Fri, Dec 19, 2025
[Archive]
Volume 1, Issue 2 (Winter 2023)
CPR 2023, 1(2): 216-227 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Firouz H, Sepehr V, Sharifi Z, Hosseinie F. Investigating the Relationship Between the Severity of Depression and Demographic Characteristics in Patients With Atopic Dermatitis in 2019. CPR 2023; 1 (2) :216-227
URL: http://cpr.mazums.ac.ir/article-1-39-en.html
URL: http://cpr.mazums.ac.ir/article-1-39-en.html
Department of Nursing, Faculty of Nursing and Midwifery, Mashhad Medical Sciences Branch, Islamic Azad University, Mashhad, Iran.
Full-Text [PDF 1351 kb]
(592 Downloads)
| Abstract (HTML) (1230 Views)
Full-Text: (631 Views)
Introduction
Dermatitis or eczema is an inflammatory response of the skin to various factors. Its clinical symptoms include itching, redness, scaling, papule, and vesicle lesions. Dermatitis is divided into the two following groups: exogenous and endogenous. One of the most important endogenous types is atopic dermatitis. Atopic dermatitis is an inflammatory skin reaction that is chronically associated with periods of relapse and recovery and can have genetic causes. This disorder is included in the category of the atopic triad [1]. Atopic dermatitis is a chronic and inflammatory disease that was first proposed by Sulzberger and Wise in 1933 [2]. The clinical symptoms of this disease may be different in different people. The most common symptoms include dryness, redness, macules, papules, and vesicles on the skin. Eczema areas are associated with scaly and peeling skin, secondary infection, lymphadenopathy, sensitivity to light, and itching. Itching is the most important symptom of this disease and scratching the skin may cause numerous changes in the skin of these subjects. The backs of the knees, wrists, face, and hands are the most commonly affected areas in patients with this disorder [3-5]. These clinical signs are very weak in the diagnosis of atopic dermatitis and no valid clinical signs and laboratory tests exist in this field [6, 7]. Affected patients sleep less than normal people, suffer from psychological damage, and are disturbed in doing daily tasks, which causes heavy costs to the family and society.
This disease usually starts before the age of two years and the first clinical symptoms are seen at this age. Accordingly, 7% to 17% of children are affected by this disease, and lasts until adulthood in two-thirds of children, affecting different areas of the body depending on the age [8].
Evidence shows that the incidence of atopic dermatitis is increasing in all countries that live in a Western-style; however, the exact cause of this issue is unknown [9]. In industrial areas and developed countries, the prevalence of the disease is higher [10]. Most of the epidemiological studies have been conducted in Western countries, and in Iran, few and scattered studies are available in this field [11].
Atopic dermatitis is a chronic and irritating skin disease and is considered the most common chronic inflammatory illness during childhood [1, 2]. Some scientific hypotheses explain the reason for the high prevalence of psychiatric diseases in patients with atopic dermatitis. Atopic dermatitis has a negative psychological effect on a person’s quality of life because of itching, scratching, and sleep disorders. It causes social embarrassment and problems in the affected people’s occupational, educational, economic, and social fields. Evidence shows that depression is more common in adults with atopic dermatitis and its relationship with these psychiatric symptoms may be influenced by various factors, such as the severity of the disease, subjective and objective assessment of the severity of the illness, and the patient’s quality of life [6].
In a descriptive study conducted in 2013 by Haj Heydari et al., the authors investigated the psychological damage to clients of skin clinics in Sari City, Iran. A total of 404 skin patients filled in a 2-part questionnaire and their demographic-medical characteristics were evaluated. The average age of the people who were referred to the clinic was in the range of 27 to 28 years and 39.4% of them were suspected to have a mental disorder. There was a significant relationship between mental disorder and occupation, education level, and positive history of mental illness. The duration of the skin disease, the type of skin disease, and the location of the lesions were not related to mental disorders. Suspected mental disorder cases were more prevalent compared to studies conducted on skin patients outside Iran and also compared to studies conducted on the prevalence of psychiatric disorders and mental health status in people with 15 and higher years of age and older in Iran. The results of this research clarify the relationship between mental disorders and skin diseases and the consideration of psychological factors in the effective treatment of skin diseases by dermatologists [12]. In a review study conducted in 2018 by Ronstad et al., the relationship between depression in patients with atopic dermatitis was investigated and a significant relationship was found between having atopic dermatitis and depression in adults. Also, atopic dermatitis is associated with depression in children; however, little information is available on depression in children. A positive correlation was found between atopic dermatitis in adults and suicidal thoughts. Only a few studies have examined the absolute suicide risk but the majority have shown a positive correlation between suicide and atopic dermatitis. It was concluded that when treating patients with atopic dermatitis, doctors should consider depression and suicidal thoughts in these patients. As improving atopic dermatitis reduces these risks, it should be prioritized [13]. Since there have been limited studies on the relationship between the severity of depression and atopic dermatitis, this study aims to investigate the severity of depression in patients with atopic dermatitis.
Materials and Methods
This was a descriptive-correlational study that was conducted in Iran in 2018 on 76 patients with atopic dermatitis. These patients were referred to the skin clinic of 22 Bahman Hospital in Mashhad City, Iran after the diagnosis of the disease by a dermatologist, and they were selected by the available sampling method. After coordinating with the officials of the hospital and obtaining an informed consent letter from the patients, a demographic information questionnaire and the Hamilton depression questionnaire were given to them. The criteria for entering the research included having atopic dermatitis and being over 12 years of age. The exclusion criteria were unwillingness to participate in the study, having a history of chronic depression, and having a history of hospitalization in a psychiatric ward. The data were analyzed using the Chi-square and the Fisher statistical tests via the SPSS software, version 16.
Study instruments
Hamilton depression inventory
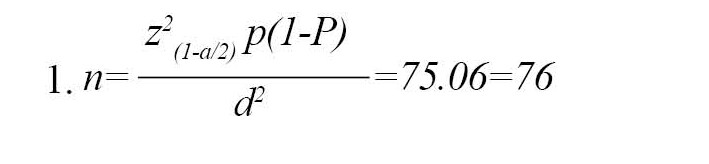
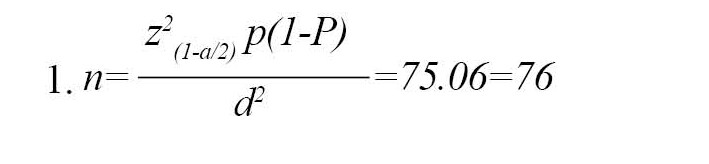
The Hamilton depression inventory (HAM-D) is one of the first scales prepared for depression, implemented by a therapist. It is designed to assess the severity of depression in patients. The original version of the HAM-D contained 21 items; however, Hamilton believed the final 4 items (daily changes, depersonalization, paranoia symptoms, and obsessive-compulsive disorder symptoms) should not be included in the total score as these symptoms are either atypical or reflective and they do not cause depression. Thus, the 17-item version of the HAM-D became the standard for clinical trials, and over the years it has become the most widely used scale in controlled clinical trials of depression. A recent study showed that more than 500 studies have used HAM-D, considering it an effective measurement scale. HAM-D is a multidimensional scale. Accordingly, specific scores of each item cannot predict the overall score of the scale. All the questions are scored from 0 to 4, and the sum of the points determines the severity of depression in the patient. A total score of 0 to 7 indicates normal depression, scores from 8 to 16 indicate mild depression, scores from 17 to 23 indicate moderate depression and scores above 24 indicate severe depression. Several studies have examined the internal reliability of different versions of HAM-D and the results have shown a range from 0.48 to 0.92. Recent studies have obtained an internal reliability coefficient of 0.83 for HAM-D-17 and 0.88 for HAM-D-24 [14]. The face and content validity of the tool was checked using experts’ opinions. In addition, the content validity index (CVI) and content validity ratio (CVR) were considered. According to the study by Manzoni et al. [15], the sample size was calculated at 76 people based on Equation 1:
Results
The mean age of the patients was 38.11±14.07 years. A total of 37(51.3%) patients were male and 39(51.3%) were female. The average depression score was 8.55±6.87. According to the results, 47 patients (61.8%) were without depression, 17 patients (22.4%) had mild depression, and 10 patients (13.2%) suffered from moderate depression. Finally, 2 individuals (2.6%) had severe depression.
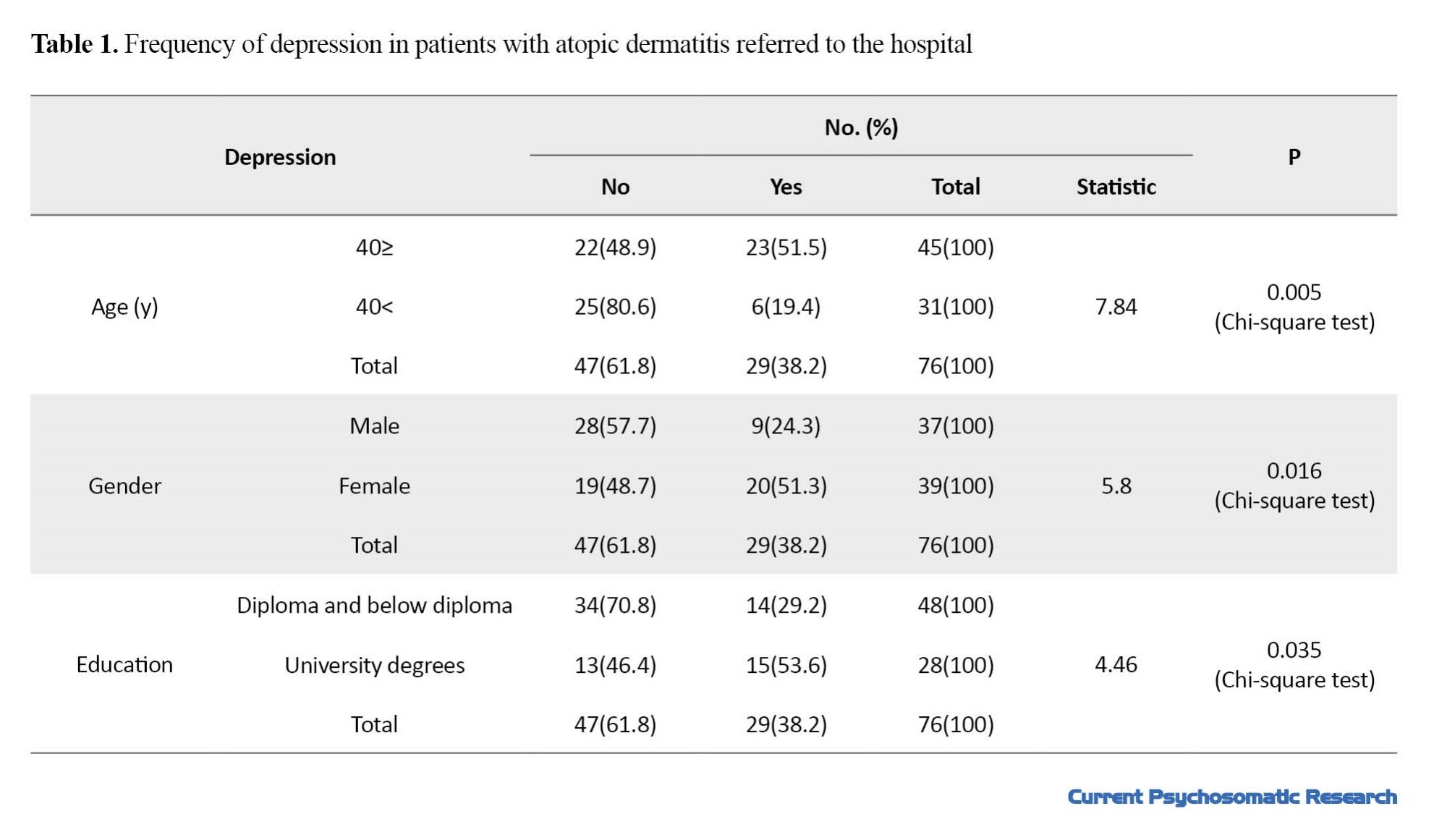
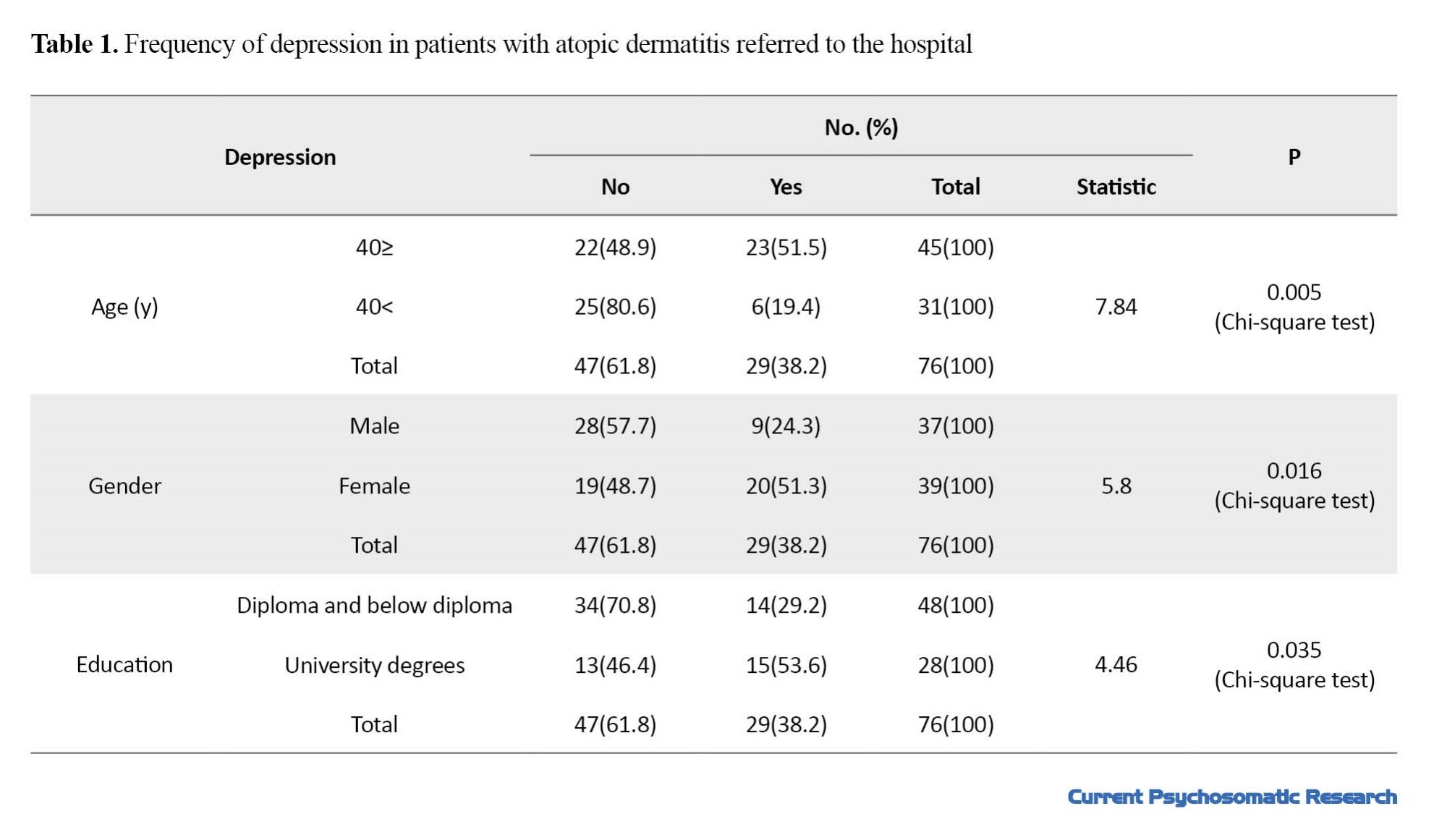
As shown in Table 1, the frequency of depression in patients aged less than 40 years was significantly higher compared to patients older than 40 years (51.1% vs 19.4%; P=0.005). Also, the frequency of depression in female patients was significantly higher compared to male patients (51.3% vs 24.3%; P=0.016). Finally, the frequency of depression was significantly higher in patients with a university education compared to individuals with a diploma or less (53.6% vs 29.2%, P=0.035).
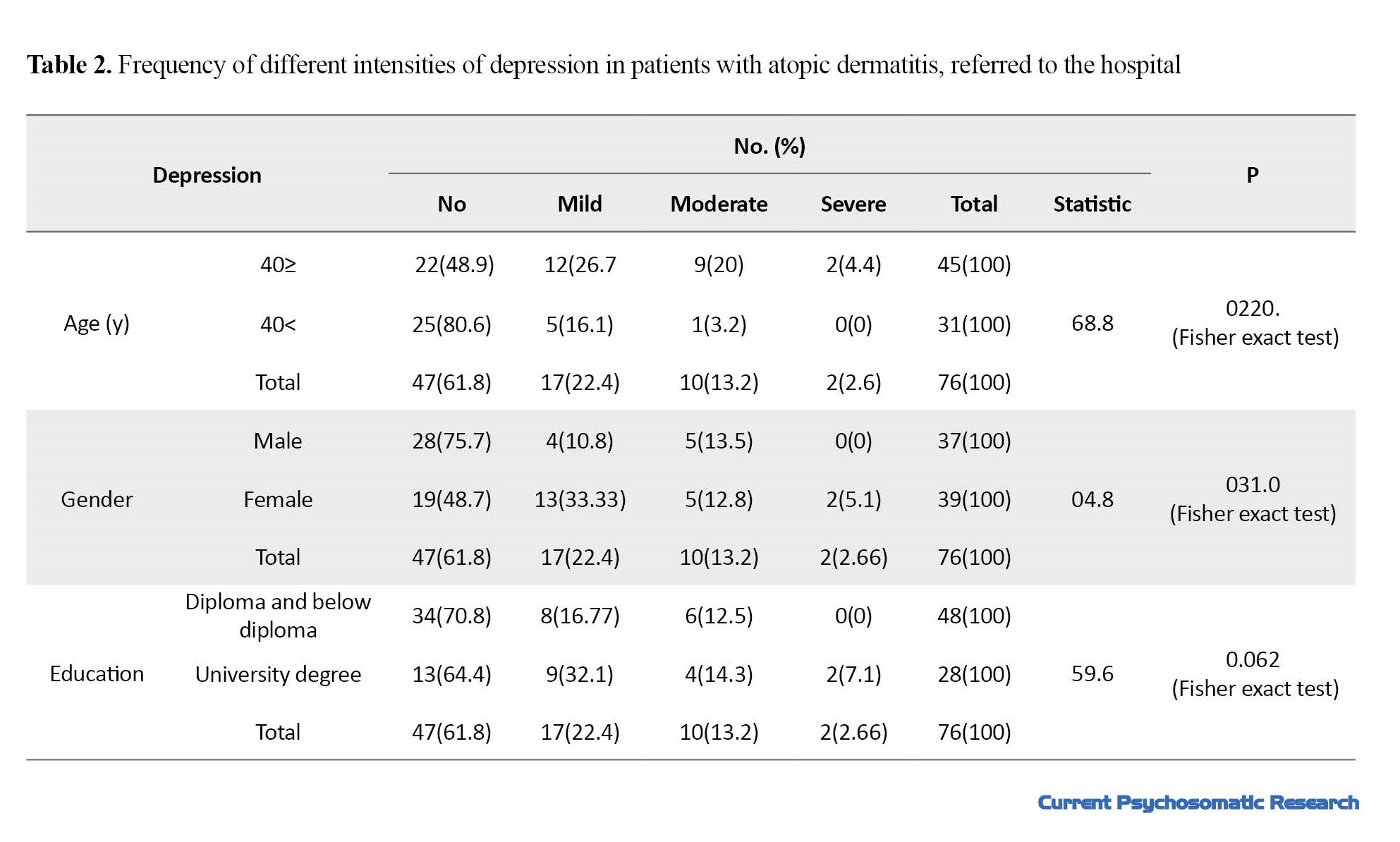
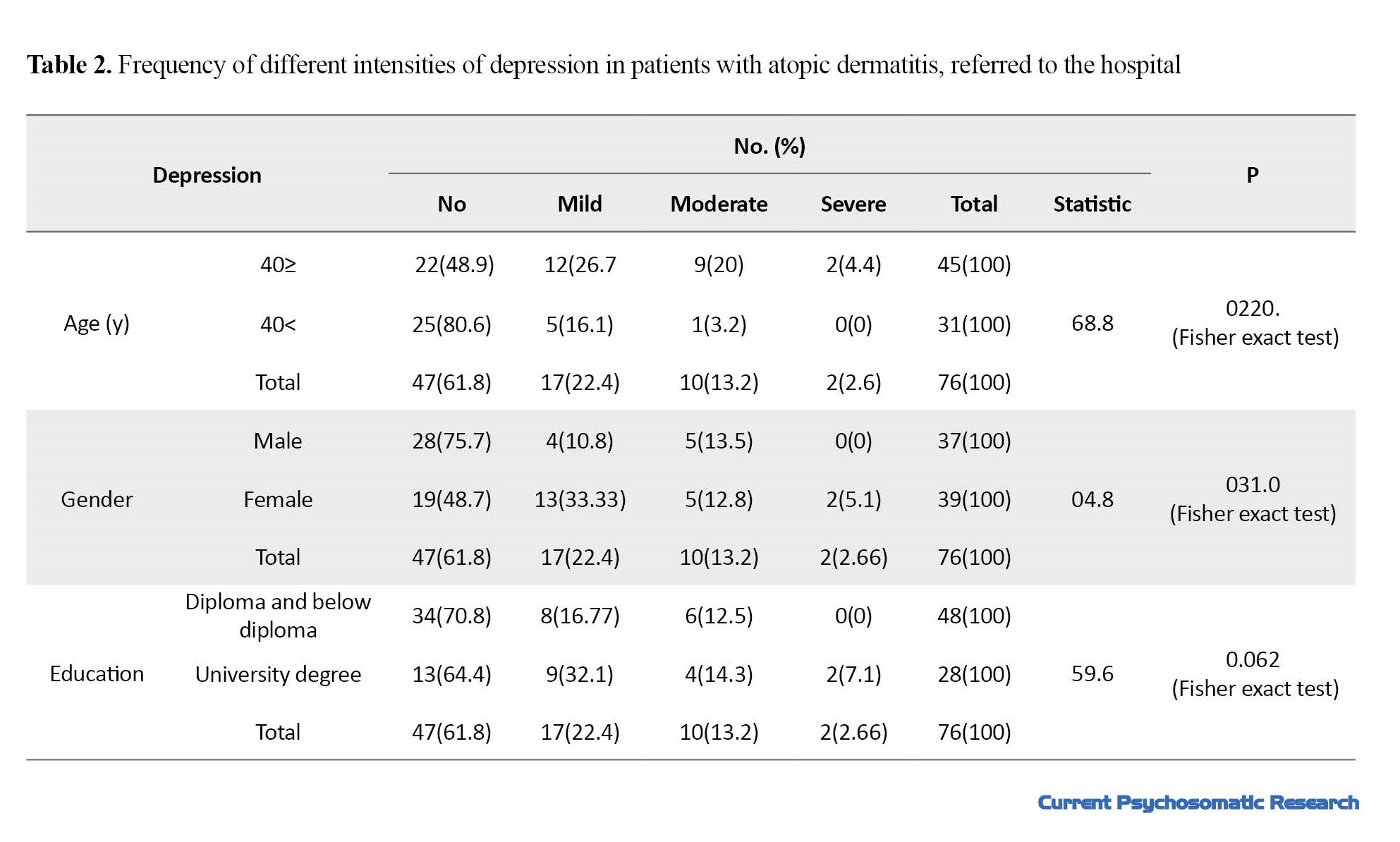
As shown in Table 2, the frequency of moderate and severe depression in patients younger than 40 years was significantly higher compared to patients more than 40 years of age (P=0.022). Also, the frequency of severe and mild depression in female patients was significantly higher compared to male patients (P=0.031). Finally, no statistically significant difference was observed in the frequency of different degrees of depression in patients with atopic dermatitis based on education (P=0.031).
Discussion
The present study was conducted to investigate the severity of depression in patients with atopic dermatitis referred to the skin clinic of 22 Bahman Hospital in Mashhad City, Iran, in 2018. In a study conducted in 2020 by Yochaei et al. to investigate depression in patients with atopic dermatitis, they identified 526 808 adults with atopic eczema; meanwhile, 2,569,030 healthy people were also matched and included in the study. As the severity of atopic eczema increased, the severity of depression increased as well. It was concluded that adults with atopic eczema are more likely to suffer from depression. Also, in terms of depression, they observed a dose-response relationship with the severity of atopic eczema [16]. Although the studied sample size was far bigger than our study, the findings are in line with our results, as they show a significant increase in the severity of depression in patients with atopic dermatitis. In research conducted by Lim et al. in 2016 at the National Skin Care Center of Singapore, titled “anxiety and depression in patients with atopic dermatitis in a somatic dermatology center in Southeast Asia,” a total of 100 patients with atopic dermatitis with no history of psychiatric diseases who had visited the skin clinic of the National Skin Care Center of Singapore in 2008-2009 were investigated using the atopic dermatitis grade scale and the hospital anxiety and depression scale. The average depression score based on HADS was 5. In these patients, compared to individuals without atopic dermatitis, the intensity of depression was significantly higher [9]. The findings of the mentioned study regarding the high severity of depression in the case group are similar to our study. Although there was no control group for comparison in the present study, the percentage reported in the mentioned study is far less than our findings. The severity reported in the mentioned study compared to our study is also related to the economic and social conditions of the society because factors other than the disease may aggravate depression. In a review study conducted by Ronstad et al. in 2018 to investigate the prevalence of depression in patients with atopic dermatitis, a significant relationship was observed between atopic dermatitis and depression in adults. It was concluded that when treating patients with atopic dermatitis, depression, anxiety, and suicidal thoughts should be considered by doctors. Since improvement in atopic dermatitis appears to reduce these risks, this issue should be considered a priority [13]. Our study was also conducted on people over 12 years of age and the risk of severe depression in the patients was high. Although suicide risk and suicidal thoughts were not investigated in our study, the increase in mental health disorders augments the incidence of suicide in people, which requires more studies in this field. In a study conducted by Maina et al. in 2015 in New Delhi, India, titled “gender differences in depression and anxiety caused by atopic dermatitis,” a total of 81 patients (36 men and 45 women) were randomly sampled. They were included in the study after receiving an informed consent letter from the skin care clinic. All patients underwent initial evaluations of mental disorders. In this study, the prevalence of depression was 15%. Also, the severity of depression was significantly higher in women compared to men. As a result of this study, women with atopic dermatitis are more likely to suffer from depression [17]. The findings of the mentioned study regarding the higher level of depression in women were similar to ours, with the difference that the intensity reported in the mentioned study is far less than ours. The results of our study showed that 22.4% of patients with atopic dermatitis had mild depression, 13.2% had moderate depression, and 2.6% had severe depression. It was also found that depression was associated with young age, female gender, and education. Therefore, according to the high severity of depression in patients with atopic dermatitis and the identification of effective factors in aggravating depression, patients with atopic dermatitis with a higher risk should be properly screened and appropriate counseling and educational measures should be taken, in addition to standard treatment for people to reduce the severity of depression and its complications.
Ethical Considerations
Compliance with ethical guidelines
This article is from a research project with the code IR.IAU.MSHD.REC.1398.113 approved by the Ethics Committee of Mashhad Medical Sciences Branch of Islamic Azad University.
Funding
This article is extracted from the professional doctorate thesis of Homa Firoz, approved by Faculty of Medicine, Mashhad Medical Sciences Branch of Islamic Azad University.
Authors' contributions
Research and review: Homa Firouz; Supervision: Vahid Sepehr; Draftin the manuscript: Zahra Sharifi; Editing and finalization: Fateme Hosseini.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We would like to thank all relevant authorities and participants for their cooperation in the implementation of this research project.
Dermatitis or eczema is an inflammatory response of the skin to various factors. Its clinical symptoms include itching, redness, scaling, papule, and vesicle lesions. Dermatitis is divided into the two following groups: exogenous and endogenous. One of the most important endogenous types is atopic dermatitis. Atopic dermatitis is an inflammatory skin reaction that is chronically associated with periods of relapse and recovery and can have genetic causes. This disorder is included in the category of the atopic triad [1]. Atopic dermatitis is a chronic and inflammatory disease that was first proposed by Sulzberger and Wise in 1933 [2]. The clinical symptoms of this disease may be different in different people. The most common symptoms include dryness, redness, macules, papules, and vesicles on the skin. Eczema areas are associated with scaly and peeling skin, secondary infection, lymphadenopathy, sensitivity to light, and itching. Itching is the most important symptom of this disease and scratching the skin may cause numerous changes in the skin of these subjects. The backs of the knees, wrists, face, and hands are the most commonly affected areas in patients with this disorder [3-5]. These clinical signs are very weak in the diagnosis of atopic dermatitis and no valid clinical signs and laboratory tests exist in this field [6, 7]. Affected patients sleep less than normal people, suffer from psychological damage, and are disturbed in doing daily tasks, which causes heavy costs to the family and society.
This disease usually starts before the age of two years and the first clinical symptoms are seen at this age. Accordingly, 7% to 17% of children are affected by this disease, and lasts until adulthood in two-thirds of children, affecting different areas of the body depending on the age [8].
Evidence shows that the incidence of atopic dermatitis is increasing in all countries that live in a Western-style; however, the exact cause of this issue is unknown [9]. In industrial areas and developed countries, the prevalence of the disease is higher [10]. Most of the epidemiological studies have been conducted in Western countries, and in Iran, few and scattered studies are available in this field [11].
Atopic dermatitis is a chronic and irritating skin disease and is considered the most common chronic inflammatory illness during childhood [1, 2]. Some scientific hypotheses explain the reason for the high prevalence of psychiatric diseases in patients with atopic dermatitis. Atopic dermatitis has a negative psychological effect on a person’s quality of life because of itching, scratching, and sleep disorders. It causes social embarrassment and problems in the affected people’s occupational, educational, economic, and social fields. Evidence shows that depression is more common in adults with atopic dermatitis and its relationship with these psychiatric symptoms may be influenced by various factors, such as the severity of the disease, subjective and objective assessment of the severity of the illness, and the patient’s quality of life [6].
In a descriptive study conducted in 2013 by Haj Heydari et al., the authors investigated the psychological damage to clients of skin clinics in Sari City, Iran. A total of 404 skin patients filled in a 2-part questionnaire and their demographic-medical characteristics were evaluated. The average age of the people who were referred to the clinic was in the range of 27 to 28 years and 39.4% of them were suspected to have a mental disorder. There was a significant relationship between mental disorder and occupation, education level, and positive history of mental illness. The duration of the skin disease, the type of skin disease, and the location of the lesions were not related to mental disorders. Suspected mental disorder cases were more prevalent compared to studies conducted on skin patients outside Iran and also compared to studies conducted on the prevalence of psychiatric disorders and mental health status in people with 15 and higher years of age and older in Iran. The results of this research clarify the relationship between mental disorders and skin diseases and the consideration of psychological factors in the effective treatment of skin diseases by dermatologists [12]. In a review study conducted in 2018 by Ronstad et al., the relationship between depression in patients with atopic dermatitis was investigated and a significant relationship was found between having atopic dermatitis and depression in adults. Also, atopic dermatitis is associated with depression in children; however, little information is available on depression in children. A positive correlation was found between atopic dermatitis in adults and suicidal thoughts. Only a few studies have examined the absolute suicide risk but the majority have shown a positive correlation between suicide and atopic dermatitis. It was concluded that when treating patients with atopic dermatitis, doctors should consider depression and suicidal thoughts in these patients. As improving atopic dermatitis reduces these risks, it should be prioritized [13]. Since there have been limited studies on the relationship between the severity of depression and atopic dermatitis, this study aims to investigate the severity of depression in patients with atopic dermatitis.
Materials and Methods
This was a descriptive-correlational study that was conducted in Iran in 2018 on 76 patients with atopic dermatitis. These patients were referred to the skin clinic of 22 Bahman Hospital in Mashhad City, Iran after the diagnosis of the disease by a dermatologist, and they were selected by the available sampling method. After coordinating with the officials of the hospital and obtaining an informed consent letter from the patients, a demographic information questionnaire and the Hamilton depression questionnaire were given to them. The criteria for entering the research included having atopic dermatitis and being over 12 years of age. The exclusion criteria were unwillingness to participate in the study, having a history of chronic depression, and having a history of hospitalization in a psychiatric ward. The data were analyzed using the Chi-square and the Fisher statistical tests via the SPSS software, version 16.
Study instruments
Hamilton depression inventory
The Hamilton depression inventory (HAM-D) is one of the first scales prepared for depression, implemented by a therapist. It is designed to assess the severity of depression in patients. The original version of the HAM-D contained 21 items; however, Hamilton believed the final 4 items (daily changes, depersonalization, paranoia symptoms, and obsessive-compulsive disorder symptoms) should not be included in the total score as these symptoms are either atypical or reflective and they do not cause depression. Thus, the 17-item version of the HAM-D became the standard for clinical trials, and over the years it has become the most widely used scale in controlled clinical trials of depression. A recent study showed that more than 500 studies have used HAM-D, considering it an effective measurement scale. HAM-D is a multidimensional scale. Accordingly, specific scores of each item cannot predict the overall score of the scale. All the questions are scored from 0 to 4, and the sum of the points determines the severity of depression in the patient. A total score of 0 to 7 indicates normal depression, scores from 8 to 16 indicate mild depression, scores from 17 to 23 indicate moderate depression and scores above 24 indicate severe depression. Several studies have examined the internal reliability of different versions of HAM-D and the results have shown a range from 0.48 to 0.92. Recent studies have obtained an internal reliability coefficient of 0.83 for HAM-D-17 and 0.88 for HAM-D-24 [14]. The face and content validity of the tool was checked using experts’ opinions. In addition, the content validity index (CVI) and content validity ratio (CVR) were considered. According to the study by Manzoni et al. [15], the sample size was calculated at 76 people based on Equation 1:
Results
The mean age of the patients was 38.11±14.07 years. A total of 37(51.3%) patients were male and 39(51.3%) were female. The average depression score was 8.55±6.87. According to the results, 47 patients (61.8%) were without depression, 17 patients (22.4%) had mild depression, and 10 patients (13.2%) suffered from moderate depression. Finally, 2 individuals (2.6%) had severe depression.
As shown in Table 1, the frequency of depression in patients aged less than 40 years was significantly higher compared to patients older than 40 years (51.1% vs 19.4%; P=0.005). Also, the frequency of depression in female patients was significantly higher compared to male patients (51.3% vs 24.3%; P=0.016). Finally, the frequency of depression was significantly higher in patients with a university education compared to individuals with a diploma or less (53.6% vs 29.2%, P=0.035).
As shown in Table 2, the frequency of moderate and severe depression in patients younger than 40 years was significantly higher compared to patients more than 40 years of age (P=0.022). Also, the frequency of severe and mild depression in female patients was significantly higher compared to male patients (P=0.031). Finally, no statistically significant difference was observed in the frequency of different degrees of depression in patients with atopic dermatitis based on education (P=0.031).
Discussion
The present study was conducted to investigate the severity of depression in patients with atopic dermatitis referred to the skin clinic of 22 Bahman Hospital in Mashhad City, Iran, in 2018. In a study conducted in 2020 by Yochaei et al. to investigate depression in patients with atopic dermatitis, they identified 526 808 adults with atopic eczema; meanwhile, 2,569,030 healthy people were also matched and included in the study. As the severity of atopic eczema increased, the severity of depression increased as well. It was concluded that adults with atopic eczema are more likely to suffer from depression. Also, in terms of depression, they observed a dose-response relationship with the severity of atopic eczema [16]. Although the studied sample size was far bigger than our study, the findings are in line with our results, as they show a significant increase in the severity of depression in patients with atopic dermatitis. In research conducted by Lim et al. in 2016 at the National Skin Care Center of Singapore, titled “anxiety and depression in patients with atopic dermatitis in a somatic dermatology center in Southeast Asia,” a total of 100 patients with atopic dermatitis with no history of psychiatric diseases who had visited the skin clinic of the National Skin Care Center of Singapore in 2008-2009 were investigated using the atopic dermatitis grade scale and the hospital anxiety and depression scale. The average depression score based on HADS was 5. In these patients, compared to individuals without atopic dermatitis, the intensity of depression was significantly higher [9]. The findings of the mentioned study regarding the high severity of depression in the case group are similar to our study. Although there was no control group for comparison in the present study, the percentage reported in the mentioned study is far less than our findings. The severity reported in the mentioned study compared to our study is also related to the economic and social conditions of the society because factors other than the disease may aggravate depression. In a review study conducted by Ronstad et al. in 2018 to investigate the prevalence of depression in patients with atopic dermatitis, a significant relationship was observed between atopic dermatitis and depression in adults. It was concluded that when treating patients with atopic dermatitis, depression, anxiety, and suicidal thoughts should be considered by doctors. Since improvement in atopic dermatitis appears to reduce these risks, this issue should be considered a priority [13]. Our study was also conducted on people over 12 years of age and the risk of severe depression in the patients was high. Although suicide risk and suicidal thoughts were not investigated in our study, the increase in mental health disorders augments the incidence of suicide in people, which requires more studies in this field. In a study conducted by Maina et al. in 2015 in New Delhi, India, titled “gender differences in depression and anxiety caused by atopic dermatitis,” a total of 81 patients (36 men and 45 women) were randomly sampled. They were included in the study after receiving an informed consent letter from the skin care clinic. All patients underwent initial evaluations of mental disorders. In this study, the prevalence of depression was 15%. Also, the severity of depression was significantly higher in women compared to men. As a result of this study, women with atopic dermatitis are more likely to suffer from depression [17]. The findings of the mentioned study regarding the higher level of depression in women were similar to ours, with the difference that the intensity reported in the mentioned study is far less than ours. The results of our study showed that 22.4% of patients with atopic dermatitis had mild depression, 13.2% had moderate depression, and 2.6% had severe depression. It was also found that depression was associated with young age, female gender, and education. Therefore, according to the high severity of depression in patients with atopic dermatitis and the identification of effective factors in aggravating depression, patients with atopic dermatitis with a higher risk should be properly screened and appropriate counseling and educational measures should be taken, in addition to standard treatment for people to reduce the severity of depression and its complications.
Ethical Considerations
Compliance with ethical guidelines
This article is from a research project with the code IR.IAU.MSHD.REC.1398.113 approved by the Ethics Committee of Mashhad Medical Sciences Branch of Islamic Azad University.
Funding
This article is extracted from the professional doctorate thesis of Homa Firoz, approved by Faculty of Medicine, Mashhad Medical Sciences Branch of Islamic Azad University.
Authors' contributions
Research and review: Homa Firouz; Supervision: Vahid Sepehr; Draftin the manuscript: Zahra Sharifi; Editing and finalization: Fateme Hosseini.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We would like to thank all relevant authorities and participants for their cooperation in the implementation of this research project.
References
- Cheng CM, Hsu JW, Huang KL, Bai YM, Su TP, Li CT, et al. Risk of developing major depressive disorder and anxiety disorders among adolescents and adults with atopic dermatitis: A nationwide longitudinal study. J Affect Disord. 2015; 178:60-5. [DOI:10.1016/j.jad.2015.02.025] [PMID]
- Thyssen JP, Hamann CR, Linneberg A, Dantoft TM, Skov L, Gislason GH, et al. Atopic dermatitis is associated with anxiety, depression, and suicidal ideation, but not with psychiatric hospitalization or suicide. Allergy. 2018; 73(1):214-20. [DOI:10.1111/all.13231] [PMID]
- Abuabara K, Yu A, Okhovat JP, Allen I, Langan SM. The prevalence of atopic dermatitis beyond childhood: A systematic review and meta-analysis of longitudinal studies. Allergy. 2018; 73(3):696-704. [DOI:10.1111/all.13320] [PMID] [PMCID]
- Shoormasti RS, Pourpak Z, Fazlollahi MR, Kazemnejad A, Nadali F, Ebadi Z, et al. The prevalence of allergic rhinitis, allergic conjunctivitis, atopic dermatitis and asthma among adults of Tehran. Iran J Public Health. 2018; 47(11):1749-55. [Link]
- Nicholas MN, Gooderham MJ. Atopic dermatitis, depression, and suicidality. J Cutan Med Surg. 2017; 21(3):237-42. [DOI:10.1177/1203475416685078] [PMID]
- Sherry HY, Silverberg JI. Association between atopic dermatitis and depression in US adults. J Invest Dermatol. 2015; 135(12):3183-6. [DOI:10.1038/jid.2015.337] [PMID]
- Slattery MJ, Essex MJ, Paletz EM, Vanness ER, Infante M, Rogers GM, et al. Depression, anxiety, and dermatologic quality of life in adolescents with atopic dermatitis. J Allergy Clin Immunol. 2011; 128(3):668-71. [DOI:10.1016/j.jaci.2011.05.003] [PMID] [PMCID]
- Dalgard FJ, Svensson Å, Gieler U, Tomas-Aragones L, Lien L, Poot F, et al. Dermatologists across Europe underestimate depression and anxiety: Results from 3635 dermatological consultations. Br J Dermatol. 2018; 179(2):464-70. [DOI:10.1111/bjd.16250] [PMID]
- Lim VZ, Ho RC, Tee SI, Ho MS, Pan JY, Lim YL, et al. Anxiety and depression in patients with atopic dermatitis in a Southeast Asian tertiary dermatological centre. Ann Acad Med Singapore. 2016; 45(10):451-5. [DOI:10.47102/annals-acadmedsg.V45N10p451] [PMID]
- Langan SM, Irvine AD, Weidinger S. Atopic dermatitis. Lancet. 2020; 396(10247):345-60. [DOI:10.1016/S0140-6736(20)31286-1] [PMID]
- Moosavi Z, Samadzadeh D. [Prevalence of atopic dermatitis in 7-11 year old school children, Ahwaz (Persian)]. J Shahid Sadoughi Univ Med Sci. 2006; 14(3):38-44. [Link]
- Hajheydari Z, Zarghami M, Khajeh A. [Evaluation of psychological problem based on GHQ-28 Questionnaires in patients attending the dermatological clinics of Sari, Iran, 2004 (Persian)]. J Mazandaran Univ Med Sci. 2006; 15(50):105-12. [Link]
- Rønnstad ATM, Halling-Overgaard AS, Hamann CR, Skov L, Egeberg A, Thyssen JP. Association of atopic dermatitis with depression, anxiety, and suicidal ideation in children and adults: A systematic review and meta-analysis. J Am Acad Dermatol. 2018; 79(3):448-56.e30. [DOI:10.1016/j.jaad.2018.03.017] [PMID]
- Tahghigh I. [Hamilton anxiety rating scale for depreesion (Persian)]. Tehran: Iran Tahghigh. [Link]
- Manzoni AP, Weber MB, Nagatomi AR, Pereira RL, Townsend RZ, Cestari TF. Assessing depression and anxiety in the caregivers of pediatric patients with chronic skin disorders. An Bras Dermatol. 2013; 88(6):894-9. [DOI:10.1590/abd1806-4841.20131915] [PMID] [PMCID]
- Schonmann Y, Mansfield KE, Hayes JF, Abuabara K, Roberts A, Smeeth L, et al. Atopic eczema in adulthood and risk of depression and anxiety: A population-based cohort study. J Allergy Clin Immunol Pract. 2020; 8(1):248-57.e16. [DOI:10.1016/j.jaip.2019.08.030] [PMID] [PMCID]
- Mina S, Jabeen M, Singh S, Verma R. Gender differences in depression and anxiety among atopic dermatitis patients. Indian J Dermatol. 2015; 60(2):211. [DOI:10.4103/0019-5154.152564]
Type of Study: Study protocol |
Subject:
Psychology
Received: 2022/11/1 | Accepted: 2023/04/3 | Published: 2023/01/1
Received: 2022/11/1 | Accepted: 2023/04/3 | Published: 2023/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |