0.82 [10].
The fatigue severity scale (FSS) included 9 questions that assess only the concept of fatigue. It was scored on a Likert scale from completely disagree (1) to completely agree (7). The validity and reliability of its Persian version have been done and the value of its Cronbach alpha coefficient has been reported as 0.96 [11].
The expanded disability status score (EDSS) is a quantitative method to measure disability in MS. It ranges from 0 (normal neurological status) to 10 (death due to MS). Necessary information was extracted from patients’ files. A score of 1 to 4.5 included patients who were fully moving, and a score of 5 to 9.5 indicated impaired movement, and this classification was used in this study [12].
The Beck depression inventory-fast screen (BDI-FS) was introduced by Beck et al. in 1961. It consists of 7 questions that are graded on a Likert scale from 0 to 3. Its Cronbach alpha coefficient is 0.87 and its reliability is reported as 0.90 [13].
The verbal fluency test was evaluated by the COWAT test. In this test, the patient was asked to say several words that start with letters (m, b, and t) and with certain restrictions (no place name, no number, etc.). Its scoring was the sum of the number of words spoken in the time limit of 60 s for each letter. Arman Eshaghi et al performed its validity and reliability in Iran [14].
To investigate the simultaneous effect of independent variables (clinical characteristics) on the dependent variable (verbal fluency test), a generalized linear regression model was fitted. The result of fitting the regression model in quantitative variables is reported as the model coefficient and in qualitative variables as the result of Bonferroni’s post hoc test.
Results
The participants of this research were 71 patients with MS (67.6% women and 32.4% men). A total of 52.1% of subjects were married and 26.8% were single. The average age of subjects in this study was 43.9±35.54 years, the average disease duration was 13.83±5.62 years, and the average fatigue score was 53.7±10.88. Table 1 presents the frequency distribution of the subjects’ clinical characteristics.
Verbal fluency was measured with the verbal fluency questionnaire among the participants, and its mean and standard deviation are 23.68 and 11.76, respectively.
Effective factors on verbal fluency were examined in Table 2.
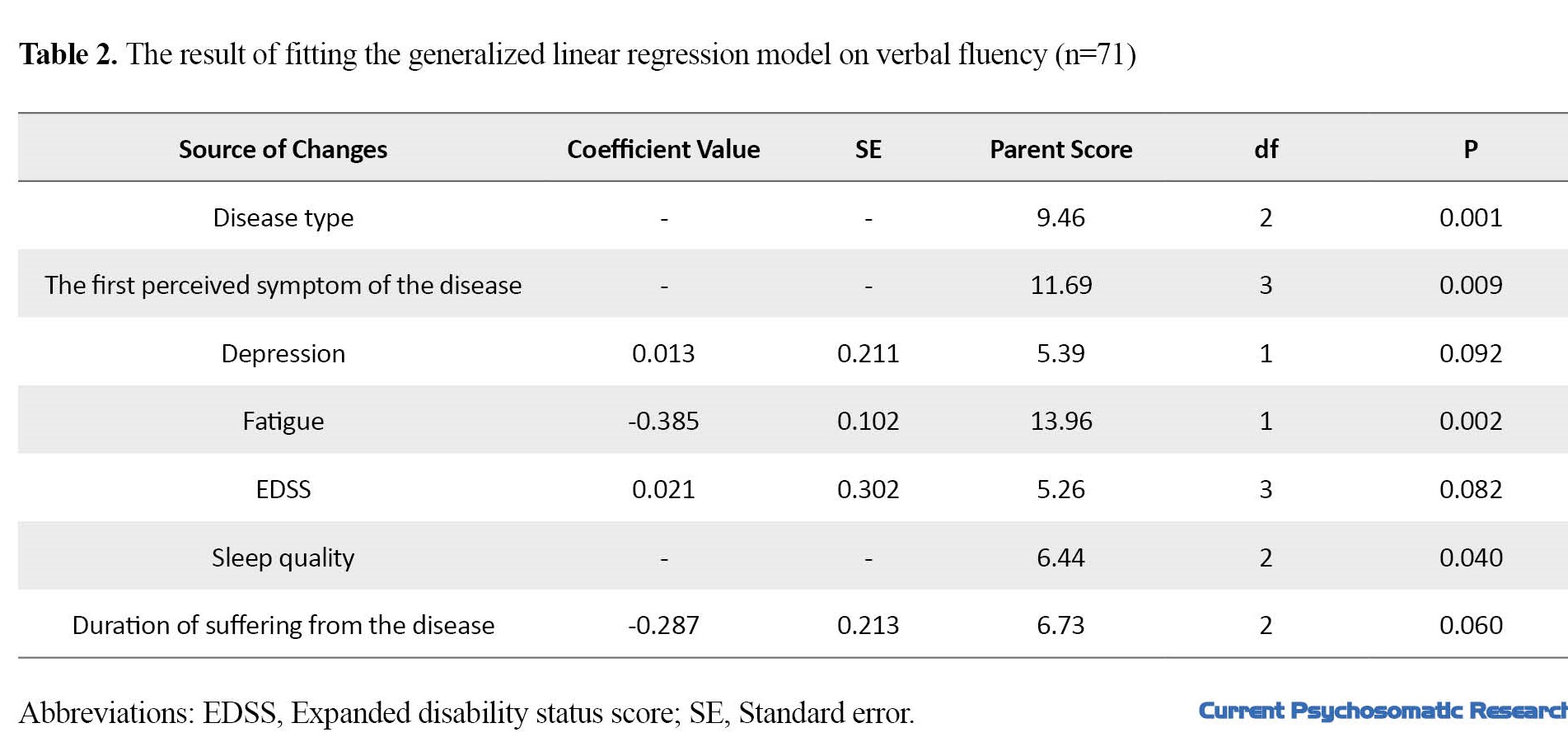
The result of the generalized linear regression model showed that the factors of disease type, the first symptom of the disease, sleep status, and fatigue have a significant relationship with the verbal fluency test (Table 2).
According to the fitted model, the probability value of the variables of depression, physical disability, and the duration of the disease was approximately 0.05, that’s why they were kept in the model. In future studies with a larger sample size, it may be possible to examine the significant relationship status of these variables with more verbal fluency. The fatigue variable shows a significant relationship (P<0.05); with an increase of one score in people’s fatigue, the average verbal fluency decreases by about 0.04. Qualitative variables of the disease type, the first symptom of the disease, and sleep status also showed a significant relationship with verbal fluency. To compare the average verbal fluency in these variables, which have more than two levels, Bonferroni’s test was used, which is generalized in linear regression (EM means comparing). The results of Bonferroni’s test showed a significant difference in the average verbal fluency score in people whose disease perception symptoms were dizziness, visual, and muscular. A significant difference was observed in the average verbal fluency score of people with moderate sleep disorders and people with severe and very severe disorders. Also, a significant difference was observed in the mean verbal fluency score in people who had a progressive type of disease (primary and secondary progressive) (Table 3).

Discussion
Verbal fluency disorder is one of the cognitive disorders in patients with MS, in which the person complains of loss of speech in daily conversations. This disorder reduces social participation and as a result, communication, emotional, and mental health problems for MS patients [6]. This study was conducted to examine the relationship between verbal fluency and some clinical characteristics of patients with MS (physical disability, type of MS disease, duration of disease, first symptom of the disease, fatigue, sleep disorders, depression) using COWAT.
In the present study, no significant relationship was found between the verbal fluency score of patients with MS with their physical disability. Among the inconsistent studies in this field, we can refer to the study of Viterbo et al., who stated that verbal fluency disorder is associated with a level of physical disability, and more severe physical disability results in poor performance in verbal fluency [7]. Talebi et al.’s study was consistent with the present study [8]. In justifying the lack of a significant relationship between physical and mental disability, we can point to the different natures of physical and cognitive scales. In the physical disability scale, not many cognitive items are considered but most physical and movement items are considered. It is also possible to point out the difference between physical and cognitive information processing in the brain. Motor brain skills are mostly processed in primary motor, premotor, and supplementary motor areas, while cognitive skills are mostly processed in the frontal and prefrontal areas.
According to the findings of this study, no significant relationship was observed between the verbal fluency score of patients with MS and the duration of the disease. The results were inconsistent with some studies conducted in this field. In these studies, it has been stated that verbal fluency disorder is associated with the duration of the disease [7, 15]. The average duration of the disease in the present study was 13 years old; this difference in the average duration of the disease in different studies can affect the significance. Also, the sample size in the present study was less than the mentioned studies; this issue can affect the significance.
In the present study, no significant relationship was found between depression and verbal fluency of patients with MS. Among the inconsistent studies in this field, we can refer to the study conducted by Bruce et al. and Julien et al. who stated that depression is effective in verbal fluency cognition of patients with MS [16, 17]. One of the factors affecting the inconsistency of the results is the use of different tools to assess depression. The Beck depression inventory-fast screen (BDI-FS) was used in the present study, which is not necessary for some studies conducted on patients with MS [18]. On the other hand, it is possible to mention the severity of depression, the previous background of depression in patients, as well as the amount of support received from the support groups of the depressed person in MS while examining the determining factors of the above-mentioned conditions.
Fatigue had a significant inverse relationship with the verbal fluency score of the subjects. This study was consistent with other studies conducted in this field, including the study conducted by Martin et al. and Krapp et al. [19, 20]. Fatigue in people with MS includes physical, cognitive, and social fatigue. Cognitive (mental) fatigue in people with MS can have a great impact on cognitive functions [19]. Fatigue is associated with changes in metabolic processes and cognitive activity may be affected by these metabolic changes. For example, fluctuation in the supply and metabolism of glucose (as the primary fuel of the brain) leads to decreased cognitive levels. On the other hand, the person’s concentration becomes difficult, when tired, and the ability to learn and remember is reduced, as a result of which people’s motivation also decreases. Decreasing motivation causes isolation of people and less use of cognitive skills and further reduction of cognition [20].
A significant difference was observed between the verbal fluency score and the sleep status of the subjects. People with moderate levels of sleep disorder had a higher mean and better performance than severe and very severe disorders in the verbal fluency test. The results of the present study were consistent with other studies conducted in this field, including the study conducted by Gurti et al., Bareilly et al., and Abi et al., who investigated the relationship between cognitive disorders and sleep in MS patients. Low quality of sleep can reduce the cognitive and psychological performance of people’s verbal fluency [21-23]. During sleep, more cholinergic projections occur between the hippocampus and the cortex, which have a direct effect on memory, verbal fluency, and other cognitive functions [24]. People with poor sleep quality can have problems in terms of memory and speed of information processing. This can be a justification for the significance of sleep and verbal fluency in this research.
In the present study, the mean of the verbal fluency test had a significant relationship with the first symptom of the disease. The first symptoms of MS, based on the patients’ self-reports, included muscle symptoms, dizziness, and balance and vision. The results showed that people whose onset of the disease was reported with visual symptoms showed poorer performance in the verbal fluency test. This issue can be due to the importance of the vision sense in people’s cognitive skills. In the studies conducted in this field, it has been stated that the vision status of MS people can affect the performance of neuropsychological tests [25, 26]. This issue can be due to occurring both cognitive and vision problems with cortex and subcortex disorders [27].
In the present study, the score of the verbal fluency test had a significant relationship with the type of disease, and people who had the progressive type of the disease (secondary and primary) gained a lower verbal fluency score than other participants in the research. The results were consistent with other studies in this field, including the study conducted by Amy et al., which stated that verbal fluency disorders are more common in the progressive type of disease [15]. In the progressive type, the disease is constantly progressing and the nervous system does not get a chance to recover; however, in the relapsing-remitting type, the possibility of plasticity of the nervous system exists among attacks. On the other hand, in many relapsing-remitting people, the disease becomes a secondary progressive type after a period, the duration of the disease is vital in the cognitive level of people.
Conclusion
The results of this study showed a significant relationship between verbal fluency and some clinical characteristics of patients with MS (fatigue, sleep status, type of disease, and the first symptom of the disease). This relationship shows that in the first diagnoses of MS, considering clinical characteristics and taking early measures such as cognitive rehabilitation and lifestyle modification are taken based on the probability of these disorders which will be an effective step in improving the quality of life of these people. One of the limitations of this research is the lack of replication with healthy people. It is suggested to examine the clinical characteristics of patients with MS who do not have verbal fluency disorder.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of the University of Rehabilitation Sciences and Social Health with code IR.USWR.REC.1396.106.
Funding
This research is derived from the secondary findings of the master’s thesis of Maryam Pouramiri in the Department of Occupational Therapy, University of Rehabilitation Sciences and Social Health.
Authors' contributions
Conceptualization and Supervision: Methodology: Nazila Akbarfahimi and Mojtaba Azimian and Ebrahim Pishyareh; Investigation, Writing–original draf and Data collection: Maryam Pouramiri; Data analysis: Samaneh Hossienzadeh; Writing– review & editing, Funding acquisition and Resource: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Hence, we thank the Clinical Research Development Unit of Rofideh Rehabilitation Hospital in Tehran City, Iran, and all those who helped us in conducting this research.
References
- Mirmosayyeb O, Shaygannejad V, Bagherieh S, Hosseinabadi AM, Ghajarzadeh M. Prevalence of multiple sclerosis (MS) in Iran: A systematic review and meta-analysis. Neurol Sci. 2022; 43(1):233-41. [DOI:10.1007/s10072-021-05750-w] [PMID]
- Górska E, Tylicka M, Hermanowicz A, Matuszczak E, Sankiewicz A, Gorodkiewicz E, et al. UCHL1, besides leptin and fibronectin, also could be a sensitive marker of the relapsing-remitting type of multiple sclerosis. Sci Rep. 2023; 13(1):3423. [DOI:10.1038/s41598-023-30237-3] [PMID]
- Shiri V, Emami M, Shiri E. [Investigating the relationship between selective attention and cognitive flexibility with balance in patients with relapsing-remitting multiple sclerosis (Persian)]. Arch Rehabil. 2018; 18(4):296-305. [DOI:10.21859/jrehab.18.4.4]
- Pakniya N, Bahmani B, Dadkhah A, Azimian M, Naghiyaee M, Masudi SR. Effectiveness of cognitive existential approach on decreasing demoralization in women with multiple sclerosis. 2015; 13(4):28-33. [Link]
- Matotek K, Saling MM, Gates P, Sedal L. Subjective complaints, verbal fluency, and working memory in mild multiple sclerosis. Appl Neuropsychol. 2001; 8(4):204-10. [DOI:10.1207/S15324826AN0804_2] [PMID]
- Farazi M, Azimian M, Hosseinzadeh S, Amrevani M, Faraji S, Fazeli M. A study on verbal fluency of Persian Patients with three types of multiple sclerosis. Shiraz E-Med J. 2021; 22(6):e103903. [DOI:10.5812/semj.103903]
- Viterbo RG, Iaffaldano P, Trojano M. Verbal fluency deficits in clinically isolated syndrome suggestive of multiple sclerosis. J Neurol Sci. 2013; 330(1-2):56-60. [DOI:10.1016/j.jns.2013.04.004] [PMID]
- Talebi M, Sadigh-Eteghad S, Talebi M, Naseri A, Zafarani F. Predominant domains and associated demographic and clinical characteristics in multiple sclerosis-related cognitive impairment in mildly disabled patients. Egypt J Neurol Psychiatry Neurosurg 2022; 58(1):1-8. [DOI:10.1186/s41983-022-00485-7]
- Friend KB, Rabin BM, Groninger L, Deluty RH, Bever C, Grattan L. Language functions in patients with multiple sclerosis. Clin Neuropsychol. 1999; 13(1):78-94. [DOI:10.1076/clin.13.1.78.1979] [PMID]
- Khajavi D, Khanmohamadi R. The Effect of "Green Exercise" on improving the sleep quality of female elderly without regular physical activity in arak city. J Woman Fam Studies. 2016; 3(2):7-32. [DOI:10.22051/jwfs.2016.2206]
- Shahvaroughi-Farahani A, A'zimiyan M, Fallah-Pour M, Karimlou M. Fatigue Severity Scale (FSS): Evaluation of reliability of the persian version among persons with multiple sclerosis. jrehab 2010; 10(4). [Link]
- Goodkin DE, Cookfair D, Wende K, Bourdette D, Pullicino P, Scherokman B, et al. Inter-and intrarater scoring agreement using grades 1.0 to 3.5 of the Kurtzke Expanded Disability Status Scale (EDSS). Multiple Sclerosis Collaborative Research Group. Neurology. 1992; 42(4):859-63. [DOI:10.1212/WNL.42.4.859] [PMID]
- Scogin F, Beutler L, Corbishley A, Hamblin D. Reliability and validity of the short form Beck Depression Inventory with older adults. J Clin Psychol. 1988; 44(6):853-7. [DOI:10.1002/1097-4679(198811)44:63.0.CO;2-7] [PMID]
- Eshaghi A, Riyahi-Alam S, Roostaei T, Haeri G, Aghsaei A, Aidi MR, et al. Validity and reliability of a Persian translation of the Minimal Assessment of Cognitive Function in Multiple Sclerosis (MACFIMS). Clin Neuropsychol. 2012; 26(6):975-84. [DOI:10.1080/13854046.2012.694912] [PMID]
- Lebkuecher AL, Chiaravalloti ND, Strober LB. The role of language ability in verbal fluency of individuals with multiple sclerosis. Mult Scler Relat Disord. 2021; 50:102846. [DOI:10.1016/j.msard.2021.102846] [PMID]
- Julian L, Merluzzi NM, Mohr DC. The relationship among depression, subjective cognitive impairment, and neuropsychological performance in multiple sclerosis. Mult Scler. 2007; 13(1):81-6. [DOI:10.1177/1352458506070255] [PMID]
- Diamond BJ, Johnson SK, Kaufman M, Graves L. Relationships between information processing, depression, fatigue and cognition in multiple sclerosis. Arch Clin Neuropsychol. 2008; 23(2):189-99. [DOI:10.1016/j.acn.2007.10.002] [PMID]
- Raghibi M. Comparing the cognitive function in multiple sclerosis patients. Zahedan J Res Med Sci. 2012; 14(2):e93580. [Link]
- Sjøgård M, Wens V, Van Schependom J, Costers L, D'hooghe M, D'haeseleer M, et al. Brain dysconnectivity relates to disability and cognitive impairment in multiple sclerosis. Hum Brain Mapp. 2021; 42(3):626-43. [DOI:10.1002/hbm.25247] [PMID]
- Krupp LB, Elkins LE. Fatigue and declines in cognitive functioning in multiple sclerosis. Neurology. 2000; 55(7):934-9. [DOI:10.1212/WNL.55.7.934] [PMID]
- Braley TJ, Kratz AL, Kaplish N, Chervin RD. Sleep and cognitive function in multiple sclerosis. Sleep. 2016; 39(8):1525-33. [DOI:10.5665/sleep.6012] [PMID]
- Hughes AJ, Dunn KM, Chaffee T. Sleep disturbance and cognitive dysfunction in multiple sclerosis: A systematic review. Curr Neurol Neurosci Rep. 2018; 18(1):2. [DOI:10.1007/s11910-018-0809-7] [PMID]
- Ghezzi A, Goretti B, Portaccio E, Roscio M, Amato MP. Cognitive impairment in pediatric multiple sclerosis. Neurol Sci. 2010; 31(Suppl 2):S215-8. [DOI:10.1007/s10072-010-0437-8] [PMID]
- Naseri A, Ahahdi H, Ashayeri H, Jameie SB, Farokhi NA. [Study of the effects of short-term REM sleep deprivation on neurogenesis and spatial memory of adult male rats (Persian)]. Razi J Med Sci. 2014; 21(126):95-106. [Link]
- Feaster HT, Bruce JM. Visual acuity is associated with performance on visual and non-visual neuropsychological tests in multiple sclerosis. Clin Neuropsychol. 2011; 25(4):640-51. [DOI:10.1080/13854046.2011.565075] [PMID]
- Bruce JM, Bruce AS, Arnett PA. Mild visual acuity disturbances are associated with performance on tests of complex visual attention in MS. J Int Neuropsychol Soc. 2007; 13(3):544-8. [DOI:10.1017/S1355617707070658] [PMID]
Type of Study: Research |
Subject:
Psychology
Received: 2023/02/8 | Accepted: 2023/07/1 | Published: 2023/07/1
Received: 2023/02/8 | Accepted: 2023/07/1 | Published: 2023/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |