Fri, May 23, 2025
[Archive]
Volume 1, Issue 2 (Winter 2023)
CPR 2023, 1(2): 130-141 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alizadeh Z, Araghian F, Jafari H. Investigating the Dignity of Patients Under Palliative Care and Affecting Factors on Patients: A Narrative Review. CPR 2023; 1 (2) :130-141
URL: http://cpr.mazums.ac.ir/article-1-47-en.html
URL: http://cpr.mazums.ac.ir/article-1-47-en.html
Traditional and Complementary Medicine Research Center, Addiction Institute, Mazandaran University of Medical Sciences, Sari, Iran.
Full-Text [PDF 2043 kb]
(626 Downloads)
| Abstract (HTML) (1644 Views)
Full-Text: (430 Views)
Introduction
Palliative care is patient- and family-centered care and is used to predict, prevent, and treat pain, dyspnea, and other distressing symptoms at the end of life when other treatments are ineffective [1]. Palliative care in intensive care units is a debatable issue, however, its use in treatment is increasing. It preserves the function of vital organs and reduces mortality while preventing advanced diseases [2]. Also, palliative care focuses on problems, including physical, psychological, and spiritual distress symptoms along with communication abilities and decision-making power, which reduce the responsibility of caregivers [3]. Palliative care is an approach to care for patients with critical and malignant diseases and their families, which aims to reduce suffering through the management of medical symptoms, psychosocial issues, spiritual care, and determining care goals [4]. Also, palliative care is focused on improving the quality of life of patients with acute diseases, including patients admitted to the intensive care unit. In addition, complex symptoms can be managed by providing timely advice by a specialist palliative care team [5]. A key goal in palliative care is to preserve the dignity of patients in end-of-life care [6]. Dignity is a crucial issue in the matter of care so dignity is a source of values that are expressed absolutely and relatively. Flexibility in maintaining them is influenced by culture [7]. According to the International Council of Nurses, nurses have a vital role in maintaining the dignity of patients, and this is a legal and ethical duty to care for patients as much as possible. These 4 basic responsibilities include promoting health, preventing disease, restoring health, and reducing pain [8]. Dignity therapy is a type of psychotherapy to relieve the mental and physical distress of patients in end-of-life care, and evidence suggests that dignity therapy is very effective. In a randomized clinical trial on patients with high levels of psychological distress, the effectiveness of dignity therapy on the level of anxiety and depression was shown [9]. Dignity is a crucial principle in palliative care for patients and their families so a review of various studies in this field demonstrates various factors that play a role in preserving the dignity of patients in palliative care [10]. Life and death with dignity are fundamental values in palliative care for both patients and family members [11]. A review study shows that various factors, including individual or internal factors and external factors, play a role in maintaining the dignity of patients in palliative care [12]. A study shows that supporting patients with palliative care needs is a crucial part of nursing care [13], and for a person who is critically ill and weak in the intensive care unit, dignity gives them the ability to live according to standards and values [14]. Among the effective factors to preserve the dignity of patients is attention to care factors, such as pain management, shortness of breath management, preparation of patients for end-of-life care, promotion of participation in decision-making, and meeting the needs of patients [15]. Maintaining patients’ dignity is paying attention to communication factors, including establishing communication, dealing with respect, building trust, maintaining dignity and privacy, paying enough attention to the feelings and attitudes of the patient’s family members, and respecting the individual [16]. Considering the importance of preserving the dignity of patients in palliative care and end-of-life care, especially in patients with incurable and malignant diseases, this study aims to examine the dignity of patients under palliative care and the affecting factors on patients.
Materials and Methods
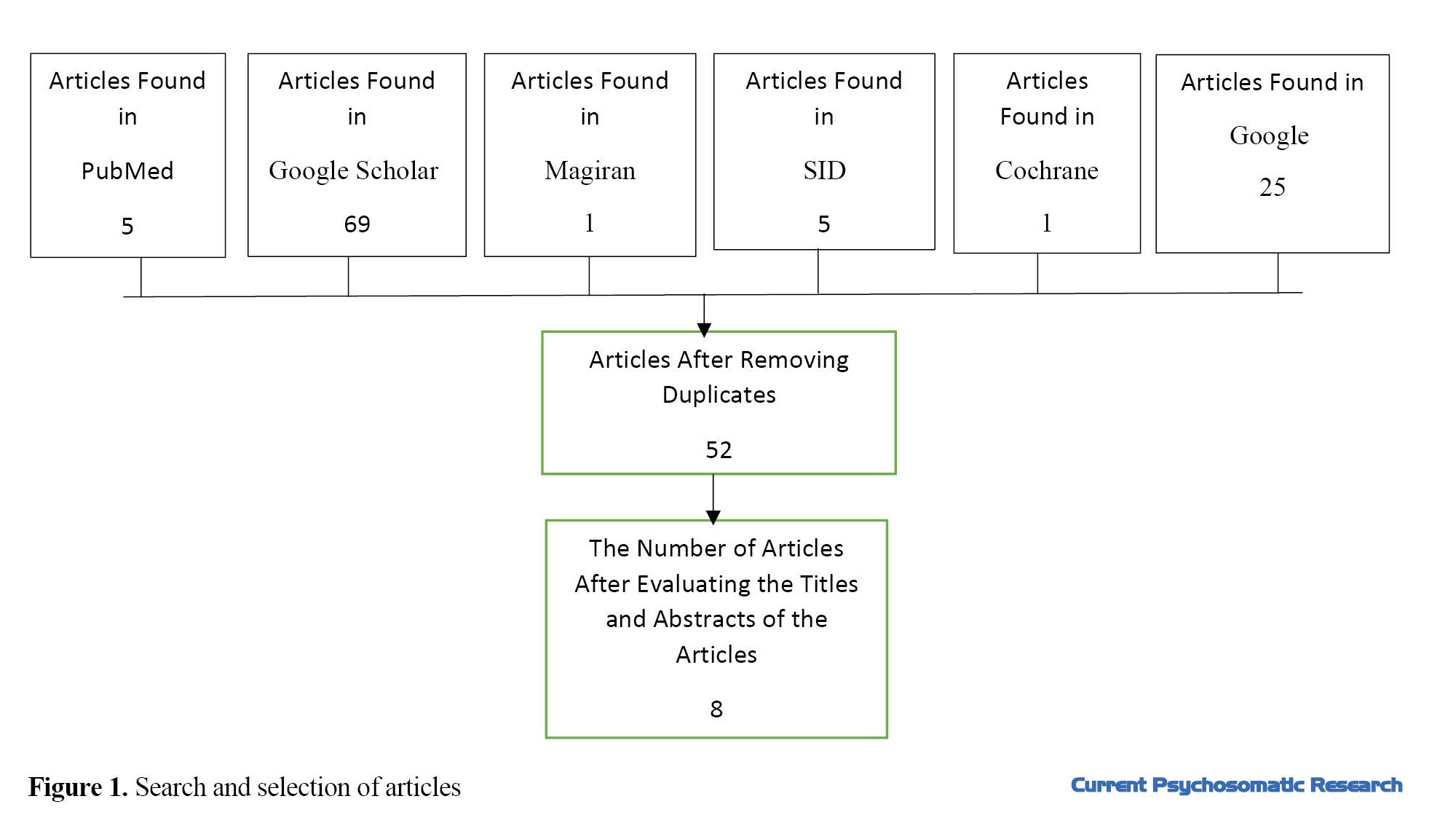
This study was conducted as a narrative review. In the present study, Persian studies were searched in Persian language databases, such as Scientific Information Database (SID) and Magirane with the keywords, dignity of patients, nurse, and palliative care from April 2012 to May 2022. To search for studies in English, the keywords of patient dignity, nurses, and palliative care were used in PubMed and Cochrane databases from June 2010 to May 2022. Also, the search was done in the Google Scholar database in Farsi and English. A manual search was performed on Google as well. The inclusion criterion was complete articles in Farsi and English. The exclusion criterion was the lack of access to the full article. Meanwhile, review articles were excluded from the study. After searching the databases, 106 articles were included in the study. By applying the inclusion and exclusion criteria and removing duplicates, the researchers examined 8 articles (Figure 1).
Results
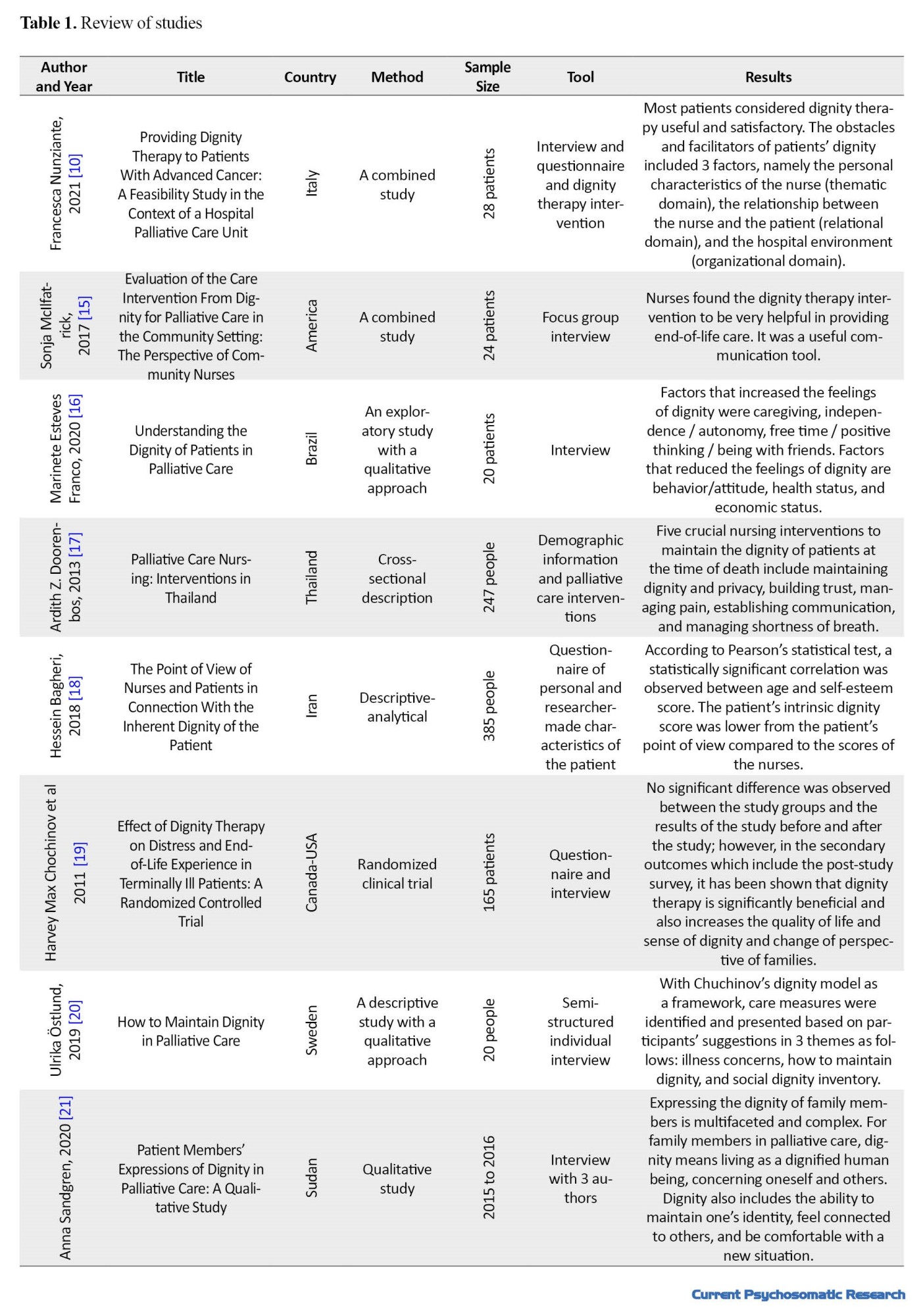
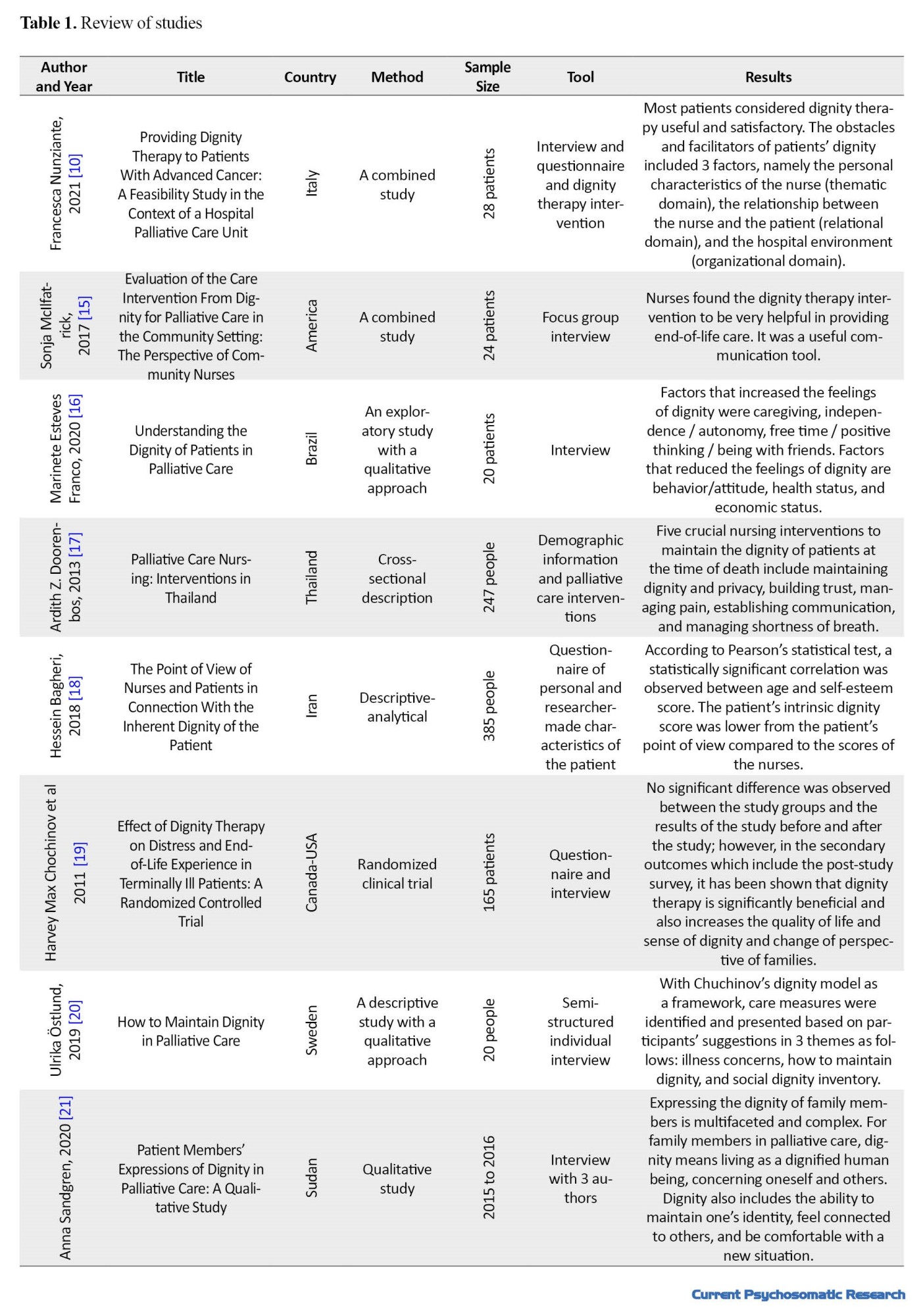
The results of the study showed that out of 8 studies, 1 study was conducted in Iran. In addition, 5 of the reviewed articles were qualitative studies (Table 1).
Discussion
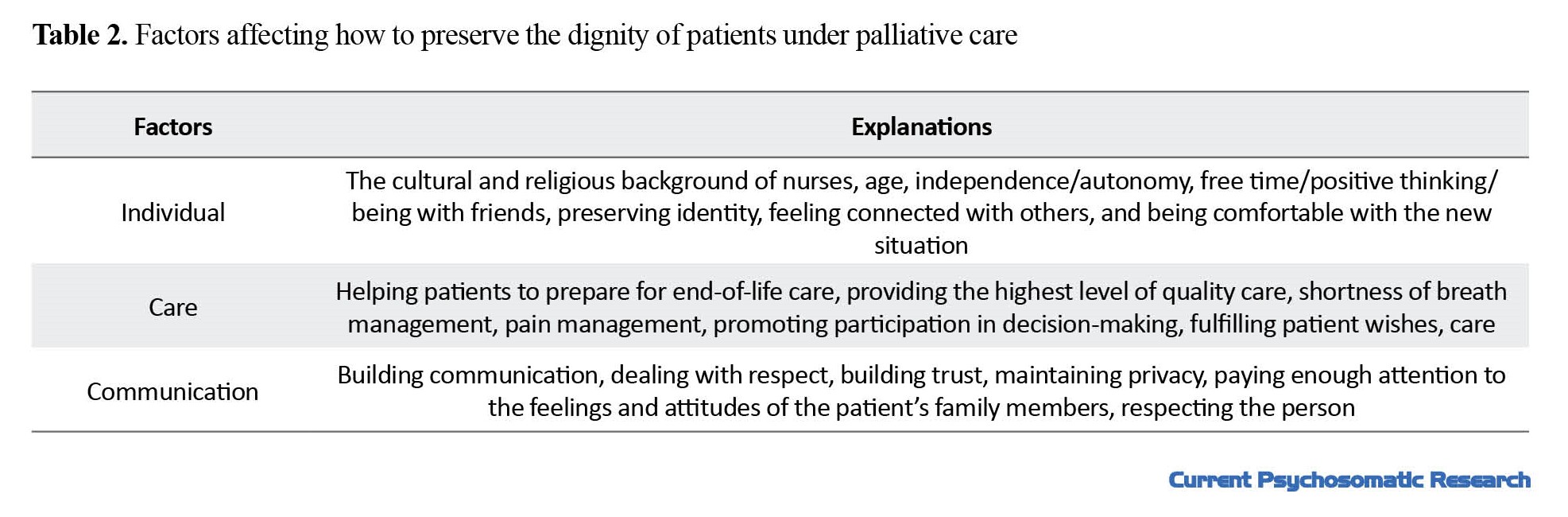
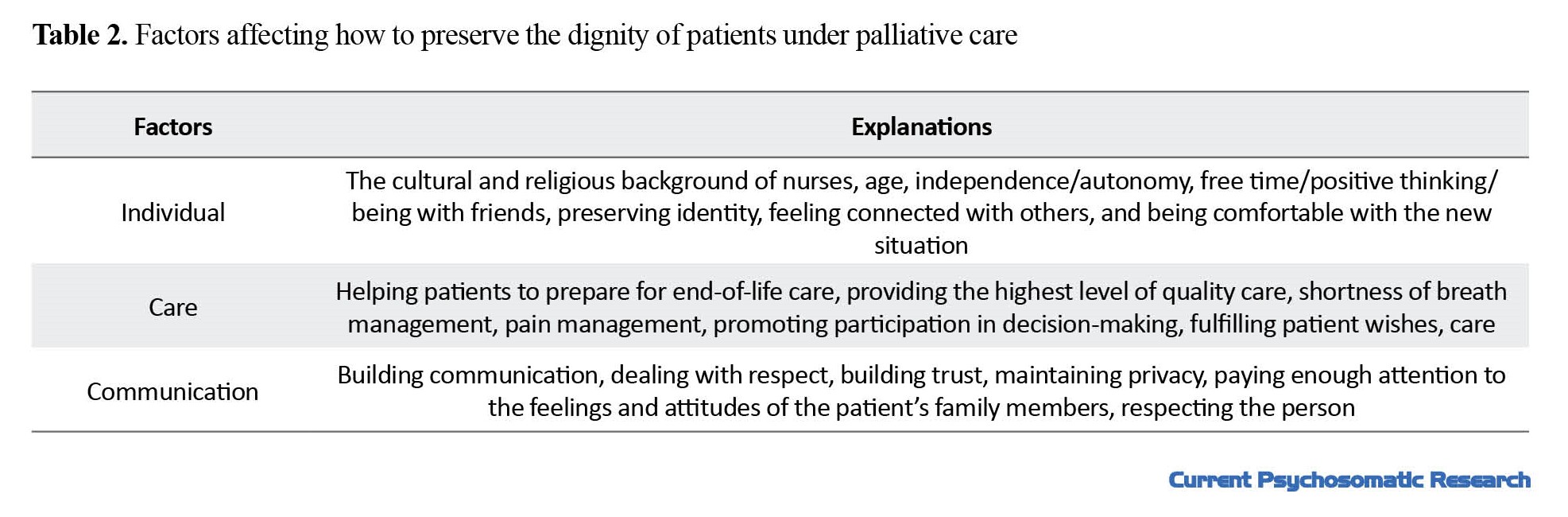
This narrative review was conducted to examine the dignity of patients under palliative care and the affecting factors on patients. The findings showed that individual, care, and communication factors are critical in maintaining the dignity of patients under palliative care (Table 2). This article was conducted to review the articles from 2010 to 2022 in Persian and English databases with the keywords dignity of patients and palliative care. The review of numerous articles in this field shows that several factors are involved in maintaining the dignity of patients in palliative care. Meanwhile, the word dignity has several meanings at any point in time. Among the factors affecting the preservation of the dignity of patients under palliative care are individual factors (nurses’ cultural and religious background, age, independence/autonomy, free time/positive thinking/being with friends, maintaining identity, feeling connected with others, and being comfortable with the new situation).
Barroso et al. concluded that the cultural and religious background of nurses is effective in understanding the meaning of dignity [22]. In a study by Harvey et al., it was shown that age has a significant impact on understanding and maintaining dignity so it is different in the elderly when compared to younger people [19]. In various studies, it has been shown that various factors, such as self-confidence, interpersonal relationships, especially with friends, family members, and health care providers, and a sense of independence and self-determination are among the vital factors that increase the feeling of dignity. Also, this issue at the time of death is effective for the patient and the patient’s family members [23, 24]. Considering the different aspects of human beings, including psychological, social, and spiritual, one of the vital factors that have been shown in studies is that interaction and communication with healthcare providers and the medical team are effective in increasing or decreasing the patient’s understanding from dignity [25]. One of the crucial skills in increasing the dignity of patients is to allow them to make decisions, especially in patients with a high level of consciousness; accordingly, various studies show that because of the progress of virtual spaces and better access to patients and their families to the sites to diagnose diseases and signs and symptoms, they can intervene in matters related to patients [26]. Hence, the role of healthcare providers in delivering information to patients in the field of disease and ensuring them regarding the maintenance of their independence is still challenging [27]. On the other hand, if the independence of patients in doing daily tasks is ignored, the dignity of patients in the matter of care reduces [28]. One of the vital aspects in increasing the dignity of patients is their relationship with healthcare providers, which increases the sense of independence and improves end-of-life care [29]. Among the factors affecting the preservation of the dignity of patients under palliative care, and care factors (helping patients to prepare for end-of-life care, providing the highest level of care quality, management of shortness of breath, pain management, promoting participation in decision-making, fulfilling patient’s wishes, and care). In addition, 5 crucial interventions of nurses and healthcare workers in the field of increasing the sense of dignity, maintaining the sense of dignity and privacy, creating a sense of trust, managing pain and shortness of breath, and promoting participation in decision-making, various studies in this field show that this is achieved when nurses create a sense of trust in patients and pay special attention to their care needs, especially in end-of-life care, while answering patients’ open questions increases patients’ sense of comfort [30]. A study conducted on cancer patients at the end of life shows that cares, such as pain and shortness of breath management and the prescription of painkillers and their support are among crucial interventions in the treatment of incurable patients and care of the end-of-life [10]. Other factors affecting the preservation of the dignity of patients under palliative care are communication factors (establishing communication, dealing with respect, building trust, preserving dignity and privacy, paying enough attention to the feelings and attitudes of the patient’s family members, and respecting the person). Establishing communication between patients and healthcare providers and their families increases the sense of self-confidence and dignity of patients in end-of-life and palliative care [31]. Also, a study has shown that communication along with participation in patients’ decision-making and family members in the treatment process is not worrying and practical in the palliative care needs of patients [32]. Palliative care is a solution that improves the quality of life of the patient and his family in facing the problems related to the disease by preventing the suffering of the patient and improving the symptoms and other physical, psychological, spiritual, and social problems of the patient. This care begins with the diagnosis of the disease and continues throughout the disease [33]. Respecting the dignity of people is a crucial issue to increase their satisfaction with the services provided by the staff, followed by the establishment of a favorable relationship between patients and nurses and a sense of security and privacy to reduce the length of stay of patients in the hospital and reduce costs. Therefore, it is necessary that the treatment team, especially nurses, become more familiar with the concept of human dignity and pay attention to it in care [18].
Conclusion
According to the review of numerous review articles in the field of dignity, human dignity, and palliative care along with the study results, nurses, as vital members in caring for patients, especially incurable patients and in end-of-life care and need of palliative care, should consider maintaining dignity and human dignity as their duty and perform their professional duties deservedly according to the factors affecting the creation and preservation of human dignity. According to the results of the studies and investigating the effective factors in maintaining human dignity and the effect of dignity therapy, the results of such research can be used to improve the care of patients with incurable diseases who need palliative care and to create trust and proper communication with patients and their families. Since the perception of dignity is a dynamic process and is different and changing during different times and lifetimes, it is suggested that more studies be conducted to investigate this issue from other perspectives, such as health professionals and relatives. Healthcare planning should consider the factors that increase the sense of dignity and should consider creating policies and procedures that are vital for these patients.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This project is fully supported and funded by Mazandaran University of Medical Sciences and the Student Research Committee of Mazandaran University of Medical Sciences.
Authors' contributions
Conceptualization, methodology, validation and visualization: Fereshte Iraqian. Supervision, management and financing: Hedayat Jafari; Research and review, sources, draft writing, editing and finalizationthe manuscript: Zahra Alizadeh;
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express our gratitude to the site manager and the library staff of Nasibeh Nursing and Midwifery Faculty in Sari City, Iran, along with other professors and colleagues who helped us in conducting this research.
Palliative care is patient- and family-centered care and is used to predict, prevent, and treat pain, dyspnea, and other distressing symptoms at the end of life when other treatments are ineffective [1]. Palliative care in intensive care units is a debatable issue, however, its use in treatment is increasing. It preserves the function of vital organs and reduces mortality while preventing advanced diseases [2]. Also, palliative care focuses on problems, including physical, psychological, and spiritual distress symptoms along with communication abilities and decision-making power, which reduce the responsibility of caregivers [3]. Palliative care is an approach to care for patients with critical and malignant diseases and their families, which aims to reduce suffering through the management of medical symptoms, psychosocial issues, spiritual care, and determining care goals [4]. Also, palliative care is focused on improving the quality of life of patients with acute diseases, including patients admitted to the intensive care unit. In addition, complex symptoms can be managed by providing timely advice by a specialist palliative care team [5]. A key goal in palliative care is to preserve the dignity of patients in end-of-life care [6]. Dignity is a crucial issue in the matter of care so dignity is a source of values that are expressed absolutely and relatively. Flexibility in maintaining them is influenced by culture [7]. According to the International Council of Nurses, nurses have a vital role in maintaining the dignity of patients, and this is a legal and ethical duty to care for patients as much as possible. These 4 basic responsibilities include promoting health, preventing disease, restoring health, and reducing pain [8]. Dignity therapy is a type of psychotherapy to relieve the mental and physical distress of patients in end-of-life care, and evidence suggests that dignity therapy is very effective. In a randomized clinical trial on patients with high levels of psychological distress, the effectiveness of dignity therapy on the level of anxiety and depression was shown [9]. Dignity is a crucial principle in palliative care for patients and their families so a review of various studies in this field demonstrates various factors that play a role in preserving the dignity of patients in palliative care [10]. Life and death with dignity are fundamental values in palliative care for both patients and family members [11]. A review study shows that various factors, including individual or internal factors and external factors, play a role in maintaining the dignity of patients in palliative care [12]. A study shows that supporting patients with palliative care needs is a crucial part of nursing care [13], and for a person who is critically ill and weak in the intensive care unit, dignity gives them the ability to live according to standards and values [14]. Among the effective factors to preserve the dignity of patients is attention to care factors, such as pain management, shortness of breath management, preparation of patients for end-of-life care, promotion of participation in decision-making, and meeting the needs of patients [15]. Maintaining patients’ dignity is paying attention to communication factors, including establishing communication, dealing with respect, building trust, maintaining dignity and privacy, paying enough attention to the feelings and attitudes of the patient’s family members, and respecting the individual [16]. Considering the importance of preserving the dignity of patients in palliative care and end-of-life care, especially in patients with incurable and malignant diseases, this study aims to examine the dignity of patients under palliative care and the affecting factors on patients.
Materials and Methods
This study was conducted as a narrative review. In the present study, Persian studies were searched in Persian language databases, such as Scientific Information Database (SID) and Magirane with the keywords, dignity of patients, nurse, and palliative care from April 2012 to May 2022. To search for studies in English, the keywords of patient dignity, nurses, and palliative care were used in PubMed and Cochrane databases from June 2010 to May 2022. Also, the search was done in the Google Scholar database in Farsi and English. A manual search was performed on Google as well. The inclusion criterion was complete articles in Farsi and English. The exclusion criterion was the lack of access to the full article. Meanwhile, review articles were excluded from the study. After searching the databases, 106 articles were included in the study. By applying the inclusion and exclusion criteria and removing duplicates, the researchers examined 8 articles (Figure 1).
Results
The results of the study showed that out of 8 studies, 1 study was conducted in Iran. In addition, 5 of the reviewed articles were qualitative studies (Table 1).
Discussion
This narrative review was conducted to examine the dignity of patients under palliative care and the affecting factors on patients. The findings showed that individual, care, and communication factors are critical in maintaining the dignity of patients under palliative care (Table 2). This article was conducted to review the articles from 2010 to 2022 in Persian and English databases with the keywords dignity of patients and palliative care. The review of numerous articles in this field shows that several factors are involved in maintaining the dignity of patients in palliative care. Meanwhile, the word dignity has several meanings at any point in time. Among the factors affecting the preservation of the dignity of patients under palliative care are individual factors (nurses’ cultural and religious background, age, independence/autonomy, free time/positive thinking/being with friends, maintaining identity, feeling connected with others, and being comfortable with the new situation).
Barroso et al. concluded that the cultural and religious background of nurses is effective in understanding the meaning of dignity [22]. In a study by Harvey et al., it was shown that age has a significant impact on understanding and maintaining dignity so it is different in the elderly when compared to younger people [19]. In various studies, it has been shown that various factors, such as self-confidence, interpersonal relationships, especially with friends, family members, and health care providers, and a sense of independence and self-determination are among the vital factors that increase the feeling of dignity. Also, this issue at the time of death is effective for the patient and the patient’s family members [23, 24]. Considering the different aspects of human beings, including psychological, social, and spiritual, one of the vital factors that have been shown in studies is that interaction and communication with healthcare providers and the medical team are effective in increasing or decreasing the patient’s understanding from dignity [25]. One of the crucial skills in increasing the dignity of patients is to allow them to make decisions, especially in patients with a high level of consciousness; accordingly, various studies show that because of the progress of virtual spaces and better access to patients and their families to the sites to diagnose diseases and signs and symptoms, they can intervene in matters related to patients [26]. Hence, the role of healthcare providers in delivering information to patients in the field of disease and ensuring them regarding the maintenance of their independence is still challenging [27]. On the other hand, if the independence of patients in doing daily tasks is ignored, the dignity of patients in the matter of care reduces [28]. One of the vital aspects in increasing the dignity of patients is their relationship with healthcare providers, which increases the sense of independence and improves end-of-life care [29]. Among the factors affecting the preservation of the dignity of patients under palliative care, and care factors (helping patients to prepare for end-of-life care, providing the highest level of care quality, management of shortness of breath, pain management, promoting participation in decision-making, fulfilling patient’s wishes, and care). In addition, 5 crucial interventions of nurses and healthcare workers in the field of increasing the sense of dignity, maintaining the sense of dignity and privacy, creating a sense of trust, managing pain and shortness of breath, and promoting participation in decision-making, various studies in this field show that this is achieved when nurses create a sense of trust in patients and pay special attention to their care needs, especially in end-of-life care, while answering patients’ open questions increases patients’ sense of comfort [30]. A study conducted on cancer patients at the end of life shows that cares, such as pain and shortness of breath management and the prescription of painkillers and their support are among crucial interventions in the treatment of incurable patients and care of the end-of-life [10]. Other factors affecting the preservation of the dignity of patients under palliative care are communication factors (establishing communication, dealing with respect, building trust, preserving dignity and privacy, paying enough attention to the feelings and attitudes of the patient’s family members, and respecting the person). Establishing communication between patients and healthcare providers and their families increases the sense of self-confidence and dignity of patients in end-of-life and palliative care [31]. Also, a study has shown that communication along with participation in patients’ decision-making and family members in the treatment process is not worrying and practical in the palliative care needs of patients [32]. Palliative care is a solution that improves the quality of life of the patient and his family in facing the problems related to the disease by preventing the suffering of the patient and improving the symptoms and other physical, psychological, spiritual, and social problems of the patient. This care begins with the diagnosis of the disease and continues throughout the disease [33]. Respecting the dignity of people is a crucial issue to increase their satisfaction with the services provided by the staff, followed by the establishment of a favorable relationship between patients and nurses and a sense of security and privacy to reduce the length of stay of patients in the hospital and reduce costs. Therefore, it is necessary that the treatment team, especially nurses, become more familiar with the concept of human dignity and pay attention to it in care [18].
Conclusion
According to the review of numerous review articles in the field of dignity, human dignity, and palliative care along with the study results, nurses, as vital members in caring for patients, especially incurable patients and in end-of-life care and need of palliative care, should consider maintaining dignity and human dignity as their duty and perform their professional duties deservedly according to the factors affecting the creation and preservation of human dignity. According to the results of the studies and investigating the effective factors in maintaining human dignity and the effect of dignity therapy, the results of such research can be used to improve the care of patients with incurable diseases who need palliative care and to create trust and proper communication with patients and their families. Since the perception of dignity is a dynamic process and is different and changing during different times and lifetimes, it is suggested that more studies be conducted to investigate this issue from other perspectives, such as health professionals and relatives. Healthcare planning should consider the factors that increase the sense of dignity and should consider creating policies and procedures that are vital for these patients.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This project is fully supported and funded by Mazandaran University of Medical Sciences and the Student Research Committee of Mazandaran University of Medical Sciences.
Authors' contributions
Conceptualization, methodology, validation and visualization: Fereshte Iraqian. Supervision, management and financing: Hedayat Jafari; Research and review, sources, draft writing, editing and finalizationthe manuscript: Zahra Alizadeh;
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express our gratitude to the site manager and the library staff of Nasibeh Nursing and Midwifery Faculty in Sari City, Iran, along with other professors and colleagues who helped us in conducting this research.
References
- Mercadante S, Gregoretti C, Cortegiani A. Palliative care in intensive care units: Why, where, what, who, when, how. BMC Anesthesiol. 2018; 18:106. [DOI:10.1186/s12871-018-0574-9] [PMID] [PMCID]
- Angus DC, Truog RD. Toward better ICU use at the end of life. JAMA. 2016; 315(3):255-6. [DOI:10.1001/jama.2015.18681] [PMID]
- Aslakson RA, Reinke LF, Cox C, Kross EK, Benzo RP, Curtis JR. Developing a research agenda for integrating palliative care into critical care and pulmonary practice to improve patient and family outcomes. J Palliat Med. 2017; 20(4):329-43. [DOI:10.1089/jpm.2016.0567] [PMID] [PMCID]
- Glover TL, Kluger BM. Palliative medicine and end-of-life care. Handb Clin Neurol. 2019; 167:545-61. [DOI:10.1016/B978-0-12-804766-8.00030-3] [PMID]
- Crooms RC, Gelfman LP. Palliative care and end-of-life considerations for the frail patient. Anesth Analg. 2020; 130(6):1504-15. [DOI:10.1213/ANE.0000000000004763] [PMID] [PMCID]
- Viftrup DT, Hvidt NC, Prinds C. Dignity in end-of-life care at hospice: An action research study. Scand J Caring Sci. 2021; 35(2):420-9. [DOI:10.1111/scs.12872] [PMID]
- Lindwall L, Lohne V. Human dignity research in clinical practice-a systematic literature review. Scand J Caring Sci. 2021; 35(4):1038-49. [DOI:10.1111/scs.12922] [PMID] [PMCID]
- Buka P. Essential law and ethics in nursing: Patients, rights and decision-making. London: Routledge; 2020. [DOI:10.4324/9780429292187]
- Martínez M, Arantzamendi M, Belar A, Carrasco JM, Carvajal A, Rullán M, et al. ‘Dignity therapy’, a promising intervention in palliative care: A comprehensive systematic literature review. Palliat Med. 2017; 31(6):492-509. [DOI:10.1177/0269216316665562] [PMID] [PMCID]
- Nunziante F, Tanzi S, Alquati S, Autelitano C, Bedeschi E, Bertocchi E, et al. Providing dignity therapy to patients with advanced cancer: A feasibility study within the setting of a hospital palliative care unit. BMC Palliat Care. 2021; 20:129. [DOI:10.1186/s12904-021-00821-3] [PMID] [PMCID]
- Hall S, Petkova H, Tsouros AD, Costantini M, Higginson IJ. Palliative care for older people: Better practices. Geneva: World Health Organization; 2011. https://apps.who.int/iris/handle/10665/326378
- Guo Q, Jacelon CS. An integrative review of dignity in end-of-life care. Palliat Med. 2014; 28(7):931-40. [DOI:10.1177/0269216314528399] [PMID]
- Hemati Z, Ashouri E, AllahBakhshian M, Pourfarzad Z, Shirani F, Safazadeh S, et al. Dying with dignity: A concept analysis. J Clin Nurs. 2016; 25(9-10):1218-28. [DOI:10.1111/jocn.13143] [PMID]
- Barclay L. In sickness and in dignity: A philosophical account of the meaning of dignity in health care. Int J Nurs Stud. 2016; 61:136-41. [DOI:10.1016/j.ijnurstu.2016.06.010] [PMID]
- McIlfatrick S, Connolly M, Collins R, Murphy T, Johnston B, Larkin P. Evaluating a dignity care intervention for palliative care in the community setting: Community nurses’ perspectives. J Clin Nurs. 2017; 26(23-24):4300-12. [DOI:10.1111/jocn.13757] [PMID]
- Franco ME, Salvetti MG, Donato SCT, Carvalho RT, Franck EM. Perception of dignity of patients in palliative care. Texto Contexto Enferm. 2019; 28. [DOI:10.1590/1980-265x-tce-2018-0142]
- Doorenbos AZ, Juntasopeepun P, Eaton LH, Rue T, Hong E, Coenen A. Palliative care nursing interventions in Thailand. J Transcult Nurs. 2013; 24(4):332-9. [DOI:10.1177/1043659613493439] [PMID] [PMCID]
- Bagheri H, Taghva F, Sadeh M, Shahbeygi N, Ghaderi F, Mohammad Gholi N, et al. [Viewpoint of nurses and patients about inherent dignity of patients (Persian)]. Sci J Nurs Midwifery Paramed Fac. 2018; 4(2):50-8. [Link]
- Chochinov HM, Kristjanson LJ, Breitbart W, McClement S, Hack TF, Hassard T, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: A randomised controlled trial. FOCUS. 2013; 11(4):576-87. [DOI:10.1176/appi.focus.11.4.576]
- Östlund U, Blomberg K, Söderman A, Werkander Harstäde C. How to conserve dignity in palliative care: Suggestions from older patients, significant others, and healthcare professionals in Swedish municipal care. BMC Palliat Care. 2019; 18:10. [DOI:10.1186/s12904-019-0393-x] [PMID] [PMCID]
- Sandgren A, Axelsson L, Bylund-Grenklo T, Benzein E. Family members’ expressions of dignity in palliative care: A qualitative study. Scand J Caring Sci. 2021; 35(3):937-44. [DOI:10.1111/scs.12913] [PMID] [PMCID]
- Barroso LR. Here, there and everywhere': human dignity in contemporary law and in the transnational discourse. Boston Coll Int Comp Law Rev. 2012; 35(2):331. [Link]
- Meier EA, Gallegos JV, Thomas LP, Depp CA, Irwin SA, Jeste DV. Defining a good death (successful dying): Literature review and a call for research and public dialogue. Am J Geriatr Psychiatry. 2016; 24(4):261-71. [DOI:10.1016/j.jagp.2016.01.135] [PMID] [PMCID]
- Mojapelo TD, Usher K, Mills J. Effective pain management as part of palliative care for persons living with HIV/AIDS in a developing country: A qualitative study. J Clin Nurs. 2016; 25(11-12):1598-605. [DOI:10.1111/jocn.13145]
- Britten N. Qualitative research: Qualitative interviews in medical research. BMJ. 1995; 311(6999):251-3. [DOI:10.1136/bmj.311.6999.251] [PMID] [PMCID]
- Peruzzo Jr L. Autonomy, care and respect: The debate on assisted extension of life. Rev Bioet Derecho. 2017; 39:121. [Link]
- Silva JL, Oliveira-Kumakura AR. Clinical simulation to teach nursing care for wounded patients. Rev Bras Enferm. 2018; 71(S 4):1785-90. [DOI:10.1590/0034-7167-2017-0170] [PMID]
- Rodríguez-Prat A, Monforte-Royo C, Porta-Sales J, Escribano X, Balaguer A. Patient perspectives of dignity, autonomy and control at the end of life: Systematic review and meta-ethnography. PloS One. 2016; 11(3):e0151435. [DOI:10.1371/journal.pone.0151435] [PMID] [PMCID]
- Farrell C, Heaven C. Understanding the impact of chemotherapy on dignity for older people and their partners. Eur J Oncol Nurs. 2018; 36:82-8. [DOI:10.1016/j.ejon.2018.05.008] [PMID]
- Burnard P, Naiyapatana W. Culture and communication in Thai nursing: A report of an ethnographic study. Int J Nurs Stud. 2004; 41(7):755-65. [DOI:10.1016/j.ijnurstu.2004.03.002] [PMID]
- Agarwal A, Alshakhs S, Luth E, Dignam R, Reid MC, Adelman RD, et al. Caregiver challenges seen from the perspective of certified home hospice medical directors. Am J Hosp Palliat Care. 2022; 39(9):1023-8. [PMID]
- Östlund U, Brown H, Johnston B. Dignity conserving care at end-of-life: A narrative review. Eur J Oncol Nurs. 2012; 16(4):353-67. [DOI:10.1016/j.ejon.2011.07.010] [PMID]
- Radbruch L, De Lima L, Knaul F, Wenk R, Ali Z, Bhatnaghar S, et al. Redefining palliative care—a new consensus-based definition. J Pain Symptom Manage. 2020; 60(4):754-64. [PMID]
Type of Study: Research |
Subject:
Medical ethics
Received: 2022/12/24 | Accepted: 2023/04/3 | Published: 2023/01/1
Received: 2022/12/24 | Accepted: 2023/04/3 | Published: 2023/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







