Sun, Jul 27, 2025
[Archive]
Volume 2, Issue 2 (Winter 2024)
CPR 2024, 2(2): 123-132 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sharif-Nia H, Fatehi R, Nowrozi P, Gholampour M H, Ghanbari A, Goudarzian A H et al . Association Between Religious Coping and Body Imagein Patients With Chronic Kidney Failure Undergoing Hemodialysis. CPR 2024; 2 (2) :123-132
URL: http://cpr.mazums.ac.ir/article-1-106-en.html
URL: http://cpr.mazums.ac.ir/article-1-106-en.html
Hamid Sharif-Nia 

 , Reza Fatehi
, Reza Fatehi 

 , Poorya Nowrozi
, Poorya Nowrozi 

 , Mohammad Hashem Gholampour
, Mohammad Hashem Gholampour 

 , Alireza Ghanbari
, Alireza Ghanbari 

 , Amir Hossein Goudarzian
, Amir Hossein Goudarzian 

 , Fatemeh Miraghai
, Fatemeh Miraghai 



 , Reza Fatehi
, Reza Fatehi 

 , Poorya Nowrozi
, Poorya Nowrozi 

 , Mohammad Hashem Gholampour
, Mohammad Hashem Gholampour 

 , Alireza Ghanbari
, Alireza Ghanbari 

 , Amir Hossein Goudarzian
, Amir Hossein Goudarzian 

 , Fatemeh Miraghai
, Fatemeh Miraghai 

Student Research Committee, Mazandaran University of Medical Sciences, Sari, Iran.
Full-Text [PDF 663 kb]
(224 Downloads)
| Abstract (HTML) (1060 Views)
Full-Text: (284 Views)
Introduction
Chronic kidney disease (CKD) is a prevalent health concern that ultimately develops into end-stage renal disease (ESRD) [1]. In 2017, the global count of individuals with ESRD exceeded 850 million, with projections indicating that by 2040, it will emerge as a leading cause of mortality among individuals undergoing hemodialysis [2]. The prevalence of ESRD in the US, Europe and Iran has been documented at 1500, 800 and 360 cases per million, respectively. Notably, in Iran, the prevalence of this advanced chronic ailment notably surged in 2006 compared to 2000. Hemodialysis stands out as one of the most prevalent treatment modalities for ESRD [3]. Estimates suggest a surge of 5.4 million individuals in hemodialysis patients by 2030 [4].
Hemodialysis effectively enhances CKD management and elevates these patients’ quality of life (QoL) [5]. Despite advancements in hemodialysis that have bolstered the survival rates of ESRD patients, individuals with ESRD contend with various physical and psychosocial symptoms, and traditional treatments can disrupt their QoL [1, 6]. While hemodialysis treatment preserves the lives of those with ESRD, it does not avert the disease’s complications, anxiety, despair and similar challenges. Hence, the strategies patients employ to confront these obstacles hold significant importance. Religious coping is crucial for navigating stressful circumstances [1, 6].
Religious coping entails an individual’s ability to integrate religious beliefs and values into daily life and experiences. This capability assists individuals in effectively addressing life’s challenges and uncertainties, particularly through aligning with religious principles and faith in a higher power, enhancing their productivity, and fostering a sense of psychological security [7]. It can serve as a criterion for improving an individual’s mental and spiritual well-being and fortifying their connection with spirituality and religion [7, 8]. Despite the impact of dialysis on both the patient and their family, there exists a necessity for an efficient strategy to diminish dependency, uphold self-esteem, and alleviate concerns regarding body image. Research indicates that healthcare providers often lack sufficient knowledge regarding body image [9]. These patients encounter lifestyle constraints due to their condition, which can influence social interactions, beliefs, and their sense of control. Body image, integral to personal identity formation, significantly affects how patients perceive themselves and individuals undergoing hemodialysis confront physical and psychological challenges like fear, anxiety, and despair. Moreover, they encounter difficulties accepting changes in their physical appearance, which can result in concerns about body image [10].
Body image distortion is distressing and can lead to adverse consequences. A negative body image can impact physical and mental well-being, self-esteem, mood, competence and social and occupational performance [11]. Religion holds significant influence in the lives of numerous individuals [12]. Over recent years, the correlation between religiosity and psychosocial coping has garnered attention in the healthcare domain. It appears that religious or spiritual aspects, broadly defined, play a crucial role in the adaptation process for many patients, particularly those confronting severe illnesses like CKD patients undergoing hemodialysis [13].
With the escalating number of patients undergoing hemodialysis and encountering specific challenges like chronic treatment, lifestyle constraints and substantial alterations in body image and functionality, fostering a positive body image can significantly enhance the QoL for these individuals. Studies indicate a heightened prevalence of body image disorders among hemodialysis patients, with levels notably surpassing those in the general population [13-15]. Effective strategies to address negative body image include encouraging patients to concentrate on positive attributes beyond their physical appearance, such as their values and relationships [14], engaging in suitable physical activities, utilizing cosmetics and employing religious coping mechanisms [9]. Leveraging religious support and coping strategies can prove more efficacious in addressing the psychological and emotional hurdles faced by hemodialysis patients compared to alternative approaches [16, 17].
Given the elevated prevalence of body image disorders among hemodialysis patients and the significant influence of religion in Iran, understanding the correlation between religious coping and body image in hemodialysis patients holds paramount importance in addressing their mental well-being challenges. Understanding the impact of religious coping on shaping the body image of hemodialysis patients is crucial for various reasons. Firstly, it can offer insights into the psychological and emotional effects of religious coping on body image perception, which is vital for addressing the overall well-being of these individuals. Furthermore, such investigations can help in crafting tailored interventions and support mechanisms that consider the religious and spiritual aspects of coping with body image issues within this demographic. Similarly, exploring this connection can contribute to a broader comprehension of the intricate interplay between religious coping, mental health, and physical well-being within the realm of chronic illness and medical care. Hence, conducting a study on the relationship between religious coping and body image in hemodialysis patients becomes imperative to bridge this knowledge gap and advance comprehensive care and assistance for these individuals.
Materials and Methods
Design and participants
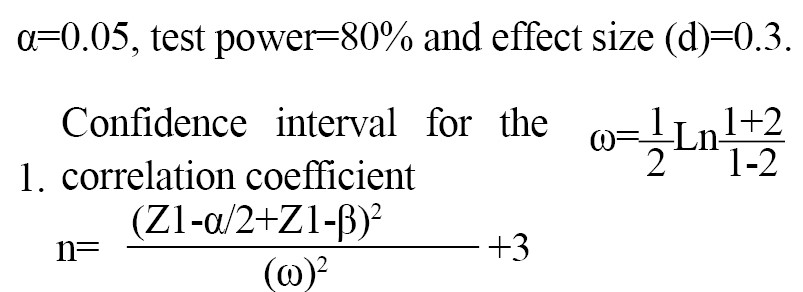
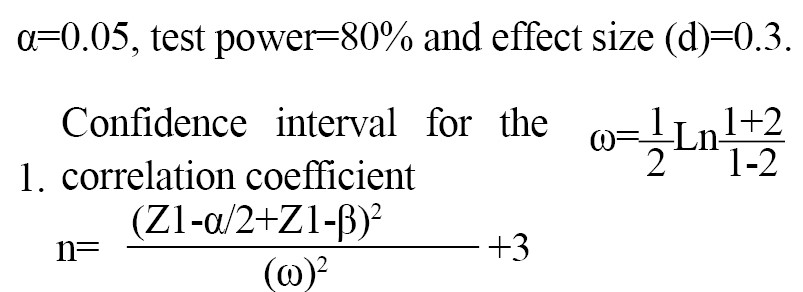
The study design employed in this research was descriptive-correlational and was carried out from March to June 2023. The sample size was 280 individuals using G*Power software version 3.1.7, considering the Equation 1:
The study population comprised patients diagnosed with ESRD undergoing hemodialysis, selected from the Shahrvand Dialysis Center in Sari City, Iran, using the available sampling method. The inclusion criteria encompassed the ability to read and write and the age of 18 years and above. The exclusion criteria involved alcohol addiction, mental, emotional and verbal issues, reduced consciousness levels, and digestive ailments like gastric ulcers, gastric reflux, and congestive heart failure [9].
Research tools
Data collection instruments comprised a demographic checklist (including age, gender, depression, marital status, education level, economic status and occupation), Littleton’s body image concern inventory (BICI) and the religious coping questionnaire (RCOPE) developed by Pargament et al. [19]
Body image concern inventory (BICI)
The BICI questionnaire comprises 19 items initially developed and validated by Littleton et al. (2005), with confirmed validity and reliability [18]. The BICI assesses an individual’s discontent, apprehension, and embarrassment concerning their appearance, including behaviors like checking and concealing perceived flaws and the extent to which fear about one’s appearance hampers social functioning. Responses are rated on a 5-point Likert scale ranging from never=1 to always=5. The total scale score ranges from 19 to 95, with higher scores indicating increased dissatisfaction with one’s body image or appearance [18]. In this study, the questionnaire’s reliability was assessed using the Cronbach α coefficient, yielding a value of 0.943.
Religious coping questionnaire (RCOPE)
The investigation into religious coping methods utilized the short form of RCOPE, a tool with confirmed validity and reliability. This standardized instrument comprises 14 items designed by Pargament et al. [19] to assess positive and negative religious coping strategies. Each scale, positive and negative, consists of seven religious coping items. RCOPE responses are rated on a 4-point Likert scale ranging from “not at all” to “very much.” Positive religious coping involves confronting adverse life events, and an individual embraces these events by deriving positive insights and changes linked to divine assistance [19]. In this study, the questionnaire’s reliability was assessed using Cronbach’s α, resulting in a value of 0.707.
Data analysis
The obtained data were analyzed using SPSS software, version 26. The normal distribution of continuous quantitative data was assessed using the Kolmogorov-Smirnov test. Simple linear regression was employed to examine the relationship between religious coping variables and body image among hemodialysis patients. Furthermore, variables that exhibited significance in simple linear regression were concurrently assessed in multiple linear regression. A significance level of <0.05 was considered for all tests.
Results
Demographic characteristics
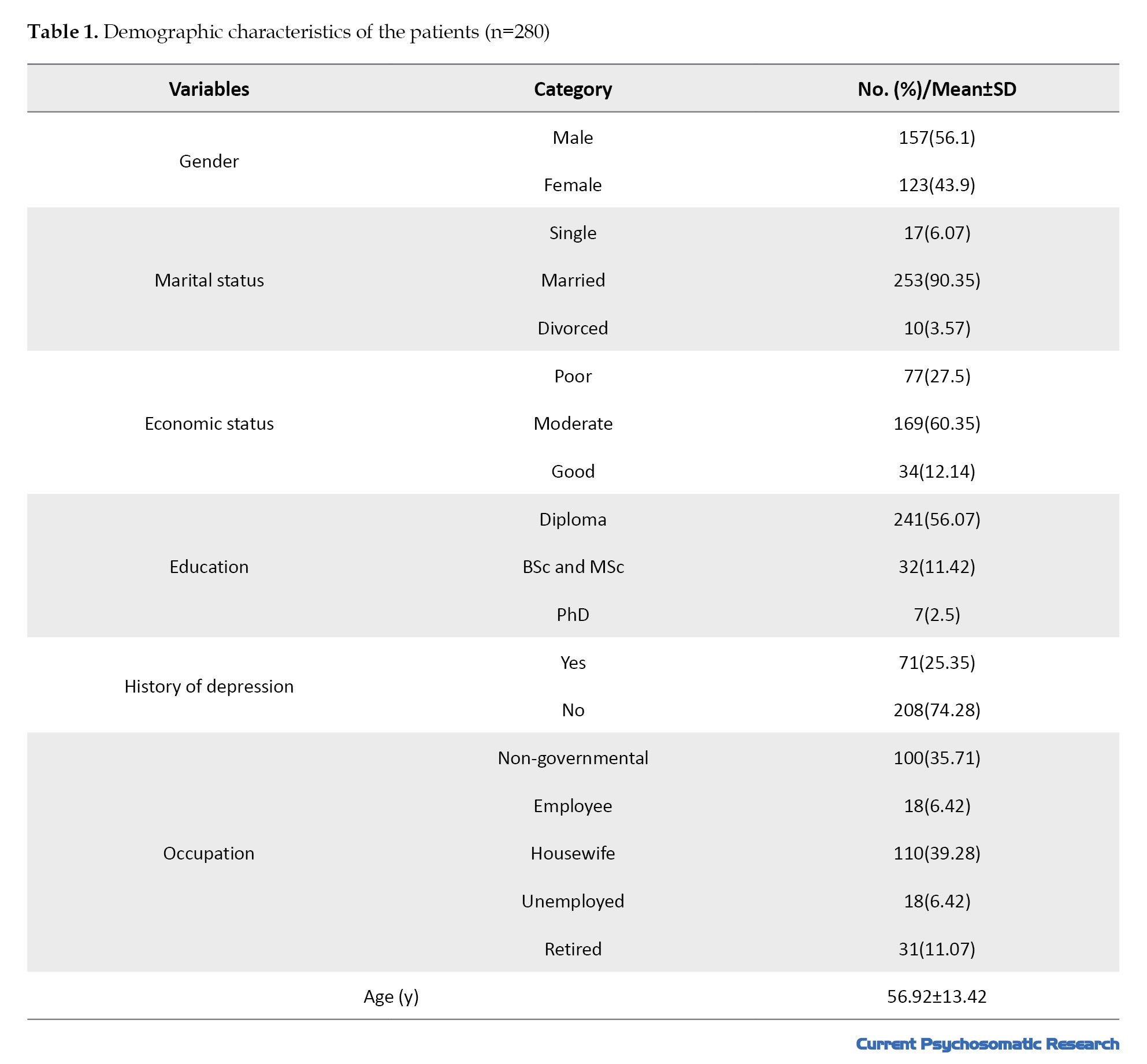
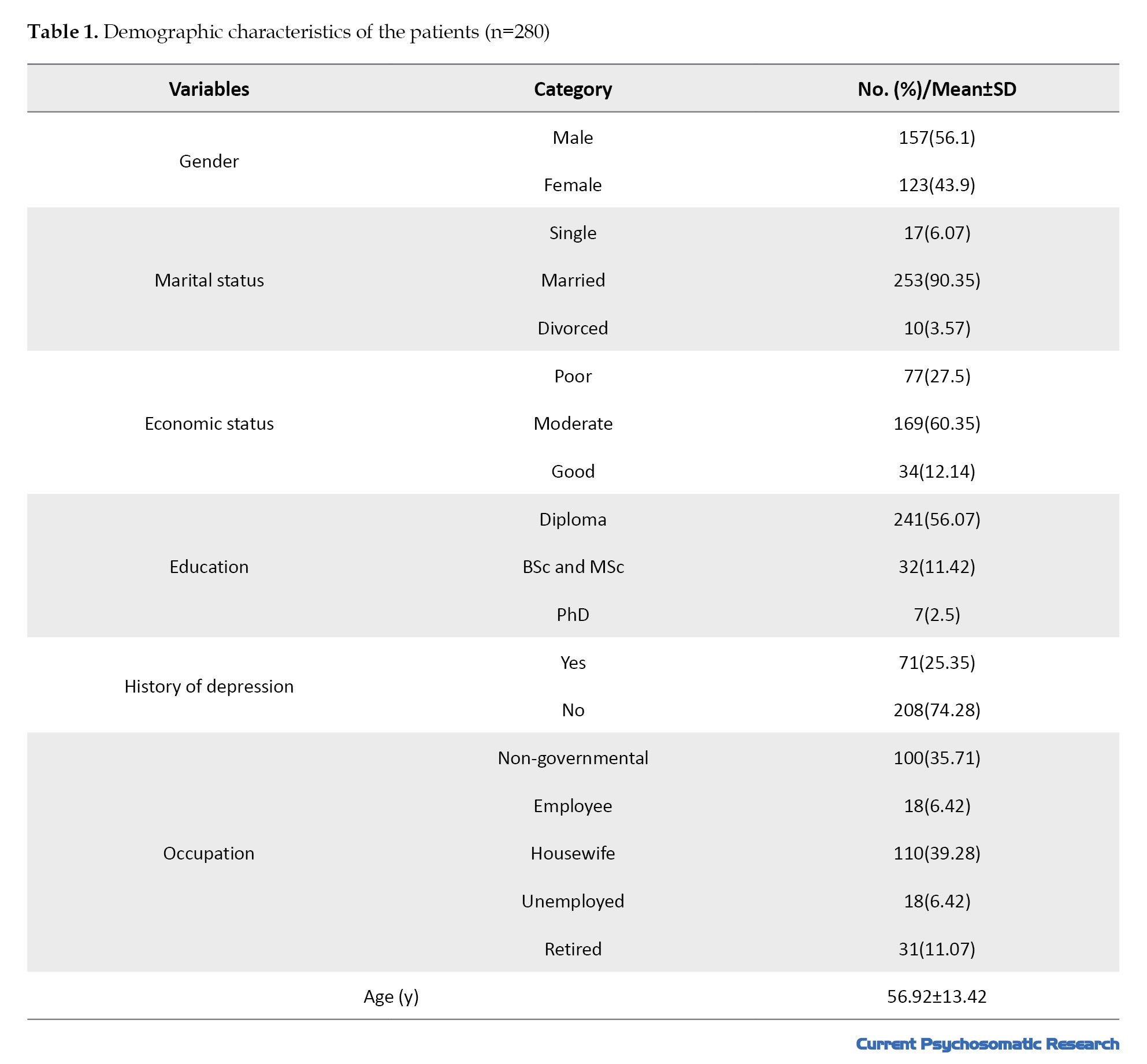
The mean age of the participants was 56.92±13.42 years. Additionally, 35.90% were married, 56.1% were male, 60.35% had a moderate economic status and approximately 86.07% of patients held a diploma (Table 1).
The average religious coping score was 34.21±5.20 and the mean body image concern score was 30.87±13.49.
Table 2 displays the outcomes of simple linear regression investigating the relationship between age, gender, education level, marital status, history of depression, economic status, occupation and religious coping with concerns regarding body image.
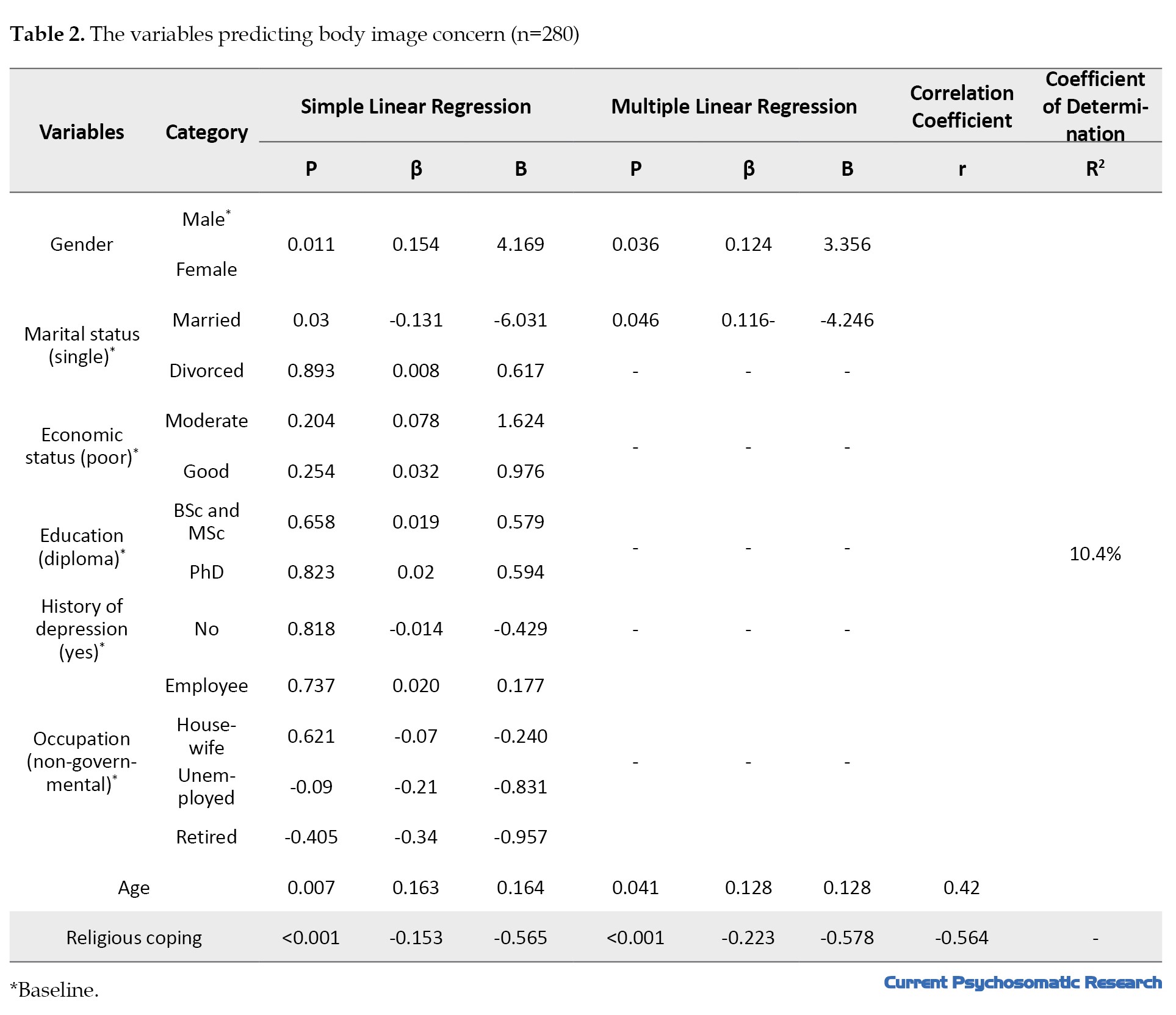
Age (B=0.164, β=0.163, P=0.007), gender (B=4.169, β=0.154, P=0.011), marital status (married) (B=-6.031, β=-0.131, P=0.03) and religious coping (B=-0.565, β=-0.153, P<0.001) emerged as predictors of body image concerns. Conversely, no significant associations were found between marital status (divorced), education level, economic status, history of depression and occupation with body image concerns (as per the ANOVA results). Additionally, Table 2 outlines the findings of multiple linear regression. Upon inclusion of age (B=-0.128, β=0.128, P=0.041), gender (B=3.356, β=0.124, P=0.036), marital status (married) (B=-4.246, β=-0.116, P=0.046) and religious coping (B=-0.578, β=-0.223, P<0.001), the multiple regression model achieved significance. This model accounted for 10.4% of the predictors of body image concerns among hemodialysis patients.
Discussion
The objective of this study was to explore the correlation between religious coping and body image among patients with CKD undergoing hemodialysis. The findings indicated that variables such as economic status, education level, history of depression, and occupation did not exhibit a significant relationship with body image concerns. Conversely, factors like female gender and age (associated with increased body image concerns), marital status (being married) and religious coping (linked to reduced body image concerns) emerged as predictors of body image concerns in hemodialysis patients. This outcome aligns with prior research [20-24]; however, it contrasts with a study conducted by Chen on factors influencing body image, where individuals with higher education displayed lower body image concerns [25]. This discrepancy could be attributed to heightened health awareness, elevated expectations, increased sensitivity to physical alterations and adherence to societal norms among individuals with higher education levels [15]. In the current study, no significant correlation was observed between education and body image, consistent with the findings of Sharif Nia et al. indicating that education does not impact body image [9]. As a multidimensional construct, body image encompasses perceptions, thoughts, emotions, and behaviors associated with the body’s appearance, capabilities and functions.
Consequently, alterations in physical, mental and social functions can influence one’s body image [26]. The findings also revealed that women, married individuals, and older people exhibited higher body image concerns. Numerous studies on the impact of gender on body image affirm that women undergoing hemodialysis may harbor greater apprehensions about their body image compared to men [27, 28]. Moreover, Sadeghian et al.’s results, which examined hemodialysis patients, corroborate our conclusions [29].
Our results indicate that married hemodialysis patients are less concerned about their body image than single patients. This observation can be analyzed from social support and psychological security perspectives. Married patients tend to receive more emotional and psychological backing due to their partners. This support helps them better manage physical transformations and challenges stemming from the illness [30]. A partner who offers love and attention can instill a sense of worth and acceptance in patients, even amidst physical difficulties. Social and emotional support can enhance the QoL for individuals with chronic conditions and alleviate concerns related to body image [31, 32].
Conversely, single, divorced and widowed patients may encounter heightened emotional and psychological challenges stemming from a lack of emotional and social support, often feeling isolated and uncared for [33]. Such sentiments can precipitate anxiety, depression, and heightened concerns regarding body image. These individuals might perceive themselves as less accepted due to physical issues, potentially undermining their self-assurance and body contentment [33, 34]. Studies indicate that feelings of loneliness and social isolation can detrimentally impact mental well-being and one’s body image perception [35]. Hence, marital status plays a pivotal role in diminishing concerns and anxieties about body image among hemodialysis patients. On the other hand, the absence of a significant relationship between economic status and body image concerns can be rationalized by the notion that hemodialysis patients may gradually acclimate to their condition and develop a form of adaptation to the illness. This adjustment process could mitigate the influence of economic status on body image concerns [9, 36].
The current study’s findings align with previous research outcomes regarding the capacity to predict body image concerns through religious coping among individuals undergoing hemodialysis treatment [37-42]. Hence, a correlation exists between religious coping and body image concerns, suggesting that enhancing religious coping mechanisms can mitigate body image concerns in individuals receiving hemodialysis treatment. Individuals with a strong bond with God and heightened spirituality levels tend to exhibit lower levels of body image concerns. Akrawi et al. similarly demonstrated that robust religious convictions correlate with reduced body image concerns [43]. Conversely, religion (religious beliefs) and spirituality (connection with a higher being) can enhance body image perceptions. People with religious beliefs usually have better body image and body satisfaction due to attributing life events to spiritual concepts [44]. In addition, religious people believe that the body is God’s creation and surrounds him. This belief reduces the importance of appearance, emphasizes the unconditional acceptance of the body, and causes people to pay limited attention to the opinions of others about their appearance [40, 45]. Addressing the religious and spiritual needs of hemodialysis patients can be a valuable component of comprehensive and patient-centered care. Helping patients use religious coping mechanisms may increase their ability to adapt to the physical challenges of illness and maintain a more positive self-perception. Therefore, the promotion of religious coping reduces the concern about body image in people undergoing hemodialysis treatment.
Individuals with religious beliefs typically experience enhanced body image and body satisfaction by attributing life events to spiritual concepts [44]. Moreover, a religious and spiritual perspective views the body as a creation of God and a vessel for divine presence. This viewpoint diminishes the significance of physical appearance, underscores the unconditional acceptance of the body, and encourages individuals to place limited emphasis on others’ opinions regarding their appearance [40, 45]. Addressing the religious and spiritual needs of hemodialysis patients can serve as a valuable component of comprehensive and patient-centered care. Assisting patients in utilizing religious coping strategies may enhance their capacity to adapt to the physical challenges of illness and foster a more positive self-perception. Therefore, promoting religious coping mechanisms can alleviate concerns about body image among individuals undergoing hemodialysis treatment.
As this study solely explored the correlation between religious coping and body image concerns among individuals undergoing hemodialysis in Iran, conducting a longitudinal study to assess how variations in religious coping over time impact body image and other psychological outcomes in hemodialysis patients or developing and evaluating the efficacy of tailored religious/spiritual support or counseling programs to enhance body image in hemodialysis patients, alongside examining the differing impacts of such interventions between genders, could prove beneficial in this domain. Conversely, research to probe how religious coping interrelates with other crucial psychosocial variables like self-esteem, depression, and QoL, as well as investigating specific religious/spiritual factors (such as beliefs, practices and social support) potentially linked to body image, appears to be highly significant and impactful.
Conclusion
The results of this study reveal that increased religious coping is associated with improved body image among hemodialysis patients. Specifically, individuals with higher levels of religious coping exhibited a more favorable body image. This correlation likely stems from the role of religion in bolstering self-acceptance, fostering an appreciation for body appearance, and aiding in the adjustment to physical changes induced by illness. Religion can serve as a source of support and spirituality for hemodialysis patients, assisting them in embracing and adapting to the physical transformations brought about by the disease. Hence, offering religious and spiritual interventions can enhance hemodialysis patients’ body image. Additionally, it appears essential to consider the religious and spiritual dimensions in the rehabilitation and care programs tailored for these patients.
Ethical Considerations
Compliance with ethical guidelines
This study stems from a research project (Code: 17740), that was approved by the Ethics Committee of Mazandaran University of Medical Sciences (Code: IR.MAZUMS.REC.1402.683). Written informed consent was obtained from all patients. The researchers visited the Shahrvand Dialysis Center, elucidating the study’s objectives to interested participants, who were then requested to complete the questionnaire during hemodialysis (post-connection to the machine). Throughout the questionnaire completion process, the researcher was present to provide necessary clarifications for accurate responses in case of any ambiguity. Before data collection and questionnaire completion, the physician and nurses were consulted regarding the patient’s clinical status, ensuring that patients had complete physical and mental well-being. Sampling procedures were conducted outside treatment sessions and meal times to prevent errors. Additionally, the authors are prepared to provide the raw data supporting the paper’s conclusions upon reasonable request.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data collection: Amir Hossein Goudarzian; Data analysis and editing: Hamid Sharif Nia; Writing the manuscript: Reza Fatehi, Poorya Nowrozi, Mohammad Hashem Gholampour, Alireza Ghanbari and Fatemeh Miraghai.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank all the patients who participated in this study; their cooperation was invaluable in advancing this research. The authors also express their gratitude to Mazandaran University of Medical Sciences for their support and approval of this project.
References
Chronic kidney disease (CKD) is a prevalent health concern that ultimately develops into end-stage renal disease (ESRD) [1]. In 2017, the global count of individuals with ESRD exceeded 850 million, with projections indicating that by 2040, it will emerge as a leading cause of mortality among individuals undergoing hemodialysis [2]. The prevalence of ESRD in the US, Europe and Iran has been documented at 1500, 800 and 360 cases per million, respectively. Notably, in Iran, the prevalence of this advanced chronic ailment notably surged in 2006 compared to 2000. Hemodialysis stands out as one of the most prevalent treatment modalities for ESRD [3]. Estimates suggest a surge of 5.4 million individuals in hemodialysis patients by 2030 [4].
Hemodialysis effectively enhances CKD management and elevates these patients’ quality of life (QoL) [5]. Despite advancements in hemodialysis that have bolstered the survival rates of ESRD patients, individuals with ESRD contend with various physical and psychosocial symptoms, and traditional treatments can disrupt their QoL [1, 6]. While hemodialysis treatment preserves the lives of those with ESRD, it does not avert the disease’s complications, anxiety, despair and similar challenges. Hence, the strategies patients employ to confront these obstacles hold significant importance. Religious coping is crucial for navigating stressful circumstances [1, 6].
Religious coping entails an individual’s ability to integrate religious beliefs and values into daily life and experiences. This capability assists individuals in effectively addressing life’s challenges and uncertainties, particularly through aligning with religious principles and faith in a higher power, enhancing their productivity, and fostering a sense of psychological security [7]. It can serve as a criterion for improving an individual’s mental and spiritual well-being and fortifying their connection with spirituality and religion [7, 8]. Despite the impact of dialysis on both the patient and their family, there exists a necessity for an efficient strategy to diminish dependency, uphold self-esteem, and alleviate concerns regarding body image. Research indicates that healthcare providers often lack sufficient knowledge regarding body image [9]. These patients encounter lifestyle constraints due to their condition, which can influence social interactions, beliefs, and their sense of control. Body image, integral to personal identity formation, significantly affects how patients perceive themselves and individuals undergoing hemodialysis confront physical and psychological challenges like fear, anxiety, and despair. Moreover, they encounter difficulties accepting changes in their physical appearance, which can result in concerns about body image [10].
Body image distortion is distressing and can lead to adverse consequences. A negative body image can impact physical and mental well-being, self-esteem, mood, competence and social and occupational performance [11]. Religion holds significant influence in the lives of numerous individuals [12]. Over recent years, the correlation between religiosity and psychosocial coping has garnered attention in the healthcare domain. It appears that religious or spiritual aspects, broadly defined, play a crucial role in the adaptation process for many patients, particularly those confronting severe illnesses like CKD patients undergoing hemodialysis [13].
With the escalating number of patients undergoing hemodialysis and encountering specific challenges like chronic treatment, lifestyle constraints and substantial alterations in body image and functionality, fostering a positive body image can significantly enhance the QoL for these individuals. Studies indicate a heightened prevalence of body image disorders among hemodialysis patients, with levels notably surpassing those in the general population [13-15]. Effective strategies to address negative body image include encouraging patients to concentrate on positive attributes beyond their physical appearance, such as their values and relationships [14], engaging in suitable physical activities, utilizing cosmetics and employing religious coping mechanisms [9]. Leveraging religious support and coping strategies can prove more efficacious in addressing the psychological and emotional hurdles faced by hemodialysis patients compared to alternative approaches [16, 17].
Given the elevated prevalence of body image disorders among hemodialysis patients and the significant influence of religion in Iran, understanding the correlation between religious coping and body image in hemodialysis patients holds paramount importance in addressing their mental well-being challenges. Understanding the impact of religious coping on shaping the body image of hemodialysis patients is crucial for various reasons. Firstly, it can offer insights into the psychological and emotional effects of religious coping on body image perception, which is vital for addressing the overall well-being of these individuals. Furthermore, such investigations can help in crafting tailored interventions and support mechanisms that consider the religious and spiritual aspects of coping with body image issues within this demographic. Similarly, exploring this connection can contribute to a broader comprehension of the intricate interplay between religious coping, mental health, and physical well-being within the realm of chronic illness and medical care. Hence, conducting a study on the relationship between religious coping and body image in hemodialysis patients becomes imperative to bridge this knowledge gap and advance comprehensive care and assistance for these individuals.
Materials and Methods
Design and participants
The study design employed in this research was descriptive-correlational and was carried out from March to June 2023. The sample size was 280 individuals using G*Power software version 3.1.7, considering the Equation 1:
The study population comprised patients diagnosed with ESRD undergoing hemodialysis, selected from the Shahrvand Dialysis Center in Sari City, Iran, using the available sampling method. The inclusion criteria encompassed the ability to read and write and the age of 18 years and above. The exclusion criteria involved alcohol addiction, mental, emotional and verbal issues, reduced consciousness levels, and digestive ailments like gastric ulcers, gastric reflux, and congestive heart failure [9].
Research tools
Data collection instruments comprised a demographic checklist (including age, gender, depression, marital status, education level, economic status and occupation), Littleton’s body image concern inventory (BICI) and the religious coping questionnaire (RCOPE) developed by Pargament et al. [19]
Body image concern inventory (BICI)
The BICI questionnaire comprises 19 items initially developed and validated by Littleton et al. (2005), with confirmed validity and reliability [18]. The BICI assesses an individual’s discontent, apprehension, and embarrassment concerning their appearance, including behaviors like checking and concealing perceived flaws and the extent to which fear about one’s appearance hampers social functioning. Responses are rated on a 5-point Likert scale ranging from never=1 to always=5. The total scale score ranges from 19 to 95, with higher scores indicating increased dissatisfaction with one’s body image or appearance [18]. In this study, the questionnaire’s reliability was assessed using the Cronbach α coefficient, yielding a value of 0.943.
Religious coping questionnaire (RCOPE)
The investigation into religious coping methods utilized the short form of RCOPE, a tool with confirmed validity and reliability. This standardized instrument comprises 14 items designed by Pargament et al. [19] to assess positive and negative religious coping strategies. Each scale, positive and negative, consists of seven religious coping items. RCOPE responses are rated on a 4-point Likert scale ranging from “not at all” to “very much.” Positive religious coping involves confronting adverse life events, and an individual embraces these events by deriving positive insights and changes linked to divine assistance [19]. In this study, the questionnaire’s reliability was assessed using Cronbach’s α, resulting in a value of 0.707.
Data analysis
The obtained data were analyzed using SPSS software, version 26. The normal distribution of continuous quantitative data was assessed using the Kolmogorov-Smirnov test. Simple linear regression was employed to examine the relationship between religious coping variables and body image among hemodialysis patients. Furthermore, variables that exhibited significance in simple linear regression were concurrently assessed in multiple linear regression. A significance level of <0.05 was considered for all tests.
Results
Demographic characteristics
The mean age of the participants was 56.92±13.42 years. Additionally, 35.90% were married, 56.1% were male, 60.35% had a moderate economic status and approximately 86.07% of patients held a diploma (Table 1).
The average religious coping score was 34.21±5.20 and the mean body image concern score was 30.87±13.49.
Table 2 displays the outcomes of simple linear regression investigating the relationship between age, gender, education level, marital status, history of depression, economic status, occupation and religious coping with concerns regarding body image.
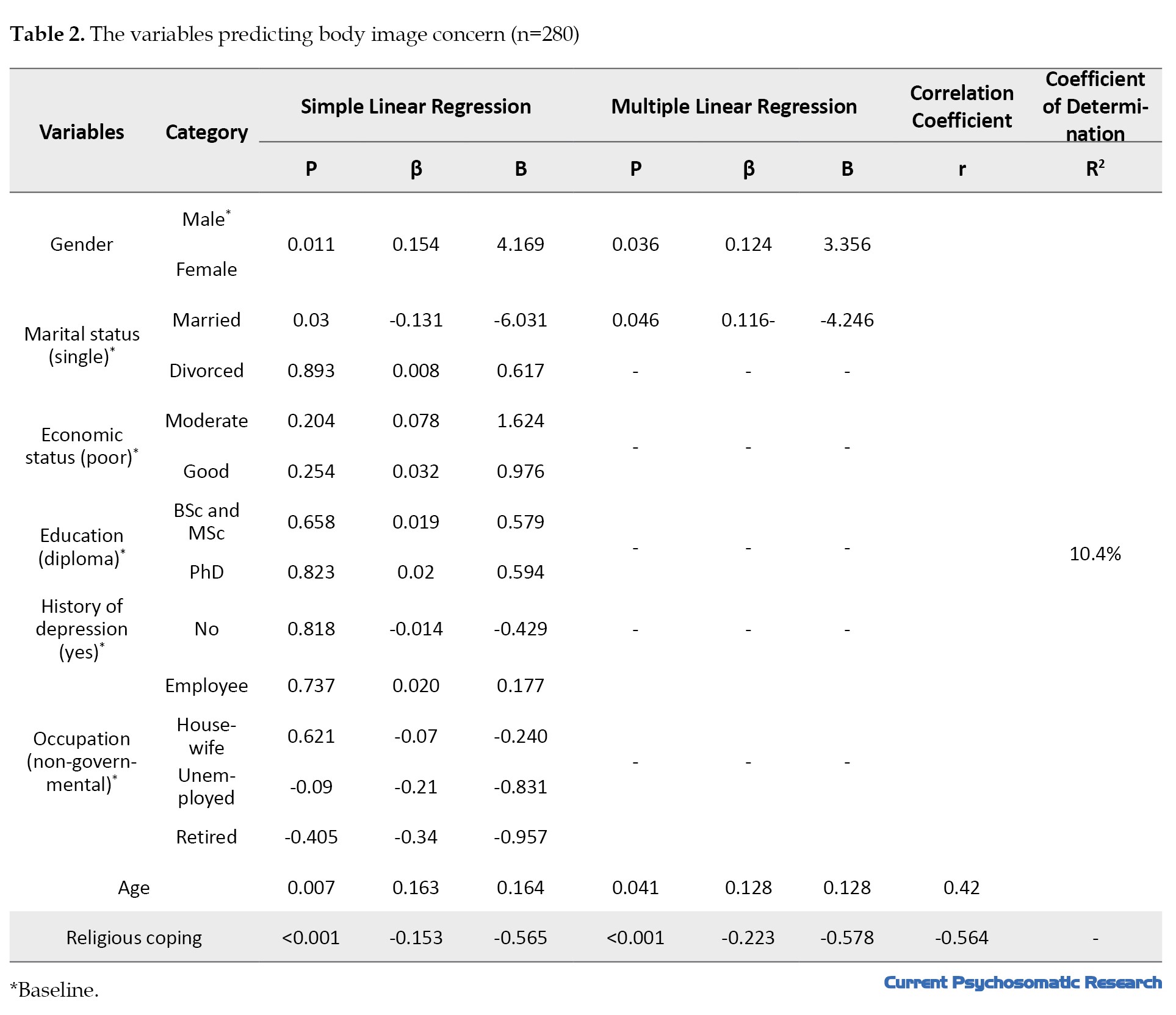
Age (B=0.164, β=0.163, P=0.007), gender (B=4.169, β=0.154, P=0.011), marital status (married) (B=-6.031, β=-0.131, P=0.03) and religious coping (B=-0.565, β=-0.153, P<0.001) emerged as predictors of body image concerns. Conversely, no significant associations were found between marital status (divorced), education level, economic status, history of depression and occupation with body image concerns (as per the ANOVA results). Additionally, Table 2 outlines the findings of multiple linear regression. Upon inclusion of age (B=-0.128, β=0.128, P=0.041), gender (B=3.356, β=0.124, P=0.036), marital status (married) (B=-4.246, β=-0.116, P=0.046) and religious coping (B=-0.578, β=-0.223, P<0.001), the multiple regression model achieved significance. This model accounted for 10.4% of the predictors of body image concerns among hemodialysis patients.
Discussion
The objective of this study was to explore the correlation between religious coping and body image among patients with CKD undergoing hemodialysis. The findings indicated that variables such as economic status, education level, history of depression, and occupation did not exhibit a significant relationship with body image concerns. Conversely, factors like female gender and age (associated with increased body image concerns), marital status (being married) and religious coping (linked to reduced body image concerns) emerged as predictors of body image concerns in hemodialysis patients. This outcome aligns with prior research [20-24]; however, it contrasts with a study conducted by Chen on factors influencing body image, where individuals with higher education displayed lower body image concerns [25]. This discrepancy could be attributed to heightened health awareness, elevated expectations, increased sensitivity to physical alterations and adherence to societal norms among individuals with higher education levels [15]. In the current study, no significant correlation was observed between education and body image, consistent with the findings of Sharif Nia et al. indicating that education does not impact body image [9]. As a multidimensional construct, body image encompasses perceptions, thoughts, emotions, and behaviors associated with the body’s appearance, capabilities and functions.
Consequently, alterations in physical, mental and social functions can influence one’s body image [26]. The findings also revealed that women, married individuals, and older people exhibited higher body image concerns. Numerous studies on the impact of gender on body image affirm that women undergoing hemodialysis may harbor greater apprehensions about their body image compared to men [27, 28]. Moreover, Sadeghian et al.’s results, which examined hemodialysis patients, corroborate our conclusions [29].
Our results indicate that married hemodialysis patients are less concerned about their body image than single patients. This observation can be analyzed from social support and psychological security perspectives. Married patients tend to receive more emotional and psychological backing due to their partners. This support helps them better manage physical transformations and challenges stemming from the illness [30]. A partner who offers love and attention can instill a sense of worth and acceptance in patients, even amidst physical difficulties. Social and emotional support can enhance the QoL for individuals with chronic conditions and alleviate concerns related to body image [31, 32].
Conversely, single, divorced and widowed patients may encounter heightened emotional and psychological challenges stemming from a lack of emotional and social support, often feeling isolated and uncared for [33]. Such sentiments can precipitate anxiety, depression, and heightened concerns regarding body image. These individuals might perceive themselves as less accepted due to physical issues, potentially undermining their self-assurance and body contentment [33, 34]. Studies indicate that feelings of loneliness and social isolation can detrimentally impact mental well-being and one’s body image perception [35]. Hence, marital status plays a pivotal role in diminishing concerns and anxieties about body image among hemodialysis patients. On the other hand, the absence of a significant relationship between economic status and body image concerns can be rationalized by the notion that hemodialysis patients may gradually acclimate to their condition and develop a form of adaptation to the illness. This adjustment process could mitigate the influence of economic status on body image concerns [9, 36].
The current study’s findings align with previous research outcomes regarding the capacity to predict body image concerns through religious coping among individuals undergoing hemodialysis treatment [37-42]. Hence, a correlation exists between religious coping and body image concerns, suggesting that enhancing religious coping mechanisms can mitigate body image concerns in individuals receiving hemodialysis treatment. Individuals with a strong bond with God and heightened spirituality levels tend to exhibit lower levels of body image concerns. Akrawi et al. similarly demonstrated that robust religious convictions correlate with reduced body image concerns [43]. Conversely, religion (religious beliefs) and spirituality (connection with a higher being) can enhance body image perceptions. People with religious beliefs usually have better body image and body satisfaction due to attributing life events to spiritual concepts [44]. In addition, religious people believe that the body is God’s creation and surrounds him. This belief reduces the importance of appearance, emphasizes the unconditional acceptance of the body, and causes people to pay limited attention to the opinions of others about their appearance [40, 45]. Addressing the religious and spiritual needs of hemodialysis patients can be a valuable component of comprehensive and patient-centered care. Helping patients use religious coping mechanisms may increase their ability to adapt to the physical challenges of illness and maintain a more positive self-perception. Therefore, the promotion of religious coping reduces the concern about body image in people undergoing hemodialysis treatment.
Individuals with religious beliefs typically experience enhanced body image and body satisfaction by attributing life events to spiritual concepts [44]. Moreover, a religious and spiritual perspective views the body as a creation of God and a vessel for divine presence. This viewpoint diminishes the significance of physical appearance, underscores the unconditional acceptance of the body, and encourages individuals to place limited emphasis on others’ opinions regarding their appearance [40, 45]. Addressing the religious and spiritual needs of hemodialysis patients can serve as a valuable component of comprehensive and patient-centered care. Assisting patients in utilizing religious coping strategies may enhance their capacity to adapt to the physical challenges of illness and foster a more positive self-perception. Therefore, promoting religious coping mechanisms can alleviate concerns about body image among individuals undergoing hemodialysis treatment.
As this study solely explored the correlation between religious coping and body image concerns among individuals undergoing hemodialysis in Iran, conducting a longitudinal study to assess how variations in religious coping over time impact body image and other psychological outcomes in hemodialysis patients or developing and evaluating the efficacy of tailored religious/spiritual support or counseling programs to enhance body image in hemodialysis patients, alongside examining the differing impacts of such interventions between genders, could prove beneficial in this domain. Conversely, research to probe how religious coping interrelates with other crucial psychosocial variables like self-esteem, depression, and QoL, as well as investigating specific religious/spiritual factors (such as beliefs, practices and social support) potentially linked to body image, appears to be highly significant and impactful.
Conclusion
The results of this study reveal that increased religious coping is associated with improved body image among hemodialysis patients. Specifically, individuals with higher levels of religious coping exhibited a more favorable body image. This correlation likely stems from the role of religion in bolstering self-acceptance, fostering an appreciation for body appearance, and aiding in the adjustment to physical changes induced by illness. Religion can serve as a source of support and spirituality for hemodialysis patients, assisting them in embracing and adapting to the physical transformations brought about by the disease. Hence, offering religious and spiritual interventions can enhance hemodialysis patients’ body image. Additionally, it appears essential to consider the religious and spiritual dimensions in the rehabilitation and care programs tailored for these patients.
Ethical Considerations
Compliance with ethical guidelines
This study stems from a research project (Code: 17740), that was approved by the Ethics Committee of Mazandaran University of Medical Sciences (Code: IR.MAZUMS.REC.1402.683). Written informed consent was obtained from all patients. The researchers visited the Shahrvand Dialysis Center, elucidating the study’s objectives to interested participants, who were then requested to complete the questionnaire during hemodialysis (post-connection to the machine). Throughout the questionnaire completion process, the researcher was present to provide necessary clarifications for accurate responses in case of any ambiguity. Before data collection and questionnaire completion, the physician and nurses were consulted regarding the patient’s clinical status, ensuring that patients had complete physical and mental well-being. Sampling procedures were conducted outside treatment sessions and meal times to prevent errors. Additionally, the authors are prepared to provide the raw data supporting the paper’s conclusions upon reasonable request.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data collection: Amir Hossein Goudarzian; Data analysis and editing: Hamid Sharif Nia; Writing the manuscript: Reza Fatehi, Poorya Nowrozi, Mohammad Hashem Gholampour, Alireza Ghanbari and Fatemeh Miraghai.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank all the patients who participated in this study; their cooperation was invaluable in advancing this research. The authors also express their gratitude to Mazandaran University of Medical Sciences for their support and approval of this project.
References
- Taheri-Kharameh Z, Zamanian H, Montazeri A, Asgarian A, Esbiri R. Negative religious coping, positive religious coping, and quality of life among hemodialysis patients. Nephrourol Mon. 2016; 8(6):e38009. [DOI:10.5812/numonthly.38009] [PMID]
- Bello AK, Okpechi IG, Osman MA, Cho Y, Htay H, Jha V, et al. Epidemiology of haemodialysis outcomes. Nat Rev Nephrol. 2022; 18(6):378-95. [DOI:10.1038/s41581-022-00542-7] [PMID]
- Ahmadi M, Mashoufi M, Barzegari S, Kebar SM, Hoseininia S, Hassanlouei B, et al. Geographical accessibility to the hemodialysis centers in Ardabil, Iran. J Nephropharmacol. 2022; 11(2):e14. [DOI:10.34172/npj.2022.14]
- Campo S, Lacquaniti A, Trombetta D, Smeriglio A, Monardo P. Immune system dysfunction and inflammation in hemodialysis patients: Two sides of the same coin. J Clin Med. 2022; 11(13):3759. [DOI:10.3390/jcm11133759] [PMID]
- Monardo P, Lacquaniti A, Campo S, Bucca M, Casuscelli di Tocco T, Rovito S, et al. Updates on hemodialysis techniques with a common denominator: The personalization of the dialytic therapy. Semin Dial. 2021; 34(3):183-95. [DOI:10.1111/sdi.12956] [PMID]
- Bayoumi M, Al Harbi A, Al Suwaida A, Al Ghonaim M, Al Wakeel J, Mishkiry A. Predictors of quality of life in hemodialysis patients. Saudi J Kidney Dis Transpl. 2013; 24(2):254-9. [DOI:10.4103/1319-2442.109566] [PMID]
- Szcześniak M, Kroplewski Z, Szałachowski R. The mediating effect of coping strategies on religious/spiritual struggles and life satisfaction. Religions. 2020; 11(4):195. [DOI:10.3390/rel11040195]
- Aloush V, Gurevich-Shapiro A, Hazan E, Furer V, Elkayam O, Ablin JN. Relationship between religiosity, spirituality and physical and mental outcomes in fibromyalgia patients. Clin Exp Rheumatol. 2021; 39(3):48-53. [DOI:10.55563/clinexprheumatol/fcxigf] [PMID]
- Sharif Nia H, Kohestani D, Froelicher ES, Ibrahim FM, Ibrahim MM, Bayat Shahparast F, et al. The relationship between self-care behavior and concerns about body image in patients undergoing hemodialysis in Iran. Front Public Health. 2022; 10:825415. [DOI:10.3389/fpubh.2022.825415] [PMID]
- Urmila K, Wulandari NPD. The relationship between the long-time undergoing hemodialysis with self concept in chronic kidney disease (CKD) stadium III patients. J Ilmiah Ilmu Keperawatan Indonesia. 2021; 11(03):102-9. [DOI:10.33221/jiiki.v11i03.993]
- Hosseini SA, Padhy RK. Body image distortion. Treasure Island: StatPearls Publishing; 2024. [Link]
- Ano GG, Vasconcelles EB. Religious coping and psychological adjustment to stress: a meta-analysis. J Clin Psychol. 2005; 61(4):461-80. [DOI:10.1002/jclp.20049] [PMID]
- Pilger C, Caldeira S, Rodrigues RAP, Carvalho ECd, Kusumota L. Spiritual well-being, religious/spiritual coping and quality of life among the elderly undergoing hemodialysis: A correlational study. J Religi Spirit Aging. 2021; 33(1):2-15. [DOI:10.1080/15528030.2020.1824848]
- Biçer S, Demir G. Determination of body image perception and life satisfaction in patients undergoing hemodialysis. J Novel Physiother Rehabil. 2020; 4(2):016-21. [DOI:10.29328/journal.jnpr.1001032]
- Marki E, Moisoglou I, Aggelidou S, Malliarou M, Tsaras K, Papathanasiou IV. Body image, emotional intelligence and quality of life in peritoneal dialysis patients. AIMS Public Health. 2023; 10(3):698-709. [DOI:10.3934/publichealth.2023048] [PMID]
- Dewi IP, Widiyanti AT. Qur’anic therapy (Islamic bibliotherapy) to improve religious coping in hemodialysis patient. Media Keperawatan Indonesia. 2018; 1(3):12-7. [DOI:10.26714/mki.1.3.2018.12-17]
- Santos PR, Capote Júnior JRFG, Cavalcante Filho JRM, Ferreira TP, Dos Santos Filho JNG, da Silva Oliveira S. Religious coping methods predict depression and quality of life among end-stage renal disease patients undergoing hemodialysis: A cross-sectional study. BMC Nephrol. 2017; 18(1):197.[DOI:10.1186/s12882-017-0619-1] [PMID]
- Littleton H, Breitkopf CR. The body image concern inventory: Validation in a multiethnic sample and initial development of a Spanish language version. Body Image. 2008; 5(4):381-8. [DOI:10.1016/j.bodyim.2008.06.004] [PMID]
- Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: Development and initial validation of the RCOPE. J Clin Psychol. 2000; 56(4):519-43. [Link]
- Nia HS, Mousazadeh N, Shahparast FB, Kohestani D, Goudarzian AH. [Relationship between self-care behavior and body image concerns in hemodialysis patients in Sari, Iran: The mediating role of religious coping (Persian)]. Relig Health. 2022; 10(1):55-64. [Link]
- Springs CB. Relationship between religion and body image perception among a sample of African American Women [doctoral dissertation]. Washington: Walden University; 2012. [Link]
- Ackard DM, Kearney-Cooke A, Peterson CB. Effect of body image and self-image on women's sexual behaviors. Int J Eat Disord. 2000; 28(4):422-9. [DOI:10.1002/1098-108X(200012)28:43.0.CO;2-1] [PMID]
- Pujols Y, Seal BN, Meston CM. The association between sexual satisfaction and body image in women. J Sex Med. 2010; 7(2 Pt 2):905-16. [DOI:10.1111/j.1743-6109.2009.01604.x] [PMID]
- Davidson D, Kelly H, Misiunaite I, Hilvert E. Body image and life satisfaction in Amish, Catholic, and non-religious women. J Amish Plain Anabaptist Stud. 2018; 6(2):174-91. [DOI:10.18061/1811/87096]
- Chen SL. The importance of body image in clinical practice. Hu Li Za Zhi. 2019; 66(5):4-5. [DOI:10.6224/JN.201910_66(5).01]
- Lewis-Smith H, Diedrichs PC, Harcourt D. A pilot study of a body image intervention for breast cancer survivors. Body Image. 2018; 27:21-31. [DOI:10.1016/j.bodyim.2018.08.006] [PMID]
- Murnen S, Don B. Body image and gender roles. Encyclopedia Body Image Human Appearance. 2012; 1:128-34. [DOI:10.1016/B978-0-12-384925-0.00019-5]
- Wu T, Zheng Y. Effect of sexual esteem and sexual communication on the relationship between body image and sexual function in Chinese heterosexual women. J Sex Med. 2021; 18(3):474-86. [DOI:10.1016/j.jsxm.2020.12.006] [PMID]
- Sadeghian J, Roudsari DM, Seyedfatemi N, Rafiei H. Body-image disturbance: A comparative study among haemodialysis and kidney transplant patients. J Clin Diagn Res. 2016; 10(5):OC14-6. [DOI:10.7860/JCDR/2016/15699.7733] [PMID]
- Moreira H, Crespo C, Paredes T, Silva S, Canavarro MC, Dattilio FM. Marital relationship, body image and psychological quality of life among breast cancer patients: The moderating role of the disease’s phases. Contemp Fam Ther. 2011; 33:161-78. [DOI:10.1007/s10591-011-9149-3]
- Theodoritsi A, Aravantinou ME, Gravani V, Bourtsi E, Vasilopoulou C, Theofilou P, et al. Factors associated with the social support of hemodialysis patients. Iran J Public Health. 2016; 45(10):1261-9. [PMID] [PMCID]
- Tavsanli NG, Nehir S. Comparison of Body Image Perception and Social Functioning Among Patients with End-Stage Renal Failure and Patients with Chronic Renal Failure. Iranian Red Crescent Med J. 2018; 20(7)):e64071. [DOI:10.5812/ircmj.64071]
- Vaingankar JA, Abdin E, Chong SA, Shafie S, Sambasivam R, Zhang YJ, et al. The association of mental disorders with perceived social support, and the role of marital status: Results from a national cross-sectional survey. Arch Public Health. 2020; 78:108. [DOI:10.1186/s13690-020-00476-1] [PMID]
- Zhang D, Zheng W, Li K. The relationship between marital status and cognitive impairment in Chinese older adults: The multiple mediating effects of social support and depression. BMC Geriatr. 2024; 24(1):367. [DOI:10.1186/s12877-024-04975-6] [PMID]
- Bellapigna CR. Need for structure, loneliness, social media use, and body image as predictors of mental health symptoms in the context of COVID-19. Galloway Township: Stockton University; 2021. [Link]
- Hassan RM, Mohamed HS, Rahman AA, Khalifa AM. Relation between therapeutic compliance and functional status of patients undergoing hemodialysis. Am J Nurs. 2020; 8(6):632-40. [Link]
- Inman M, Iceberg E, McKeel L. Do religious affirmations, religious commitments, or general commitments mitigate the negative effects of exposure to thin ideals? J Sci Study Relig. 2014; 53(1):38-55. [DOI:10.1111/jssr.12089]
- Boisvert JA, Harrell WA. Ethnicity and spirituality as risk factors for eating disorder symptomatology in men. Int J Men's Health. 2012; 11(1):36. [DOI:10.3149/jmh.1101.36]
- Boisvert JA, Harrell WA. The impact of spirituality on eating disorder symptomatology in ethnically diverse Canadian women. Int J Soc Psychiatry. 2013; 59(8):729-38. [DOI:10.1177/0020764012453816] [PMID]
- Tiggemann M, Hage K. Religion and spirituality: Pathways to positive body image. Body Image. 2019; 28:135-41. [DOI:10.1016/j.bodyim.2019.01.004] [PMID]
- Kusina JR, Exline JJ. Perceived attachment to God relates to body appreciation: mediating roles of self-compassion, sanctification of the body, and contingencies of self-worth. Ment Health, Relig Cult. 2021; 24(10):1050-71. [DOI:10.1080/13674676.2021.1995345]
- Mitton A. Exploring the Relationship between spiritual disciplines and body image, moderated by attachment to god and religious views of the body [doctoral dissertation]. La Mirada: Biola University; 2021. [Link]
- Akrawi D, Bartrop R, Potter U, Touyz S. Religiosity, spirituality in relation to disordered eating and body image concerns: A systematic review. J Eat Disord. 2015; 3:29. [DOI:10.1186/s40337-015-0064-0] [PMID]
- Goyal NG, Ip EH, Salsman JM, Avis NE. Spirituality and physical health status: A longitudinal examination of reciprocal effects in breast cancer survivors. Support Care Cancer. 2019; 27(6):2229-35. [DOI:10.1007/s00520-018-4494-5] [PMID]
- Sharif Nia H, Firouzbakht M, Rekabpour SJ, Nabavian M, Nikpour M. The psychometric properties of the Persian version of the body image after breast Cancer questionnaire: A second-order confirmatory factor analysis. Curr Psychol. 2023; 42(5):3924-34. [DOI:10.1007/s12144-021-01741-4]
Type of Study: Research |
Subject:
Nephrology
Received: 2023/08/19 | Accepted: 2023/11/13 | Published: 2024/01/1
Received: 2023/08/19 | Accepted: 2023/11/13 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




